Nasal foreign body
aka Pediatric Perplexity 018
A 3 year old boy has a button battery lodged up his nose. It has proved impossible to remove due to his admirable combativeness.
You decide to perform procedural sedation using ketamine to remove the foreign body.

Questions
Q1. What are the risks of leaving a button battery in the nasal cavity?
Answer and interpretation
Alkaline button batteries should be removed because they can can cause chemical burns.The complications of an intranasal button battery include:
- epistaxis
- purulent, malodorous unilateral nasal discharge
- necrosis of the nasal mucosa and septum
- dislodgement and subsequent ingestion or aspiration
Q2. What extraction methods can be used?
Answer and interpretation
Extraction using instruments:
- Direct extraction using forceps or a suction catheter to grasp the foreign body
- If the foreign body cannot be grasped, a blunt-tipped right-angled probe or a small Foley catheter may be used to dislodge it, or alternatively a ‘glue on a stick’ approach may be attempted
Extraction using positive pressure:
- Ask the patient to take a deep breath and blow hard through the nose while a parent occludes the unobstructed naris
- Administer a short burst of positive pressure via the patient’s mouth while the unobstructed naris is occluded – best performed as a ‘kiss’ by a parent (the proceduralist may get an ear full of snot!)
Q3. How is ketamine used for procedural sedation?
Answer and interpretation
Procedural sedation should be performed with the use of appropriate monitoring equipment (e.g. baseline vital signs and continuous SO2 monitoring, and ETCO2 monitoring if available) on a fasted and consented patient by adequately trained and resourced staff who are able to manage an airway emergency
Ketamine for procedural sedation can be given intravenously or intramuscularly. The dose of ketamine to produce profound dissociation is:
- 1 to 1.5 mg/kg IV
- This is given over 1-2 minutes, is effective within 1-2 minutes, results in effective sedation lasting 10-20 minutes, and if inadequate a further 0.5 mg/kg dose may be given
- OR4 to 5 mg/kg IM
- This is effective within 2 to 5 minutes, results in effective sedation lasting 15-30 minutes and a repeat IM dose (2-4 mg/kg) can be given after 10 to 15 minutes if the initial effect is inadequate
The IM route is useful when IV access is problematic, but the downsides include:
- a longer recovery time (mean of 120 minutes for IM vs. 80 minutes for IV)
- vomiting is more likely
- sedation doses are less easily titrated
Medication adjuncts:
- Traditionally, in older children (e.g. >5 years old), prophylactic administration of a low-dose benzodiazepine (midazolam, 0.02-0.05 mg/kg) is given to reduce the risk of emergence phenomena such as hallucinations and agitation. However, this is not supported by evidence from randomised controlled studies. Instead midazolam appears to be associated with more respiratory complications and less emesis.
- Atropine (0.02 mg/kg, up to maximum of 0.6mg) or glycopyrrolate are widely administered as a co-medication to reduce the hypersalivation caused by ketamine. The evidence-base for this practice is unclear.
A recent RCT (2011) in Annals of Emergency Medicine showed an NNT of 6 for pre-administration of 0.03mg/kg IV midazolam for reducing agitation from ketamine in adults. Reuben Strayer discusses this in Taming the Ketamine Tiger, and provides a good rationale for avoiding pre-medication and taking a prn approach.
Q4. What are the risks of performing this procedure with ketamine sedation?
Answer and interpretation
There are risks associated with the procedure itself:
- failure
- local trauma resulting in bleeding
- inadvertently advancing the foreign body to a more distant site in the aerodigestive tract
As well as the risks and side-effects of ketamine sedation:
- Laryngospasm (see below)
- Hypersalivation (~30%; ~10% with atropine in some studies)
- Emesis (~5-15%)
- Emergence phenomena such as recovery agitation (10-20%, with 1-2% clinically significant), dreams, hallucinations and depersonalisation
- Transient respiratory depression (usually in the first 2-3 minutes following a large, rapidly administered IV dose)
- Transient mild increase in heart rate and blood pressure
- Evanescent patchy erythematous rash about the upper torso (5-20%)
- Nystagmus and random purposeless movements while sedated
- ketamine induces neuronal death in animal studies — the implication of this for clinical use is not yet known.
While the battery is being removed the boy develops laryngospasm.
