Robert Andrew Hingson

Robert Andrew Hingson (1913-1996) was an American anesthesiologist.
Hingson’s career encompassed regional anaesthesia, medical device innovation, and global humanitarian medicine. His work sought to extend effective medical care beyond the limits of single injections, single patients, or conventional hospital settings.
Hingson is best known for his role in the development of continuous caudal and epidural analgesia. Working with obstetrician Waldo B. Edwards he transformed caudal block from an intermittent technique into a continuous, titratable form of neuraxial analgesia. Central to this advance was the Hingson–Edwards malleable caudal needle, which enabled prolonged epidural access via the sacral hiatus.
Hingson became a prominent innovator in portable medical technology and humanitarian health. He developed the Western Reserve Midget (Hingson Field Unit) for portable anaesthesia and resuscitation, and the Hingson Peace Gun, a high-speed jet injector that enabled rapid, needle-free mass vaccination. Through the Brother’s Brother Foundation (BFF), which he founded in 1958, Hingson led and supported large-scale immunisation and medical relief programmes worldwide, contributing to early global efforts against polio, influenza, and smallpox.
Biographical Timeline
- Born April 13, 1913 in Annniston, Alabama
- 1935 – Awarded BA, University of Alabama.
- 1938 – Graduated MD, Emory University School of Medicine, Atlanta. As a medical student, delivered 82 babies, many without anaesthesia, an experience that influenced his later focus on obstetric pain relief.
- 1939 – Internship at the US Marine Hospital, Staten Island, New York. Joined the US Coast Guard / Public Health Service.
- 1939–1941 – Fellowship in anaesthesia at the Mayo Clinic, Rochester, Minnesota, under John S. Lundy (1894–1973), an advocate of regional anaesthesia.
- 1941 – Returned to the US Marine Hospital, Staten Island, as Chief of Anaesthesia; the hospital functioned primarily as an obstetric unit caring for military families.
- 1941–1942 – In collaboration with obstetrician Waldo B. Edwards (1905-1981), adapted continuous spinal techniques to develop continuous caudal (epidural) analgesia via the sacral hiatus.
- 1942 – First clinical use of continuous caudal anaesthesia during labour and delivery; published early results demonstrating prolonged, controllable obstetric analgesia.
- 1943 – Publication of further papers on continuous caudal analgesia in obstetrics and surgery; introduced the Hingson–Edwards caudal needle.
- 1943–1945 – Director of Anaesthesia, Philadelphia Lying-In Hospital; published Control of Pain in Childbirth with Clifford Lull.
- 1945–1948 – Professor of Anaesthesiology, University of Tennessee, Memphis; established an obstetric caudal analgesia service.
- 1948–1951 – Associate Professor of Anaesthesia Research, Johns Hopkins University, Baltimore; introduced continuous lumbar epidural analgesia using ureteral catheters when caudal access was difficult.
- 1949 – Introduced lidocaine (lignocaine) into clinical use in the United States following visits to Scandinavia.
- Early 1950s – Invented the jet injector (Hypospray) after observing high-pressure transdermal injection injury in a merchant seaman.
- 1951 – Retired from the Public Health Service. Appointed Chairman of Anesthesiology, Case Western Reserve University, Cleveland, Ohio. Developed the Western Reserve Midget, a portable manual anaesthesia and resuscitation machine.
- 1956 – Began large-scale jet-injector immunisation programs in the United States (influenza, polio).
- 1958 – Led a global medical survey and vaccination missions. Founded Brother’s Keeper, later renamed the Brother’s Brother Foundation (BBF).
- 1962 – Directed a mass immunisation campaign in Liberia, vaccinating approximately 1 million people against smallpox, influencing WHO eradication strategies.
- 1968–1973 – Professor of Anaesthesiology and Public Health, University of Pittsburgh; Chief of Anaesthesiology, Magee-Womens Hospital. Permitted extended leave annually for international humanitarian missions.
