Recombinant Factor VIIa to the rescue!?
aka Hematology Hoodwinker 002
Your trauma patient in resus bay 1 continues to bleed like a stuck pig.
Half a dozen people are squeezing bags of various blood products — FFP, cryo, platelets and packed red blood cells. You try to keep your mind on the job, fighting off the dreaded realisation that you will be forced to buy your first new pair of shoes since 1998. “Damn it, these shoes are really comfortable”, you think to yourself as you squelch across the blood-soaked room. However, right now you could do without those trademark ‘ventilation ports’ that spontaneously appeared about 4 years ago…
Just as one of the nurses comes in with a kitchen sink and gets ready to throw it at the patient, one of the senior registrars mumbles, “Maybe we should give him Factor Seven?”.
The New Zealand All Blacks had their own ‘Factor Seven’, Samoan-born Michael Jones. The ‘Iceman’ is the greatest open-side flanker of all time — his all action style completely revolutionised the role of the flanker. When asked how he reconciled his devastating tackling technique with being a committed Christian, Jones said, “as the Lord says… it’s better to give than to receive.”
Questions
Q1. What is recombinant factor VIIa (rFVIIa)?
Answer and interpretation
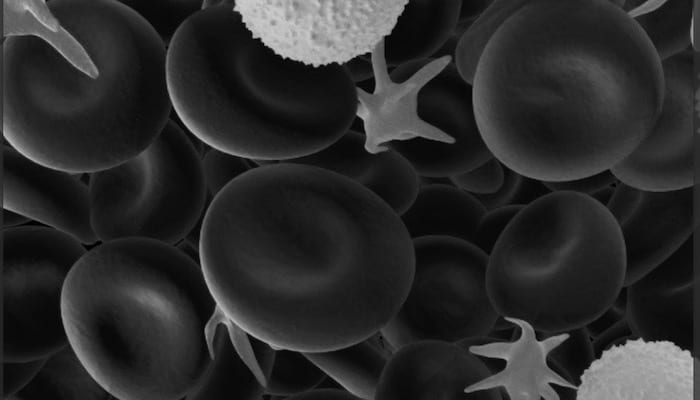
rFVIIa is produced by Novo Nordisk AG and marketed as Novoseven. It also goes by the catchy generic name of ‘eptacog alpha activated’. Factor VIIa is a trypsin-like serine protease involved in the coagulation cascade.
rFVIIa is a novel agent used to control intractable hemorrhage. It is increasingly used as salvage therapy when things are going seriously bad… by those who are impatiently averse to the old saying, ‘all bleeding stops eventually’.
Q2. What are the indications for recombinant factor VIIa (rFVIIa)?
Answer and interpretation
Ahh, the million dollar question (quite literally — it’s expensive stuff).
The indications for rFVIIa are highly controversial, and there is widespread ‘off-label’ use of the drug. Hospitals should have a set of guidelines in place for the availability and use of rFVIIa, and agreement between more than one specialist is often required prior to its administration.
rFVIIa is licensed for treatment of bleeding episodes in patients with hemophilia and alloantibodies to Factor VIII or IX (i.e. antibodies that bind and inhibit these clotting factors).
Off-label uses include:
- trauma
- post-cardiac bypass
- intracranial hemorrhage
- massive obstetric hemorrhage
- gastrointestinal variceal bleeding
- reversal of anticoagulation
- perioperative hemostasis
- platelet disorders
rFVIIa is unlikely to be effective if the patient is cold, acidemic (e.g. pH<7.1-7.2), hypocalcemic and if other blood products have not yet been administered in sufficient amounts (e.g. FFP, platelets, cryoprecipitate) — these issues should be dealt with first.
Ideally the following should be present before rFVIIa administration:
- hematocrit >24%
- pH >7.2
- platelets >50 x 10E9/L
- fibrinogen >1.0 g/L
- euthermia (this probably isn’t so important for rFVIIa)
Nevertheless, exactly when to give rFVIIa is highly contentious, as we shall see in the coming questions.
Q3. What is recombinant rFVIIa’s mechanism of action?
Answer and interpretation
rFVIIa can work in two ways to promote clot formation:
- it complexes with exposed subendothelial Tissue Factor at the site of injury.
- it acts on the surface of activated platelets, independent of Tissue Factor.
It then activates the extrinsic clotting cascade (via Factors IXa and Xa) generating a ‘thrombin burst‘ (Factor Xa complexes with Factor V to form the Prothrombinase complex that in turn activates prothrombin). Thrombin converts fibrinogen to fibrin and, voila, a clot is formed.
rFVIIa also helps stabilise the clot by activating fibrinolytic inhibitors.