Q5. What are the clinical features of laryngospasm?
Answer and interpretation
Laryngospasm is potentially life-threatening closure of the true vocal chords resulting in partial or complete airway obstruction unresponsive to airway positioning maneuvers.
Laryngospasm may be preceded by a high-pitched inspiratory stridor — some describe a characteristic ‘crowing‘ noise — followed by complete airway obstruction. It can occur without any warning signs. It should be suspected whenever airway obstruction occurs, particularly in the absence of an obvious supraglottic cause.
Q6. What are the clinical features of complete airway obstruction?
Answer and interpretation
Complete airway obstruction is characterized by:
- No chest wall movement with no breath sounds on auscultation
- No stridor or airway sounds
- Sudden loss of carbon dioxide waveform
- Inability to manually ventilate with bag-mask ventilation
Q7. How would would you manage the laryngospasm?
Answer and interpretation
Management of laryngospasm includes the following:
- Tell the proceduralist to stop the procedure.
- Call for expert help. Ensure equipment for difficult intubation is at hand.
- Administer 100% oxygen through a mask with a tight seal and a closed expiratory valve to try to force the vocal cords open with positive pressure. Hypoxia can occur rapidly in children when ventilation is inadequate.
- Use suction to clear the airway of blood and secretions – but only if the child is adequately oxygenated.
- Attempt manual ventilation while continuing to apply continuous positive airway pressure (CPAP).
- Attempt to break the laryngospasm by applying painful inward and anterior pressure at ‘Larson’s point‘ bilaterally while performing a jaw thrust. Larson’s point is also called the ‘laryngospasm notch‘.
- Consider deepening sedation/ anesthesia (e.g. low dose propofol) to reduce laryngospasm.
- If hypoxia supervenes consider administering suxamethonium. A dose of only 0.1-0.5 mg/kg may be sufficient, but in severe laryngospasm administer a full dose (1-2 mg/kg IV) and perform intubation. If there is no IV access administer the suxamethonium IM (3-4 mg/kg). Many experts advocate IM injection into the tongue.
- Be prepared for bradycardia and cardiac arrest as a result of airway manipulation and/or suxamethonium administration in the hypoxic child. Correct hypoxia urgently and administer atropine (0.02mg/kg) for bradycardia.Laryngospasm is usually brief and may be followed by a gasp – you may need to wait for this moment when attempting to pass a tracheal tube. A chest thrust maneuver immediately preceding intubation may temporarily open the vocal cords and allow passage of the tube.
- Laryngospasm may recur as neuromuscular blockade wears off.
Where is the ‘laryngospasm notch‘? AKA Larson’s notch – according to Phil Larson:
“This notch is behind the lobule of the pinna of each ear. It is bounded anteriorly by the ascending ramus of the mandible adjacent to the condyle, posteriorly by the mastoid process of the temporal bone, and cephalad by the base of the skull.”
Larson PC 1988
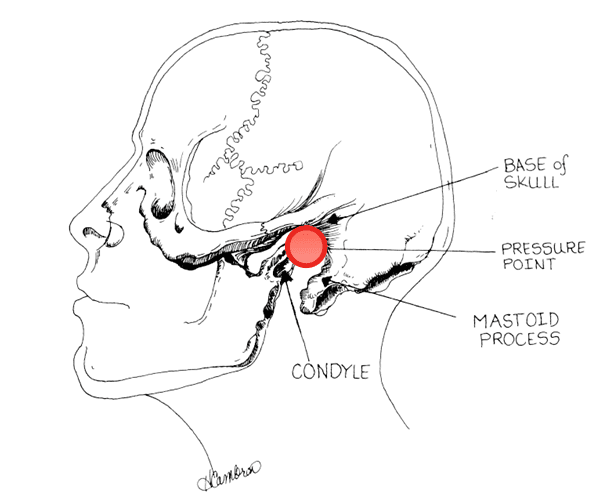
Schematic illustration of laryngospasm notch bounded anteriorly by the condyle of the mandible, posteriorly by the mastoid process, and superiorly by the base of the skull. Digital pressure is applied firmly inwardly and anteriorly on each side of the head at the apex of the notch (see pressure point arrow), which is slightly cephalad to the plane of the earlobes (not shown).
Q8. Is laryngospasm a complication associated with ketamine?
