Puffed Post-Tracheostomy
aka Pulmonary Puzzler 015
A 40 year old man had been in ICU for nearly 2 weeks and was slow to wean off the ventilator due to ARDS (acute respiratory distress syndrome). A percutaneous dilational tracheostomy (PDT) was performed. Following the procedure he developed a requirement for increased respiratory support.
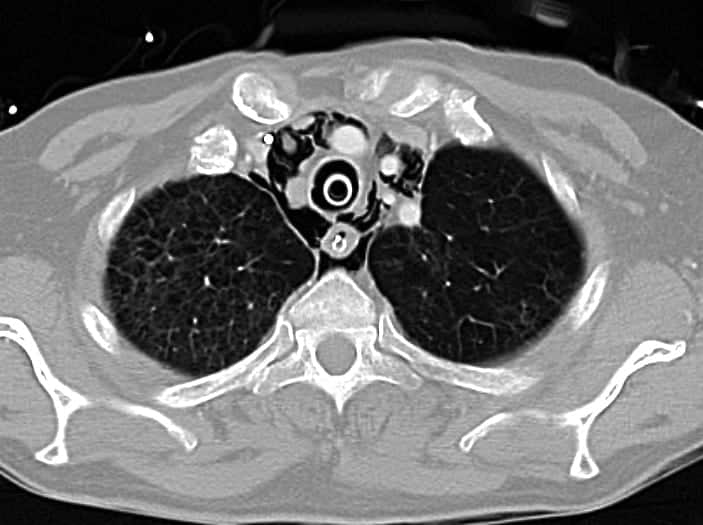
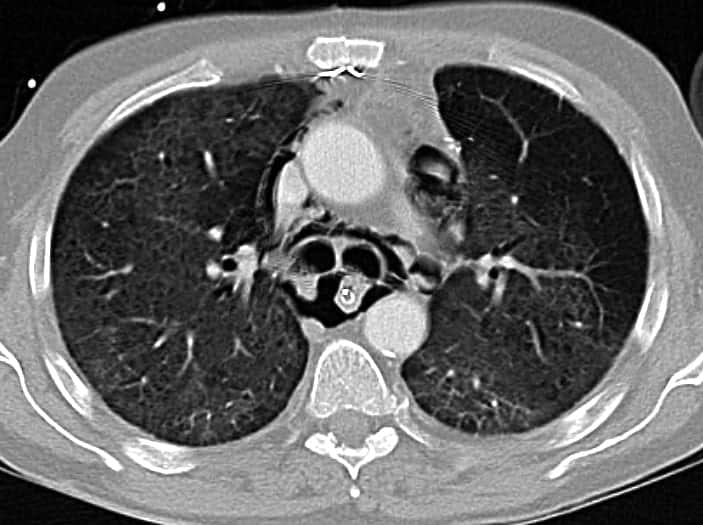
He was sufficiently stable for a CT chest to be performed. Representative images are shown below:
Questions
Q1. Describe the CT findings
Answer and interpretation
The key finding is Extensive pneumomediastinum
There is gas within the supra-aortic, sub-aortic and para-cardiac mediastinum, particularly in the posterior compartment of the mediastinum.
Other findings:
- endotracheal tube
- nasogastric tube
- bilateral lung opacities and altered lung architecture consistent with resolving ARDS
Q2. What are the important possible causes of the key finding on the CT Chest?
Answer and interpretation
Possible causes include:
- Complication of tracheostomy resulting in a small tracheal tear
- Complication of mechanical ventilation due to ARDS and need for high pressures
- Esophageal rupture post NG tube placement
— pleural effusion would be expected - Mediastinitis
— fluid or a collection would be expected
Q3. What clinical findings may be present?
Answer and interpretation
There may be very few clinical findings!
If present they may include:
- subcutaneous emphysema of the neck
- Hamman sign (aka Hammond crunch)
— a rarely heard rasping, crunching sound synchronous with the heart beat that is best heard over the precordium in the left lateral position
— caused by the heart beating against air-filled tissues - haemoptysis
- partial or complete airway obstruction
- respiratory distress and/or need for increased respiratory support.
If tension pneumomediastium develops the patient will become tachycardic and hypotensive due to impaired venous return mimicking cardiac tamponade. Neck vein distention will not be seen in the presence of subcutaneous emphysema of the neck.
Q4. What are the management priorities?
Answer and interpretation
Key priorities are supportive care of the patient and identification and treatment of possible tracheobronchial injury.
- ensure adequate oxygenation
- provide ventilatory support while minimising tidal volumes and airway pressures to limit exacerbation of the air leak
- fiberoptic endoscopic evaluation of the tracheobronchial tree to assess for presence, location, depth and length of tears (best performed in an operating theatre)
- tracheobronchial tears may be amenable to bypass by bronchoscopy-assisted endotracheal tube advancement, or even endobronchial intubation for tracheobronchial injury near the carina
- the indications for conservative versus surgical repair of iatrogenic tracheobronchial injury are poorly defined and remain controversial
— surgery may be performed via thoracotomy and/or a cervical approach
— surgery should be performed if there is progressive pneumomediastinum, increasing subcutaneous emphysema, evidence of oesophageal injury or mediastinitis - broad spectrum antibiotics are often used to prevent mediastinitis
Further Reading: Esophageal rupture is considered in Pulmonary Puzzle 003.
Q5. How would you treat a tension pneumomediastinum?
Answer and interpretation
True tension pneumomediastinum is rare, and requires emergency decompression by bedside mediastinotomy.
Bedside cervical mediastinotomy can be performed by making an incision in the jugular notch. If air is trapped in posterior spaces then this approach may not be effective. A subxiphoid approach can be attempted, and an approach through the esophageal hiatus via a mini-laparotomy has been described.
Q6. Should chest x-rays be performed after performing percutaneous dilational tracheostomy (PDT)?
Answer and interpretation
It is argued that complications following PDT are rare and that new abnormalities on chest x-ray are rarely seen. However, if difficulties are encountered during the procedure, or if the patient deteriorates afterward, a chest x-ray should be performed.
References
- For more Pulmonary cases check out the LITFL Top 150 Chest X-Rays
- Pulmonary Puzzle 003 — Roast duck and juniper beer
- Frova G, Sorbello M. Iatrogenic tracheobronchial ruptures: the debate continues. Minerva Anestesiol. 2011 Dec;77(12):1130-3. PMID: 21666570.
- Kumar VM, Grant CA, Hughes MW, Clarke E, Hill E, Jones TM, Dempsey GA. Role of routine chest radiography after percutaneous dilatational tracheostomy. Br J Anaesth. 2008 May;100(5):663-6. PMID: 18369239.

CLINICAL CASES
Pulmonary Puzzler
Intensivist in Wellington, New Zealand. Started out in ED, but now feels physically ill whenever he steps foot on the front line. Clinical researcher, kite-surfer | @DogICUma |