The localisation of rFVIIa’s action has the theoretical advantage of limiting it’s action to the sites of injury, supposedly reducing the risk of thrombotic complications.
Q4. When should recombinant Factor VIIa NOT be used?
Answer and interpretation
rFVIIa should not be given if:
- the patient’s condition is unsalvageable
- hemorrhage is surgically correctable (recombinant Factor VIIa will not stop ‘surgical bleeding’)
Relative contraindications are:
- history of thromboembolic events (e.g. pulmonary emboli, myocardial infarction, cerebrovascular accident, deep vein thrombosis) within the previous 6 months.
- the patient is hypothermic and acidemic (pH <7.1-7.2) and other factors have not been adequately replaced (e.g. FFP, cryoprecipitate, platelets).
Recombinant Factor VIIa should not be given instead of other blood product administration and it should not be used too early (but not too late either… as a rule of thumb it should probably be given within 3 hours of the onset of the bleeding episode).
- Adequate FFP, cryoprecipitate and platelets need to be present for full effect.
- Some experts guesstimate that somewhere between 8 and 20 units of PRBCs is when the use of rFVIIa is likely to be cost-effective.
Q4. What is the evidence base supporting the use of rFVIIa?
Answer and interpretation
A major concern with the widespread off-label use of rFVIIa (apart from the cost and potential for thrombotic complications) is the paucity of convincing evidence for its effectiveness. Off-label use continues to be driven by clinicians, often because of their own remarkable anecdotal success stories (I’ve seen a few ‘miracles’ myself).
Here is a brief (?) overview of the evidence base for the use of rFVIIa for various indications:
Hemorrhage in Hemophilia A and B
- Lusher et al, 2005 — A randomised controlled trial that showed “>70% ‘efficient or excellent’ treatment of hemorrhage”.
- Hay et al, 1997 — Review of a database of compassionate use from 32 international centers showed ~90% effective hemorrhage control within 8 hours.
Hemorrhage in trauma
- Use of rFVIIa in trauma was first described in a soldier in 1999 and there have been numerous case series since.
- Boffard et al, 2005 — Two parallel double blinded randomised controlled trials (one blunt trauma, one penetrating) totaling 277 patients who had received >6 units of PRBCs; the treatment arms received 3 doses of rFVIIa (200, 100 and 100 mcg/kg) after the 8th unit of PRBCs. Results: no mortality difference, blunt trauma patients treated with rFVIIa had a mean of 2.6 units less PRBCs, 20% less patients needed massive transfusion (>20 units PRBCs). No significant differences in the penetrating trauma group. Post-hoc subgroup analyses suggested greater benefit in those with traumatic coagulopathy and those with higher initial likelihood of survival.
- Multicenter prospective studies, such as the CONTROL trial, are underway…
Intracerebral hemorrhage (ICH)
There have been two big drug-company funded trials.
- Mayer et al, 2005 — 399 adults that presented within 3 hours of acute ICH (confirmed by CT). There was a 16% ARR in death or severe disability at 90 days. However this was a phase II trial actually designed to assess safety, and the primary outcome of ‘overall adverse events’ was not different between the placebo and treatment arms.
- Mayer et al, 2008 (the FAST Trial) — The follow up phase III trial consisted of 841 patients. The 80 mcg/kg treatment group had a mean increase in ICH volume of 11% that was significantly less than the 26% seen in the placebo group. However, there was no difference in rates of mortality, disability or thromboembolic events.
Reversal of anticoagulation
- Prospective clinical trials are lacking but multiple case reports and case series describe the rapid normalisation of INR following rFVIIa treatment in hemorrhage due to warfarin-associated coagulopathy.
Gastrointestinal bleeding
- Bosch et al (2004) — 245 cirrhotic patients scheduled to undergo endoscopy for active gastrointestinal bleeding were randomised to placebo or 8 doses of 100 mcg/kg rFVII over up to 30 hours. There was no difference in the composite endpoint of ‘failure to control bleeding, rebleeding and death’ between the two groups. A subgroup analysis showed a significant decrease in the composite endpoint in those with variceal bleeding (23% vs 8%).
Other uses
- Many scenarios that might be considered for use of rFVII have yet to be studied and overall there are few clinical trials supporting the various uses.
- A systematic review of seven RCTs by Ranucci et al (2008) found that there was less need for blood transfusion in surgical patients that were treated with rFVIIa, but patients would require massive transfusions for it to be cost-effective.