Answer and interpretation
Ketamine is known to preserve and exaggerate protective airway reflexes. Laryngospasm is a much feared complication — however, it is extremely rare.From a 1990 meta-analysis of 97 studies including 11.589 children, Green and colleagues reported a rate of laryngospasm of 0.4% from ketamine sedation. In nearly all cases the laryngospasm was transient and responded to oxygenation and ventilation. Only two children (0.017%) required intubation for laryngospasm.
Laryngospasm is more common in children compared with adults.
Q9. How can laryngospasm be prevented?
Answer and interpretation
Avoid ketamine sedation in children if:
- <3 months of age — Very young children have a higher risk of airway problems, laryngospasm and apnoea from all forms of sedation and anesthesia
- active URTI (RR 5.5)
- active asthma (RR 3.7)
Ensure adequate depth of sedation before commencing the procedure and avoid stimulation of the posterior pharynx.
Spraying the posterior pharynx with 1% lignocaine may reduce the risk of laryngospasm, but local anesthesia may also compromise airway protection.
Q10. What are the contraindications for ketamine sedation?
Answer and interpretation
Absolute contraindications:
- <3 months of age
(higher risk of airway complications) - Known or suspected psychosis, even if currently stable and controlled with medications
Relative contraindications:
- Age of 3-12 months – (higher risk of airway complications)
- Procedures involving stimulation of posterior pharynx – (higher risk of laryngospasm)
- History of airway instability, tracheal surgery, or tracheal stenosis – (presumed higher risk for airway complications)
- Active pulmonary infection or disease, including upper respiratory infection or asthma in children – (higher risk of laryngospasm)
- Known or suspected cardiovascular disease, including angina, heart failure, or hypertension
- Head injury associated with loss of consciousness, altered mental status, or emesis – (elevated intracranial pressure with ketamine)
- Central nervous system masses, abnormalities, or hydrocephalus – (elevated intracranial pressure with ketamine)
- Glaucoma or acute globe injury – (elevated intraocular pressure with ketamine)
- Porphyria, thyroid disorder, or thyroid medications – (enhanced sympathomimetic effect)
Note that elevated intracranial pressure due to ketamine is controversial — and probably a myth — but is still widely quoted as a complication/ contra-indication for ketamine use.
References
- Long N. Button Battery Update. LITFL
- Strayer E. Taming the Ketamine Tiger. EMupdates
- Larson PC. Laryngospasm-The Best Treatment. Anesthesiology, 89 (5), 1293-1294 PMID: 9822036
- Guideline: Ketamine use in the emergency department. RCH Melbourne
- Madati PJ (2010). Ketamine: Procedural Pediatric Sedation In The Emergency Department. Pediatric Emergency Medicine Practice, 8(1).
- Nickson C. Pediatric Procedural Sedation with Ketamine. LITFL
- Clinical Practice Guideline for Emergency Department Ketamine Dissociative Sedation: 2011 Update. ACEP
- Wathen, J. (2000). Does midazolam alter the clinical effects of intravenous ketamine sedation in children? A double-blind, randomized, controlled, emergency department trial Annals of Emergency Medicine, 36 (6), 579-588 DOI: 10.1067/mem.2000.111131
- Strayer R, Nelson L. (2008). Adverse events associated with ketamine for procedural sedation in adults The American Journal of Emergency Medicine, 26 (9), 985-1028 DOI: 10.1016/j.ajem.2007.12.005
- Roback M, et al. (2006). A Randomized, Controlled Trial of IV Versus IM Ketamine for Sedation of Pediatric Patients Receiving Emergency Department Orthopedic Procedures. Annals of Emergency Medicine, 48 (5), 605-612 DOI: 10.1016/j.annemergmed.2006.06.001
- Green S, et al (2009). Predictors of Airway and Respiratory Adverse Events With Ketamine Sedation in the Emergency Department: An Individual-Patient Data Meta-analysis of 8,282 Children. Annals of Emergency Medicine, 54 (2), 158-168 DOI: 10.1016/j.annemergmed.2008.12.011
- Heinz, P. (2006). Is atropine needed with ketamine sedation? A prospective, randomised, double blind study. Emergency Medicine Journal, 23 (3), 206-209 PMID: 164981586

CLINICAL CASES
Pediatric Perplexity
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
