Mallet Finger
Definition
Rupture / avulsion of the distal extensor mechanism of the finger, resulting in an inability to extend the distal phalanx at the DIP joint.

Mechanism
- Forced flexion +/- axial loading of the DIP joint leading to tendon rupture or bony avulsion.
- Classically occurs in sports when a ball strikes the tip of an actively extended finger (catching injury) and forces the DIP joint into flexion.
- May also occur with a laceration over the dorsal surface of the DIP joint.
Anatomy
Two types of injury can occur:
- A tendinous mallet involves rupture of the extensor tendon proximal to the DIP joint.
- A bony mallet is an avulsion fracture of the dorsal aspect of the base of distal phalanx.

Clinical Assessment
LOOK
- Visible mallet deformity of the finger.
- An associated subungal haematoma may be present.
FEEL
- Maximally tender over the dorsal DIP joint.
MOVE
- Unable to actively extend DIP joint.
- Flexion of DIP joint is preserved but may be limited by pain.
Imaging
- Dedicated finger X-ray.
Radiological Assessment
- Look for evidence of an avulsion fracture on the dorsal aspect of the base of the distal phalanx (=bony mallet).
- If a fracture is present -> assess the % of articular surface involvement and whether volar subluxation of the distal phalanx is present.
- Surgery may be required if >30% of the articular surface is avulsed, or if the distal phalanx demonstrates volar subluxation.
- Clinical mallet deformity + no fractures seen on x-ray = tendinous mallet injury.

Clinical Cases
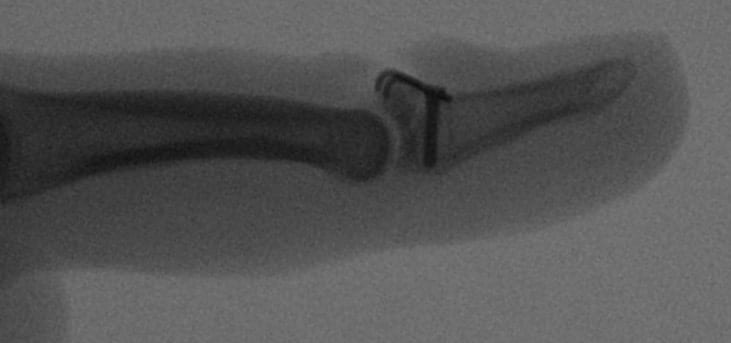
Case 1
A 32-year old female presented to ED with a mallet deformity to her right little finger after attempting to catch a ball that was thrown with some force by her brother.

Case 1 Interpretation
- There is a fracture through the dorsal aspect of the base of the distal phalanx, with around 30-40% involvement of the articular surface.
- Focusing on the soft tissue shadow, one can also appreciate the classic fixed flexion deformity of the DIP joint.
- This patient was placed in a dorsal finger splint and referred to a hand surgeon for ongoing care.
Case 2
A 31-year old male presented with mallet deformities to two of his fingers after sustaining a crush injury while lowering a washing machine to the ground.

Case 2 Interpretation
- The patient’s fingers are splinted in extension.
- There are avulsion fractures at the dorsal aspect of the bases of both ring and middle finger distal phalanges, with involvement of 40-50% of the articular surface of each.
- This patient went for ORIF of his middle finger (see images below). The ring finger was managed conservatively with splintage.

Case 3
A 31-year old female presented with a mallet deformity of her thumb after a friend collided with her outstretched hand.

Case 3 interpretation
- There is a displaced avulsion fracture arising from the dorsal aspect of the thumb distal phalanx. The avulsion fragment is <30% of the articular surface.
- This patient was splinted in extension and referred to a hand surgeon. They did not require operative management.
Case 4
A 12-year old girl presented to ED with a mallet deformity of her right ring finger after being struck on the finger tip by a netball.

Case 4 interpretation
Salter-Harris III fracture of the dorsal aspect of the distal phalanx, with an intra-articular avulsion fragment involving ~50% of the articular surface associated with widening of the dorsal portion of the growth plate.
Emergency Management
- Analgesia
- Splintage – Immobilise the DIP joint in full extension, leaving the PIP joint free. We prefer to use a dorsal aluminium (“Zimmer”) splint, trimmed to size with trauma scissors and secured with pink Elastoplast tape.

Disposition
- Refer all mallet injuries to a hand surgeon for follow up (usually within 7 days).
- Surgery may be required for fractures >30% of the articular surface or volar subluxation of the distal phalanx.
- Conservative management involves splintage for 6-12 weeks.
- Once the patient has seen a surgeon and the management approach is determined, they will also need follow up with a hand therapist for ongoing splintage and rehabilitation. The hand therapist will often change the patient to a customised (e.g. thermoplastic) splint for more sophisticated immobilisation.
Discharge Advice
- The DIP joint needs to be kept in extension at all times to avoid separation of the tendon and protracted healing time. The splint can be removed for cleaning, but it is essential to support the finger tip and keep the DIP straight during this process.
- It is important to follow up with a hand surgeon to determine the optimal management approach for each patient.
Pearls and Pitfalls
- Tendinous mallet injuries are slower to heal. The recommended period of splintage is 6-8 weeks for a bony mallet and 8-12 weeks for a tendinous mallet.
- Mallet injuries may lead to a chronic swan-neck deformity if treatment is delayed or splintage is inadequate.
Useful Links
- EMRAP – Paediatric Finger Tip Injury (Podcast)
- Radiopaedia – Mallet Finger (Radiology Education)
- RACGP – Assessment and Management of Common Hand Injuries (Review Article)
- Current Reviews in Musculoskeletal Medicine – A Review of Mallet Finger and Jersey Finger Injuries in the Athlete (Journal Article)
Authors
- Lilian Wong (ED Physiotherapy Practitioner, Sydney)
- Ed Burns (Emergency Physician, Sydney)
- Matt Lutze (ED Nurse Practitioner, Sydney)
[cite]
Trauma Library
Injury database
Emergency Physician in Prehospital and Retrieval Medicine in Sydney, Australia. He has a passion for ECG interpretation and medical education | ECG Library |