- 1981 – Awarded the Gaston Labat Award by the American Society of Regional Anesthesia.
- 1987 – Received the President’s Volunteer Action Award from US President Ronald Reagan; nominated for the Nobel Peace Prize (humanitarian work).
- Died October 9, 1996 in Lake City, Florida, from complications of polymyositis.
Key contributions to neuraxial blockade
Introduction of continuous caudal analgesia
1941 – Inspired by the work of William Thomas Lemmon (1896-1974) on continuous spinal anaesthesia, Hingson, and obstetrician Waldo B. Edwards, introduced the continuous caudal technique. By maintaining access to the epidural space via the sacral hiatus, fractional doses of local anaesthetic could be administered over many hours, allowing the level, depth, and duration of analgesia to be titrated to clinical need.
Their first clinical series, published in 1943, demonstrated that labour could be conducted with sustained analgesia, preserved maternal consciousness, minimal haemodynamic disturbance, and good neonatal outcomes, overcoming many limitations of single-injection caudal and spinal techniques.
The Hingson–Edwards needle
A critical innovation in the development was the Hingson–Edwards malleable caudal needle. Unlike rigid steel needles, it was designed to follow the curvature of the sacral canal without kinking, lumen obstruction, or breakage.
The most important part of the apparatus is the malleable needle… constructed so that it will assume the curvature of the sacral canal for many hours under considerable stress without breakage and without obliteration of the lumen… In our series it has been used more than four hundred times without breakage. However, until experience has been sufficient to test the durability of the needle, we recommend that it be discarded after five complete labors and deliveries.
Hingson, Edwards 1943
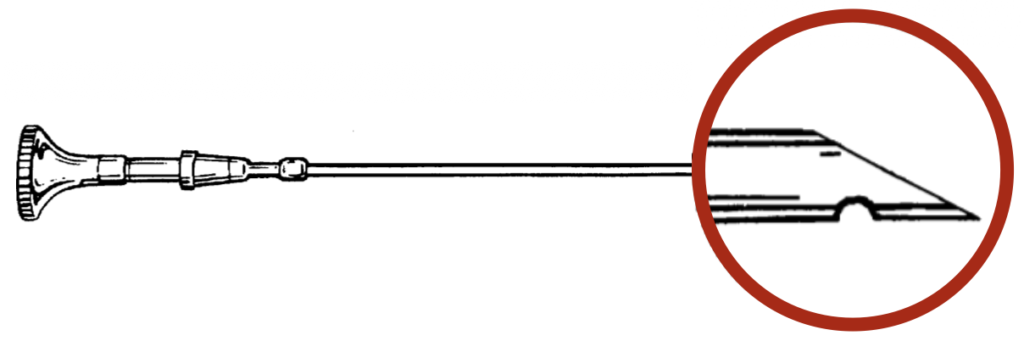
Technically, the needle combined rigid proximal and distal segments with an annealed, malleable mid-portion, allowing it to conform to sacral anatomy while maintaining control at the hub and tip. The tip was a short-bevel point with a relatively blunt cutting edge, supplemented by an additional side orifice near the tip to maintain flow even if the bevel abutted tissue. The hub incorporated a reinforced steel collar for secure attachment to small-bore tubing, and a safety bead designed to reduce the risk of needle fracture. Together, these features materially reduced complications associated with earlier rigid needles and made prolonged continuous caudal analgesia technically feasible.
Late 1940s: Extension to lumbar epidural analgesia
Hingson extended the principles of continuous neuraxial blockade beyond the sacral approach. When caudal access was anatomically difficult or undesirable, he used continuous lumbar epidural analgesia. Initially using ureteric catheters in the absence of purpose-built epidural equipment, this adaptation completed the shift from intermittent caudal block to modern continuous epidural anaesthesia.