- No firm conclusions can be drawn, but there are case series and retrospectives studies that have indicated possible benefits for rFVIIa therapy in the following settings: after cardiopulmonary bypass, liver surgery, post-partum hemorrhage, and patients with platelet disorders (e.g. Glanzmann thrombasthaenia).
Q5. How should rFVIIa be administered and in what dose?
Answer and interpretation
Standard dosing of rFVIIa in bleeding hemophilia patients is:
90 mcg/kg IV every 2-3 hours until bleeding stops, although between 35 and 120 mcg/kg has been successfully used. Up to 270 mcg/kg is used in children.
Dosing for off-label indications is understandably variable — in a review of off-label use the mean doses used were 76 mcg/kg for ‘prophylactic’ use and 89 mcg/kg for’ therapeutic’ use.
Suggested doses for off-label indications according to Fishman, et al (2008) are shown below:

rFVIIa is given intravenously over 2-5 minutes and has a half-life of 2.7 hours (although this varies between individuals and according to clinical state). It should be kept refrigerated.
Q6. What are the main complications of rFVIIa?
Answer and interpretation
There are two main types of complications:
- thrombotic complications
- DVT, PE, MI, stroke and microvascular occlusion contributing to multiple organ dysfunction syndrome (MODS).
- The risk of thrombosis is about 1% in bleeding hemophiliacs with alloantibodies. The risks may be much higher in patients with widespread exposed Tissue Factor (e.g. sepsis, atherosclerosis or DIC).
- Studies thus far have suggested that rFVIIa has few complications, though they have generally not been powered to detect adverse effects. Indeed, thrombotic complications are found in many patients who die (from whatever cause) following rFVIIa therapy.
- bankrupting the health system
- did I mention it’s expensive?! (about US$4500/ 4.8mg vial… you do the math)
References
- Trauma.org —Recombinant Factor VIIa (NovoSeven) for Traumatic Coagulopathy
- Crashingpatient.com — Blood therapy
- Boffard KD, Riou B, Warren B, et al. Recombinant factor VIIa as adjunctive therapy for bleeding control in severely injured trauma patients: two parallel randomized, placebo-controlled, double-blind clinical trials. J Trauma. 2005 Jul;59(1):8-15; discussion 15-8. PMID: 16096533.
- Bosch J, Thabut D, Albillos A, et al. Recombinant factor VIIa for variceal bleeding in patients with advanced cirrhosis: A randomized, controlled trial. Hepatology. 2008 May;47(5):1604-14. PMID: 18393319.
- Fishman PE, Drumheller BC, Dubon ME, Slesinger TL. Recombinant activatedfactor VII use in the emergency department. Emerg Med J. 2008 Oct;25(10):625-30. Review. PMID: 18843055.
- Grottke O, Henzler D, Rossaint R. Activated recombinant factor VII (rFVIIa). Best Pract Res Clin Anaesthesiol. 2010 Mar;24(1):95-106. Review. PMID: 20402173.
- Hay CR, Negrier C, Ludlam CA. The treatment of bleeding in acquired haemophilia with recombinant factor VIIa: a multicentre study. Thromb Haemost. 1997 Dec;78(6):1463-7. PubMed PMID: 9423795.
- Lusher JM, Roberts HR, Davignon G, Joist JH, Smith H, Shapiro A, Laurian Y, Kasper CK, Mannucci PM et al. A randomized, double-blind comparison of two dosage levels of recombinant factor VIIa in the treatment of joint, muscle and mucocutaneous haemorrhages in persons with haemophilia A and B, with and without inhibitors. rFVIIa Study Group. Haemophilia. 1998 Nov;4(6):790-8. PMID: 10028299.
- Mayer SA, Brun NC, Begtrup K, et al; Recombinant Activated Factor VII Intracerebral Hemorrhage TrialInvestigators. Recombinant activated factor VII for acute intracerebral hemorrhage. N Engl J Med. 2005 Feb 24;352(8):777-85. PMID: 15728810.
- Mayer SA, Brun NC, Begtrup K, et al. Efficacy and safety of recombinant activated factor VII for acute intracerebral hemorrhage. N Engl J Med. 2008 May 15;358(20):2127-37. PMID: 18480205 [FAST trial]
- Ranucci M, Isgrò G, Soro G, et al. Efficacy and safety of recombinant activated factor vii in major surgical procedures: systematic review and meta-analysis of randomized clinical trials. Arch Surg. 2008 Mar;143(3):296-304; discussion 304. Review. PMID: 18347278
CLINICAL CASES
Hematology Hoodwinker
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
