Lithium toxicity
Lithium is commonly used to treat bipolar, for your toxicology encounter it will come in two varieties, either an acute overdose or chronic toxicity and it is important to distinguish the two (examiners love this question).
Lithium is a metal and like most metals in an acute ingestion it causes nausea, vomiting, diarrhoea and abdominal pain. Provided there is no kidney impairment neurotoxicity will not develop. In contrast chronic lithium toxicity has time redistribute from the gastrointestinal tract to the intravascular space and finally into the CNS resulting in neurotoxicity.
Lithium also causes a low anion gap metabolic acidosis, only two other drugs do this; bromide and iodine (again an examiner’s favourite MCQ).
Toxic Mechanism:
Once absorbed lithium ions substitute for sodium and potassium ions and are thought to modulate intracellular secondary messengers and potentially neurotransmitter production and release (including serotonin hence its association with serotonin toxicity).
Toxicokinetics:
- Completely absorbed by six hours and peak concentration at four hours with standard release preparation.
- In overdose peak concentration could be delayed up to 12 hours with slow-release preparations.
- Lithium slowly re-distributions from the intravascular compartment to tissue compartments with a steady state volume of distribution 0.7 – 0.9 L/Kg.
- Excreted in the urine and clearance is dependent on glomerular filtration and reduced in water or sodium depleted states (the kidney mistakes the lithium for sodium and therefore there is increased sodium resorption).
- Elimination half-life is 24 hours at steady state.
Resuscitation:
- Hypotension: Give 10 – 20 ml/kg of IV crystalloid if dehydrated and severe GI symptoms are present.
- Coma and seizures are only present in chronic poisoning and are extremely rare. In an acute overdose if there is a coma or seizure then other causes or toxicants need to be considered.
Risk Assessment
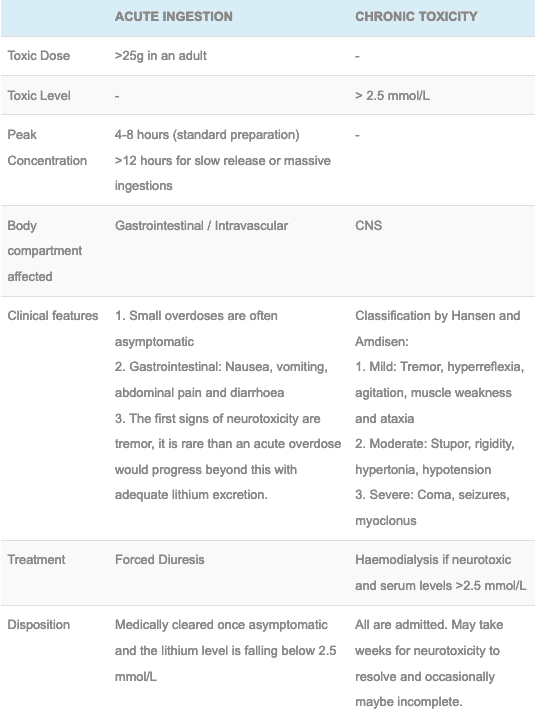
Table: Differences between an acute ingestion and chronic toxicity:
- Additional assessments regarding acute ingestion:
- If the patient has no renal impairment and acute ingestion of <25 g may cause some minor GI symptoms and is considered benign.
- >25 g can rarely lead to neurotoxicity, this can be avoided with good supportive care (avoid dehydration, sodium depletion or renal impairment).
- If the patient does have acute or chronic renal impairment, dehydration or sodium depletion lithium can redistribute to the CNS and cause neurotoxicity.
- If patients present late with neurotoxicity they should be treated as per chronic lithium toxicity.
- Children: rarely ingest enough to cause toxicity therefore do not require hospital assessment unless symptoms develop.
- Additional assessments regarding chronic ingestion:
- Patients chronically on lithium who take an acute overdose are not at increased risk of developing neurotoxicity and should be treated as per your acute overdose (assuming a normal renal function).
