Mirizzi syndrome
Mirizzi syndrome is an uncommon hepatobiliary disorder caused by extrinsic compression of the common hepatic duct (CHD) or common bile duct (CBD) by an impacted gallstone, typically lodged in the cystic duct or Hartmann’s pouch. This mechanical obstruction can progress to inflammatory erosion and fistula formation between the gallbladder and the bile duct or adjacent structures.
Clinically, patients often present with right upper quadrant pain, jaundice, fever, and signs consistent with acute or chronic cholecystitis. Diagnostic confusion with choledocholithiasis or cholangiocarcinoma is common, and preoperative recognition remains low, often leading to significant surgical morbidity.
Mirizzi syndrome is classically associated with longstanding gallstone disease, affecting approximately 0.1% of gallstone patients and seen in up to 1% of cholecystectomy specimens.
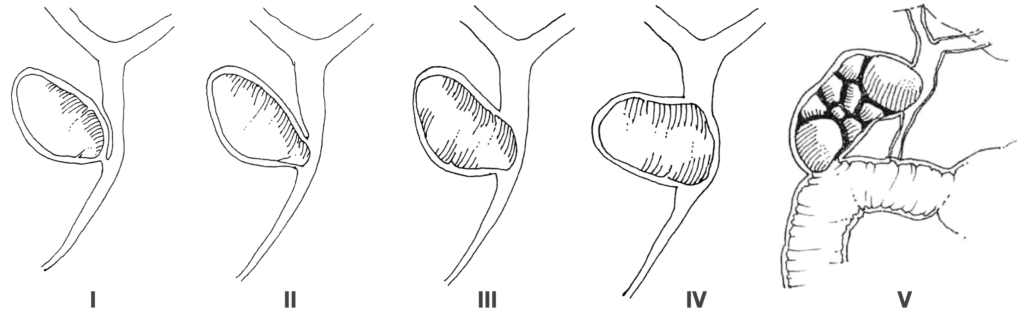
Current Classification (Beltrán modified Csendes classification)
- Type I: External compression of the common bile duct by a gallstone in the Hartmann’s pouch or cystic duct.
- Type II: Cholecystobiliary fistula involving < 1/3 of the CBD circumference.
- Type III: Fistula involving < 2/3 of the CBD.
- Type IV: Complete destruction of the CBD wall; whole circumference of bile duct
- Type Va: Types I–IV + cholecystoenteric fistula without gallstone ileus.
- Type Vb: Types I–IV + cholecystoenteric fistula with gallstone ileus.
Complications and Associations
A significant subset of patients may develop biliary-enteric fistulae, most commonly cholecystoduodenal. In Type Vb, these fistulae can lead to gallstone ileus, representing a complex and life-threatening complication. Other complications include:
- Recurrent cholangitis
- Biliary cirrhosis
- Iatrogenic bile duct injury (due to misidentification intraoperatively)
Diagnosis and Imaging
The condition is often missed preoperatively. Modalities such as MRCP, ERCP, and CT cholangiography are pivotal for pre-surgical identification:
- ERCP may reveal a characteristic smooth, right-concave stricture.
- MRCP can show a large stone in Hartmann’s pouch and intrahepatic biliary dilatation with tapering at the site of compression.
Summary Points:
- Rare complication of chronic cholelithiasis
- Results from external compression or erosion of bile duct
- Requires high index of suspicion in patients with obstructive jaundice and long-standing gallstones
- Pre-op diagnosis essential to avoid bile duct injury
- Multiple classification systems, with Csendes system most commonly used
- Surgical treatment varies with type — ranging from cholecystectomy to biliary reconstruction
History
1890 – Ludwig Courvoisier (1843-1918) in his analysis of biliary tract diseases, describes the topography and variants of the extrahepatic biliary tree, including anomalies.
1905 – Hans Kehr (1862-1916) publishes Die in meiner Klinik geübte Technik der Gallensteinoperationen, describing in detail the consequences of impacted gallstones in the cystic duct and infundibulum, including chronic inflammation, adhesions, and fistula formation. No direct mention of a hepatocystic duct compression syndrome, but Kehr is often cited (e.g., in Ruge 1908) for his detailed anatomical observations and operative cholangiographic findings relevant to the eventual Mirizzi construct.
1908 – Ernst Rüge (1878–1953) publishes Beitrage zur chirurgischen Anatomie der grossen Gallenwege with highly detailed illustrations of the surgical anatomy of the extrahepatic biliary tract. Though not clinical in focus, he describes variants in bile duct anatomy and their relation to lithiasis but does not propose a distinct syndrome. His work influences future interpretations of ductal compression and variants as pathophysiological entities.
