Vaginal bleeding – non pregnant
Vaginal bleeding can be thought of as pregnancy related or non-pregnancy related. Causes may be primary or abnormal uterine bleeding, or secondary genital tract bleeding
Vaginal bleeding in the non-pregnant patient can be categorized as:
- Primary or abnormal uterine bleeding (most common)
- Secondary genital tract bleeding
All reproductive-age women with PV bleeding must be assumed to be pregnant until proven otherwise.
All postmenopausal women with PV bleeding must be assumed to have carcinoma until proven otherwise.
See separate documents for pregnancy-related bleeding:
- Vaginal Bleeding in Early Pregnancy – Threatened Miscarriage
- Vaginal Bleeding in Early Pregnancy – Miscarriage
Terminology
- Menorrhagia: Excessive/prolonged bleeding (>80 mL per cycle)
- Metromenorrhagia: Irregular and excessive bleeding
- Oligomenorrhoea: Cycle length 35 days to 6 months
- Polymenorrhoea: Cycles <21 days apart
- Amenorrhoea: No bleeding for >6 months
- Intermenstrual Bleeding: Bleeding between regular periods
Physiology
Normal cycle characteristics:
- Cycle: 24–35 days
- Luteal phase: 14 ± 1 days
- Menstruation: <80 mL over 4–7 days
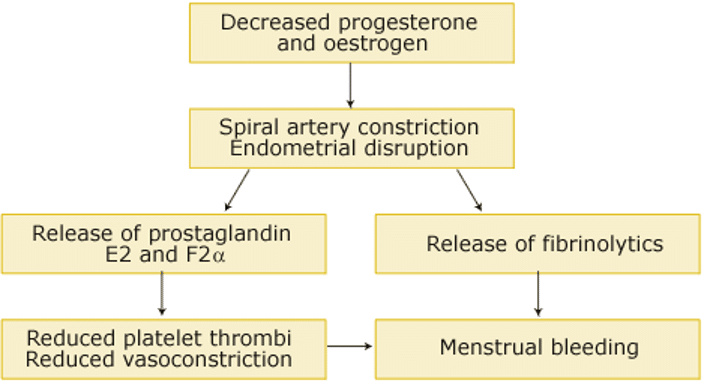
Pathophysiology
1. Primary/Uterine Causes:
- Ovulatory bleeding:
- Regular, heavy bleeding
- Increased prostaglandins/fibrinolytic activity
- Anovulatory (dysfunctional) bleeding:
- Irregular, heavy or light bleeding
- Due to unopposed estrogen (e.g. PCOS, stress)
2. Secondary Genital Tract Causes:
- Anatomical: Fibroids, polyps, malignancy, AVMs
- Infective: Endometritis, cervicitis
- Trauma
- Systemic: Thyroid disease, coagulopathy, PCOS
- Iatrogenic: IUDs, anticoagulants
Clinical Assessment
History:
- Cycle regularity, volume, timing
- Clots suggest heavy bleeding
- Symptoms of anaemia
- Systemic signs (endocrine, infection)
Examination:
- Haemodynamic status
- Anaemia signs
- Endocrinopathy signs
- PV exam (trauma, local lesions)
Investigations
Bloods:
- FBE (anaemia, infection)
- CRP (infection)
- Beta-HCG (exclude pregnancy)
- Iron studies (microcytic anaemia)
- Coagulation profile
- Endocrine screen: TFTs, pituitary hormones, oestrogen/progesterone (if indicated)
- Group & save/crossmatch (if bleeding severe)
Microbiology:
- Vaginal/cervical swabs if infection suspected
Imaging:
- Ultrasound: Fibroids, adenomyosis, polyps, endometrium
- EUA/D&C: If malignancy suspected, especially postmenopausal bleeding
Management
Initial Measures:
- Resuscitation
- Transfusion if haemodynamically unstable or symptomatic anaemia
Pharmacologic Treatments
1. Progestins
- Norethisterone: 5 mg BD–TDS (days 1–21 for 6 months)
- Medroxyprogesterone: 10 mg 1–3x daily (same protocol)
2. Antifibrinolytics
- Tranexamic acid: 1–1.5 g Q6–8h x 3–5 days
3. NSAIDs (Antiprostaglandins)
- Mefenamic acid: 500 mg TID
- Ibuprofen: 200–400 mg TID–QID (max 1600 mg/day)
- Naproxen: 500 mg initially, then 250 mg Q6–8h (max 1250 mg/day)
4. COCP (Combined Oral Contraceptive Pill)
- Thins endometrium; suitable for both ovulatory and anovulatory cycles
- Use a pill with ≥30 mcg ethinylestradiol
5. LNG-IUS (Levonorgestrel IUD)
- Long-term option; requires trained insertion
- Effective for 5 years
Acute Heavy Bleeding
1. Tranexamic Acid:
- 1–1.5 g PO Q6–8h or 10 mg/kg IV Q8h
2. Hormonal Therapy:
- Norethisterone: 5–10 mg PO Q4h (max 80 mg/day)
- Medroxyprogesterone: 10 mg PO Q4h
- COCP: One tab Q6h (30–35 mcg ethinylestradiol), reassess at 48h
- High-dose oestrogen (if needed): 50 mcg Q6h, monitor for nausea
Surgical Options
Consider if:
- Childbearing not desired
- Perimenopausal
- Poor response to medication
- Significant pathology (e.g., atypical hyperplasia)
Options:
- Endometrial ablation
- Hysterectomy
Secondary Causes
- Treat underlying condition (infection, endocrine, malignancy)
Preventive Measures
- PAP smear screening
- HPV vaccination (Gardasil)
Disposition
Admit if:
- Haemodynamic compromise
- Severe anaemia
- Significant systemic illness
Outpatient referral:
- Urgent for all postmenopausal bleeding
- Stable patients
The Pathophysiology of Menorrhagia:
- The endometrium undergoes proliferation and thickening during the follicular phase under the influence of oestrogen produced by the ovary.
- A normal endometrial thickness, as measured by ultrasound, is between 6 and 12 mm.
- After ovulation, the endometrium is exposed to progesterone produced by the corpus luteum.
- Biochemically, the cycle is confirmed as being ovulatory if the serum progesterone is above 20 nmol/L during the midluteal phase (5 to 10 days before menses).
- Menorrhagia is favoured by endometrial development that is not followed by ovulation, excessive local production of prostaglandins, or excessive fibrinolysis of clot
References
FOAMed
- Quo M. Abnormal vaginal bleeding. CCC
- Hiller J, Yarwood L. Vaginal bleeding – nonpregnant. FFS
- Yarwood L, Hiller J. Vaginal bleeding – early pregnancy. FFS
- Hiller J, Yarwood L. Vaginal bleeding – miscarriage. FFS
- Yarwood L, Hiller J. Septic abortion. FFS
- Mackenzie J, Beech A. Procedure: Speculum examination. LITFL
Fellowship Notes
Doctor at King Edward Memorial Hospital in Western Australia. Graduated from Curtin University in 2023 with a Bachelor of Medicine, Bachelor of Surgery. I am passionate about Obstetrics and Gynaecology, with a special interest in rural health care.
Educator, magister, munus exemplar, dicata in agro subitis medicina et discrimine cura | FFS |