- Serum lithium concentrations correlate poorly with clinical features of toxicity.
- Consider lithium toxicity in anyone on therapy who has neurological signs or symptoms.
- A significantly reduced GCS or seizures in the context of lithium toxicity carries a significant risk of permanent neurological sequelae.
- Causes of toxicity:
- Diabetes insipidus and hypothyroidism (both precipitate toxicity and are also due to chronic lithium therapy).
- Dehydration
- Drug interaction (NSAIDs, ACE-i, Thiazide diuretics and topiramate)
- Sodium depletion
Supportive Care
- Attention to correcting any water or sodium deficits are required to maximise lithium excretion.
- In an acute overdose aim for >1ml/kg/hour of urine output is recommended.
- Cease any drug that may impair renal function
Investigations
- Screening: 12 lead ECG, BSL, Paracetamol level
- Specific:
- ECG: minor ST changes maybe seen.
- EUC to detect and monitor hyponatraemia and renal impairment.
- Serum lithium levels, useful to determine the overdose but also monitor progress in larger overdoses. It is not unusual to see levels >5 mmol/L occurring 4 – 8 hours post ingestion.
- Thyroid function (lithium can cause thyroid dysfunction, it inhibits thyroid hormone release).
Decontamination:
- Activated charcoal does not effectively absorb lithium.
Enhanced Elimination
- Lithium can be eliminated via haemodialysis, it is reserved for patients with established renal impairment or those with clinical features of neurotoxicity. For all other patients forced diuresis as described in supportive care is normally sufficient to avoid neurotoxicity.
- It should be considered in anyone with neurological dysfunction and a lithium level >2.5 mmol/L. Prolonged and repeated haemodialysis sessions may be required (it takes a long time for the lithium to redistribute out of the CNS and the concentration gradient needs to be maintained).
Antidote
- None available
Disposition
- Acute ingestion: patients with no evidence of neurotoxicity and a serum lithium level <2.5 mmol/L and falling can be medically cleared.
- Chronic poisoning: Always require admission, resolution of neurotoxicity may take weeks to resolve and occasionally may be incomplete.
References and Additional Resources:
Additional Resources:
- CCC – Lithium toxicity
- Tox Conundrum 048 – Lithium, Vomiting And Diarrhoea
- Metabolic Acidosis DDx
References:
- Hansen HE and Amdisen A. Lithium intoxication. Quarterly Journal of Medicine 1978: 47;123-144.
- Jaeger A et al. When should dialysis be performed in lithium poisoning? A kinetic study in 14 cases of lithium poisoning. Clinical Toxicology 1993; 31:429-427.
- Oakley P, Whyte IM and Carter GL. Lithium toxicity: an iatrogenic problem in susceptible individuals. Aust N Z J Psychiatry. 2001 Dec;35(6):833-40.

Toxicology Library
DRUGS and TOXICANTS
Dr Neil Long BMBS FACEM FRCEM FRCPC. Emergency Physician at Kelowna hospital, British Columbia. Loves the misery of alpine climbing and working in austere environments (namely tertiary trauma centres). Supporter of FOAMed, lifelong education and trying to find that elusive peak performance.

Hi do you have a reference for the toxic dose being 25g? I’m finding most resources state 4-5g being potentially fatal.
Thanks for the post
Ibrahim
Hi Ibrhim. The toxicology Handbook’s 3rd and 4th Editions (Murray and Little 2015) and (Armstrong and Pascu 2022) have the 25g dose quoted. This is only for acute ingestions in patients with a normal renal function. This doesn’t apply to chronic ingestions or those with renal impairment, which is why you may have sources with a more conservative number. I hope this helps.
Thank you. So this (“This is only for acute ingestions in patients with a normal renal function”) would mean a lithium naive patient?
Correct. In someone without a steady state of lithium and normal renal function, you’d expect them to pee all the lithium out before it could cause any neurotoxicity. Like all metal ingestions though you’d expect GI upset.