Other key innovations and eponyms
Hingson Field Unit (Western Reserve Midget)
In the early 1950s, after becoming Chair of Anaesthesiology at Case Western Reserve University, Hingson collaborated with engineers to develop a portable anaesthesia and resuscitation device. The unit delivered a non-explosive gas mixture of cyclopropane, helium, and oxygen from thumb-sized cylinders, and could function as an anaesthesia machine, oxygen inhalator, or resuscitator. Weighing approximately 2 lb, it was designed for simplicity, portability, and safety, and used for obstetric, paediatric, dental, and emergency procedures.

B. Three-liter duck decoy rubber toy bag for inductions of anesthesia in babies and small children. Hingson 1958
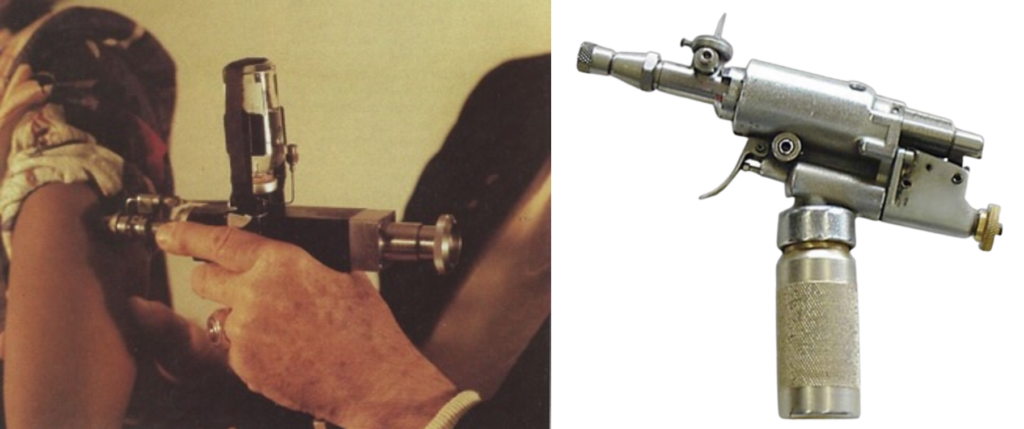
Hingson Peace Gun (jet injector)
While serving as Chief of Anaesthesia at the US Marine Hospital, Staten Island, Hingson treated a sailor who had accidentally injected diesel fuel under high pressure, leaving no visible skin wound. This observation led him to develop high-speed jet injectors, capable of delivering medications transdermally without needles. The device became widely known as the Hingson Peace Gun.
1956 – Hingson and his team began production-line immunisation, initially vaccinating children with the Salk polio vaccine in Cleveland, Ohio. The speed and economy of jet injection enabled mass vaccination campaigns, and by the late 1950s more than 300,000 patients patients had been immunised against polio and influenza. Through the Brother’s Brother Foundation, jet injectors were later used internationally, contributing to large-scale vaccination programmes in Asia, Africa, and Latin America.
Humanitarian and global health work
From the mid-1950s onward, Hingson directed his energy toward humanitarian medicine and global public health, applying medical innovation to large-scale relief rather than individual procedures. His interest in mass treatment was closely linked to the development of needle-free jet injection (Hingson Peace Gun), which made rapid, low-cost immunisation feasible in resource-limited settings.
1958 – Hingson founded Brother’s Brother Foundation, a non-profit organisation dedicated to delivering medical supplies, vaccines, and expertise to underserved populations worldwide. The foundation coordinated teams of physicians, nurses, and logisticians, often working in regions affected by poverty, natural disaster, or political instability. Hingson insisted that humanitarian medicine should be practical, scalable, and respectful of local healthcare systems, rather than episodic or purely symbolic.
Through the late 1950s and 1960s, Hingson led or advised mass immunisation campaigns using jet injectors in the United States, Africa, Asia, and Latin America. These programmes contributed to large-scale vaccination against polio, influenza, and smallpox, including a campaign in Liberia that immunised approximately one million people. His work influenced emerging international approaches to population-level disease control and aligned with early World Health Organization eradication strategies. In recognition of his humanitarian contributions, Hingson received multiple national and international honours and was later nominated for the Nobel Peace Prize.