1932 – Pablo Luis Mirizzi (1893-1964) was the first make a practical application for operative cholangiography. He publishes Cholangiografi durante las operaciones de las vias biliares and begins exploring the functional sphincteric mechanisms of the hepatic duct system. He hypothesizes a physiological sphincteric zone in the hepatic duct that regulates bile flow and protects against retrograde infection.
1940 – Mirizzi incorrectly introduces the concept of a “physiologic sphincter” in the common hepatic duct and discusses the presence of muscular fibres in a spiral or annular pattern. He begins to frame a functional model of biliary regulation with protective implications in disease.
1942 – Mirizzi publishes El sistema del hepático: Su fisiopatología and expands the functional-anatomical model. He suggests the hepatic duct’s contractile properties form a “hepatocystic sphincter”.
1948 – Mirizzi publishes Síndrome de Conducto Hepático in the Journal international de Chirurgie, Bruxelles. He discusses the impaired function of this sphincter during stasis and inflammation (e.g., cholangitis), leading to the so-called “hepatic syndrome” indicating that bile duct dilation and spasm are central to this process.
1949 – Mirizzi adds further clinical details in his Síndrome del Conducto Hepático published in Cirugía y Cirujanos. He clinically and radiologically define the syndrome with impacted stones in the gallbladder neck/cystic duct causing external compression of the common hepatic duct, without choledocholithiasis, and confirmed by operative cholangiography.
Colangiografía operatoria: Demuestra con toda nitidez que el colédoco está libre de obstáculo; en cambio, el sistema del hepático no solamente está inyectado, sino que el lipiodol se retiene en forma manifiesta.
La vesícula sin contenido líquido, está repleta de cálculos, tiene paredes engrosadas y se adhiere fuertemente a los tejidos vecinos. El vestíbulo y el conducto cístico están unidos por adherencias robustas al hepático. En el cuello vesicular hay cálculos muy apretados entre sí. – Mirrizi 1949
Operative cholangiogram: Shows with total clarity that the bile duct is free from blockage; instead, the hepatic system is not only enlarged, but the lipiodol [injected contrast] is retained manifest
The gallbladder, devoid of liquid content, is filled with stones, has thickened walls, and is strongly adherent to surrounding tissues. The vestibule and cystic duct are joined by robust adhesions to the hepatic duct. In the gallbladder neck, stones are tightly compacted – Mirrizi 1949
1950 – Albert Behrend and Milton L. Cullen described three cases of internal biliary fistulas where gallstones eroded directly through the gallbladder wall into the common bile duct, forming what they termed cholecysto-choledochal fistulas. Their report emphasised the complete obliteration of the cystic duct in each case and the chronic inflammation anchoring the gallbladder to the bile duct, necessitating reconstruction over a T-tube. One case additionally involved a fistulous connection to the duodenum.
The accompanying illustrations demonstrated the erosion pathway and surgical management, highlighting the clinical significance of these complex biliary communications.
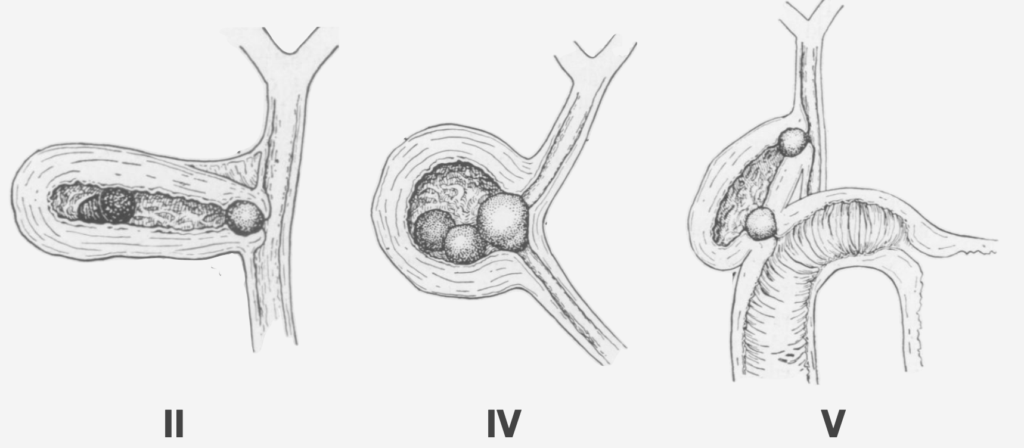
II: The cystic duct has become obliterated due to a chronic inflammatory process and the gallstones have eroded the gallbladder wall and formed a cholecystobiliary fistula [Mirizzi syndrome type II]
IV: The gallstone surrounded by an inflammatory process was clearly dilating the cystic duct fusing the gallbladder to the bile duct [Mirizzi syndrome type IV]
V: The continuous inflammatory process affecting the gallbladder has obliterated the cystic duct, and the gallstones compressed inside the gallbladder, have produced pressure ulcers over the gallbladder walls eroding into the bile duct and the duodenum [Mirizzi syndrome type V] Behrand 1950 [with current classification]
1982 – McSherry et al published a two‑type classification of Mirizzi syndrome:
- Type I: External compression of the common hepatic (or bile) duct by a stone impacted in the cystic duct/Hartmann’s pouch.
- Type II: Cholecystobiliary fistula formation.
1989 – The Csendes classification marks a pivotal shift in the conceptualisation of Mirizzi syndrome by explicitly recognising it as a spectrum of progressive pathological change, rather than a singular entity. Csendes et al. reviewed 219 patients out of over 17,000 biliary surgeries and defined four types of lesions based on the extent of bile duct involvement:
- Type I: External compression of the common hepatic duct by a stone impacted in the cystic duct or Hartmann’s pouch. [Classic Mirizzi syndrome]
- Type II: Cholecystocholedochal fistula involving <1/3 of the bile duct circumference.
- Type III: Fistula involves up to 2/3 of the bile duct circumference.
- Type IV: Complete destruction of the bile duct wall with a wide cholecystobiliary fistula.
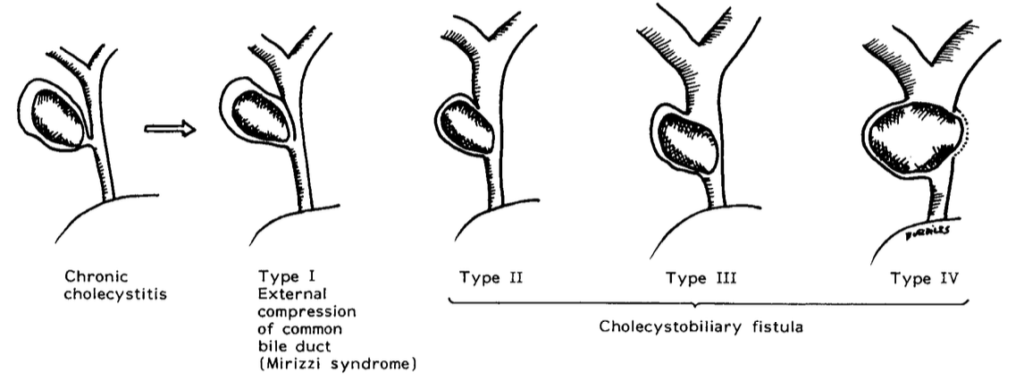
Before Csendes, the literature was scattered, treating Mirizzi syndrome and cholecysto-biliary fistulae as separate or anecdotal entities. Csendes reframed the issue as one of pathological continuum rather than variation, enabling better stratification of risk and surgical decision-making.
- Type I → Cholecystectomy + T-tube (if needed).
- Type II → Fistula suture or choledochoplasty with gallbladder cuff.
- Type III → Choledochoplasty recommended.
- Type IV → Bilioenteric anastomosis (e.g., hepaticojejunostomy).
2002 – Abou-Saif and Al-Kawas re-emphasized the two-stage pathogenesis: (1) extrinsic compression, (2) fistula formation. Also highlighted that cholecystocholedochal fistulas and Mirizzi syndrome lie on a spectrum.
2005–2008 In response to the clinical overlap between Mirizzi syndrome and complex cholecystoenteric fistulas, Marcelo A Beltrán and colleagues expanded the Csendes classification system to Type V:
- Type Va: Any of the existing types I–IV with a cholecystoenteric fistula, without gallstone ileus.
- Type Vb: As above, with gallstone ileus.
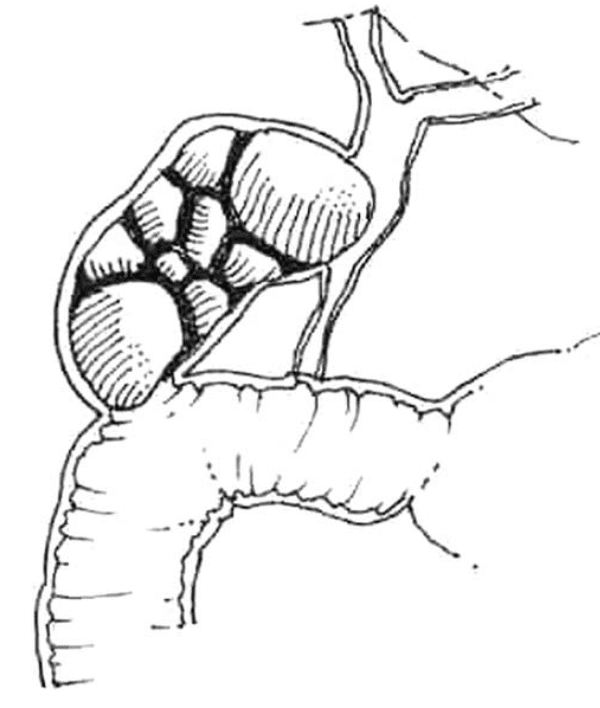
This extension acknowledged that Mirizzi syndrome can progress beyond biliary fistula to involve adjacent organs such as:
- Duodenum (most common, 40%)
- Stomach (32%)
- Colon (28%)
The authors emphasized that Mirizzi syndrome represents a continuum of chronic inflammation, often culminating in complex fistulas involving not only the biliary tree but also gastrointestinal structures. This view challenges older definitions that confined the disease to bile duct compression or erosion alone.