Major Publications
- Edwards WB, Hingson RA. Continuous Caudal Anesthesia During Labor and Delivery. Anesthesia & Analgesia: 1942; 21(6): 301-311
- Edwards WB, Hingson RA. Continuous Caudal Anesthesia in Obstetrics. JAMA. 1943; 121(4): 225-229.
- Edwards WB, Hingson RA. Continuous Caudal Analgesia in Obstetrics – A Method for Safe, Painless Childbirth. JAMA. 1943; 121(4): 260-261
- Southworth JL, Hingson RA. Continuous Caudal Analgesia in Surgery. Ann Surg. 1943 Dec;118(6):945-70.
- Edwards WB, Hingson RA. The Present Status of Continuous Caudal Analgesia in Obstetrics. Bull N Y Acad Med. 1943 Jul;19(7):507-18.
- Hingson RA, Edwards WB. Comprehensive review of continuous caudal analgesia for anesthetists. Anesthesiology 1943; 4(2): 181-196.
- Lull CB, Hingson RA. Control of Pain in Childbirth: Anesthesia, Analgesia, Amnesia. 1944
- Hingson RA, Hughes JG. Clinical studies with jet injection; a new method of drug administration. Curr Res Anesth Analg. 1947 Nov-Dec;26(6):221-30.
- Hingson RA. The Western Reserve anesthesia mechaine, oxygen inhalator, and resuscitator. J Am Med Assoc. 1958 Jun 28;167(9):1077-82.
- Hingson RA, Pitkin WM. Hypodermic injection device. JAMA. 1963 Apr 27;184:319
- Hingson RA. World Anesthesia: Problems confronting emerging countries. Anesth Analg. 1964; 43: 610-9.
- Hingson RA. [The world-wide federation of anesthesiologists societies diffuses the education of anesthesia and emergency care through the continents]. Anesth Analg (Paris). 1969; 26(4): 459-69.
- Hingson RA, Pitkin WM. Delivery of anesthesia services throughout the world. Clin Anesth. 1974; 10(3): 265-80
References
Biography
- Saxon W. Robert Andrew Hingson, 83, A Pioneer in Public Health. NY Times Oct 12, 1996.
- Robert Hingson. University of Pittsburgh 1996; 29(5)
- Maltby R. Robert Andrew Hingson (1913-1996). Notable Names in Anaesthesia. The Choir Press; 2013: 95-98
Eponymous terms
- Lemmon WT. A method for continuous spinal anesthesia: a preliminary report. Ann Surg. 1940 Jan;111(1):141-4.
- Schorr MR. Needles. Some points to think about. I. Anesth Analg. 1966 Jul-Aug;45(4):509-13
- Schorr MR. Needles some points to think about. II. Anesth Analg. 1966 Sep-Oct;45(5):514-9.
- Schorr MR. Needles some points to think about. III. Anesth Analg. 1966 Sep-Oct;45(5):520-6.
- Bryant CE. Operation Brother’s Brother. 1968
- Bause G. Hingson’s Peace Gun. Anesthesiology, 2009; 111(1): 4.
- Jackson A, Edwards M. The Historical Development of Obstetric Anesthesia and Its Contributions to Perinatology. American Journal of Perinatology, 2017; 34(3): 211–216.
- Hingson Peace Gun. Wood Library museum
- Hingson Field Unit. Wood Library museum
- Our Founder. Brothers Brother Foundation
Eponym
the person behind the name
MBBS Newcastle University, UK. Currently working at Sir Charles Gairdner Hospital, Perth. Aspiring anaesthetist
BA MA (Oxon) MBChB (Edin) FACEM FFSEM. Emergency physician, Sir Charles Gairdner Hospital. Passion for rugby; medical history; medical education; and asynchronous learning #FOAMed evangelist. Co-founder and CTO of Life in the Fast lane | On Call: Principles and Protocol 4e| Eponyms | Books |