Contemporary Reviews: Emphasize imaging modalities (US, CT, MRCP, ERCP), the importance of preoperative diagnosis to avoid bile duct injury, and the relevance of laparoscopic vs open surgical approaches. Gallstone ileus is now clearly defined as a rare but related complication due to chronic fistulization.
Associated Persons
- Ludwig Courvoisier (1843-1918)
- Hans Kehr (1862-1916)
- Ernst Ludwig Richard Ruge (1878–1953)
- Pablo Luis Mirizzi (1893-1964)
- Atilla Csendes
- Marcelo A Beltrán
References
Original articles
- Kehr H. Die in meiner Klinik geübte Technik der Gallensteinoperationen mit einem Hinweis auf die Indikationen und die Dauererfolge. 1905
- Ruge E. Beitrage zur chirurgischen Anatomie der grossen Gallenwege (Ductus hepaticus, choledochus und pancreaticus) Archiv für Klinische Chirurgie. 1908; 77: 47-77
- Mirizzi PL. Physiologic sphincter of hepatic bile duct. Archives of Surgery 1940; 41: 1325-1333.
- Mirizzi PL. Síndrome de Conducto Hepático. Journal international de chirurgie. 1948; 8: 731–777.
- Mirizzi PL. Síndrome de Conducto Hepático. (Sindrome hepaticiano). Cirugía y Cirujanos 1949; 17(3): 111-133
- Behrend A, Cullen ML. Cholecystocholedochal fistula, an unusual form of internal biliary fistula. Ann Surg. 1950 Aug;132(2):297-303.
- McSherry CK, Fernstenberg H, Virshup M. The Mirizzi Syndrome: Suggested Classification and Surgical Therapy. Surgical Gastroenterology, 1982; 1: 219-225.
- Csendes A, Díaz JC, Burdiles P, Maluenda F, Nava O. Mirizzi syndrome and cholecystobiliary fistula: a unifying classification. Br J Surg. 1989 Nov;76(11):1139-43.
- Beltran MA, Csendes A. Mirizzi syndrome and gallstone ileus: an unusual presentation of gallstone disease. J Gastrointest Surg. 2005 May-Jun;9(5):686-9.
- Beltrán MA, Csendes A, Cruces KS. The relationship of Mirizzi syndrome and cholecystoenteric fistula: validation of a modified classification. World J Surg. 2008 Oct;32(10):2237-43
- Beltrán MA. Mirizzi syndrome: history, current knowledge and proposal of a simplified classification. World J Gastroenterol. 2012 Sep 14;18(34):4639-50.
Review articles
- Pemberton M, Wells AD. The Mirizzi syndrome. Postgrad Med J. 1997 Aug;73(862):487-90
- Abou-Saif A, Al-Kawas FH. Complications of gallstone disease: Mirizzi syndrome, cholecystocholedochal fistula, and gallstone ileus. Am J Gastroenterol. 2002 Feb;97(2):249-54.
- Becker CD, Hassler H, Terrier F. Preoperative diagnosis of the Mirizzi syndrome: limitations of sonography and computed tomography. AJR Am J Roentgenol. 1984 Sep;143(3):591-6.
- Lai EC, Lau WY. Mirizzi syndrome: history, present and future development. ANZ J Surg. 2006 Apr;76(4):251-7.
- Payá-Llorente C, Vázquez-Tarragón A, Alberola-Soler A, Martínez-Pérez A, Martínez-López E, Santarrufina-Martínez S, Ortiz-Tarín I, Armañanzas-Villena E. Mirizzi syndrome: a new insight provided by a novel classification. Ann Hepatobiliary Pancreat Surg. 2017 May;21(2):67-75.
eponymictionary
the names behind the name
BM BCh, Oxford University. Currently training in Australia. Career interest in Hepatology and Emergency Medicine
BA MA (Oxon) MBChB (Edin) FACEM FFSEM. Emergency physician, Sir Charles Gairdner Hospital. Passion for rugby; medical history; medical education; and asynchronous learning #FOAMed evangelist. Co-founder and CTO of Life in the Fast lane | On Call: Principles and Protocol 4e| Eponyms | Books |

