R&R In The FASTLANE 071
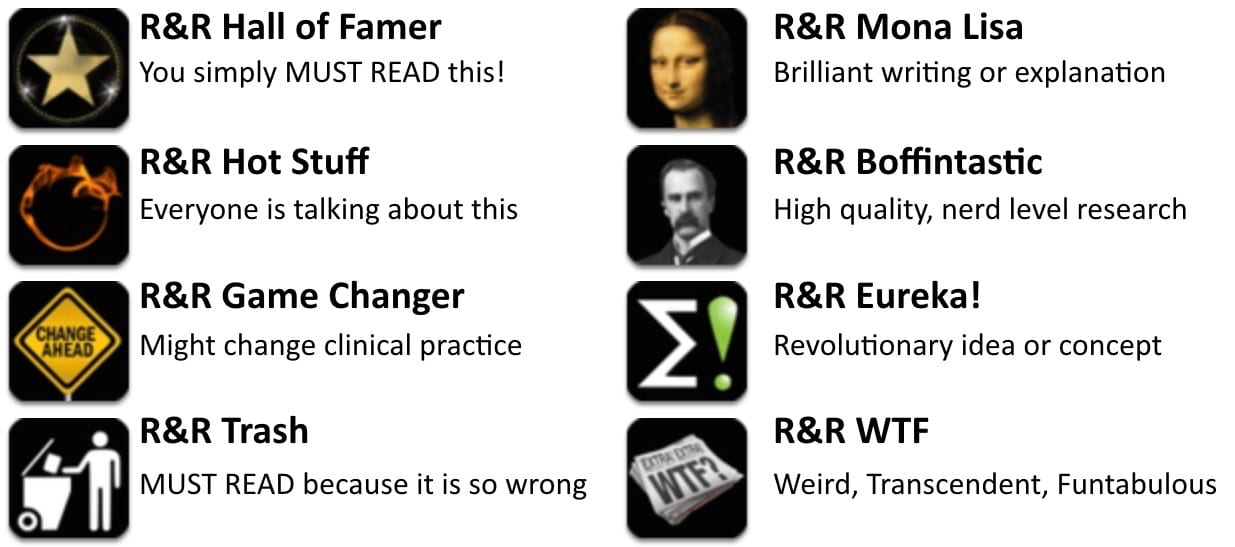
Welcome to the 71st edition of Research and Reviews in the Fastlane. R&R in the Fastlane is a free resource that harnesses the power of social media to allow some of the best and brightest emergency medicine and critical care clinicians from all over the world tell us what they think is worth reading from the published literature.
This edition contains 7 recommended reads. The R&R Editorial Team includes Jeremy Fried, Nudrat Rashid, Soren Rudolph, Anand Swaminathan and, of course, Chris Nickson. Find more R&R in the Fastlane reviews in the : Overview; Archives and Contributors
This Edition’s R&R Hall of Famer
Holcomb JB et al. Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma: the PROPPR randomized clinical trial. JAMA 2015; 313(5):471-82. PMID 25647203
- The much awaited PROPPR trial – an enormous logistic accomplishment – successfully randomised 680 severely injured patients to a transfusion strategy of either 1:1:1 or 1:1:2 (plasma:platelets:RBCs) in 12 different level 1 trauma centers. Among these patients there was no significant difference in 24 hour or 30 day mortality when comparing the two strategies. BUT, the study was powered to detect an absolute difference in outcome of 10 %! Just look at the Kaplain-Meier Failure Curves for Mortality – they seem to send a clear signal.
- Read More: The Adventure of the Blanched Soldier (EM Nerd); The PROPPR Randomized Clinical Trial (REBEL EM)
- Recommended by Søren Rudolph
Shahrami A, et al. Comparison of therapeutic effects of magnesium sulfate vs. dexamethasone/metoclopramide on alleviating acute migraine headache. J Emerg Med 2015; 48(1): 69-76. PMID 25278139
- Does IV magnesium have a role in the management of acute migraine headache in the ED? A new study says yes. Compared to dexamethasone + metoclopramide (fair comparator?), magnesium sulfate was more effective in decreasing pain severity at 20-min and 1-h and 2-h intervals after treatment (p < 0.0001).
- Recommended by Bryan Hayes
Kline JA et al. Decreased facial expression variability in patients with serious cardiopulmonary disease in the emergency care setting. Emerg Med J 2015; 32(1): 3-8. PMID: 25022275
- An important pilot study attempting to objectify what we mean when we use the word “gestalt”. Kline and others looked at facial expression variability and their findings suggest a relationship between a lack thereof, and serious disease. While this may not be a shocking finding, it’s an important first step in an attempt to be able to quantify, teach, and possible objectively use this data in the clinical setting. A preliminary study which will hopefully generate further research into this important area of work.
- Recommended by Jeremy Fried
Elif Yaka et al. Comparison of the Glasgow-Blatchford and AIMS65 Scoring Systems for Risk Stratification in Upper Gastrointestinal Bleeding in the Emergency Department. Acad Emerg Med 2014; 22: 23–30. PMID 25556538
- A comparison of the Glasgow-Blatchford (GBS) and AIMS65 scoring systems in UGIB patients in the ED population found the GBS to be more sensitive and have a higher negative predictive value for needed interventions in the low risk population. Like many studies examining clinical decision tools and scoring instruments, it was unfortunately not compared to the clinician’s prediction of expected clinical course, or gestalt. A well done study comparing the two scores, and important for ED providers to be aware of, nonetheless.
- Recommended by Jeremy Fried
Thomas DG et al. Benefits of Strict Rest After Acute Concussion: A Randomized Controlled Trial. Pediatrics 2015. PMID 25560444
- Despite sparse evidence of long-term outcome improvement in pediatric patients, cognitive rest, coupled with physical rest and graduated return to play, is the mainstay of concussion treatment and recommended by major societies. How strict this “rest” should be is debatable, but this RCT in patients age 11-22 showed no benefit in short term outcomes from “strict” rest versus usual care (varied, but 1-2 days rest and then graduated return to activities). This contribution suggests that restrictions (no school, work, or physical activity) patients feel from strict rest may engender more emotional symptoms than general rest. Prescribe rest to patients and make sure they follow up, but maybe we don’t have to be quite so strict.
- Recommended by Lauren Westafer
Shavit I et al. Sedation for children with intraoral injuries in the emergency department: a case-control study. Pediatr Emerg Care 2014; 30(11): 805-7. PMID 25343735
- Procedural sedation & analgesia for intra oral procedures (IOP) such as lacerations, I&D and aspirations is generally considered with a higher risk of Serious Adverse Events During Sedation (SAEDS). This papers compares 38 cases (sedation for IOP) with 41 controls (sedation for forearm fracture reduction) in terms of SAEDS (apnea, hypoxemia (oximetry <93%), hypoventilation, laryngospasmand other upper airway obstruction). Both groups have similar sedation strategies and events; 5 hypoxic/2 apneas in cases vs. 4 hypoxic/2 apneas in control. This papers appears to show that IOP have similar risk of SAEDS compared to sedation for non IOP procedures.
- Recommended by Daniel Cabrera
Benato P et al.Ultrasound guided chest compressions during cardiopulmonary resuscitation. Resuscitation. 2015; 87: e13-4. PMID 25497391
- Findings from transesophageal echocardiography during CPR suggest that narrowing of the base of left ventricle and of the aorta root may be an indicator of quality of chest compressions. This small case series analyse 6 patients with non-traumatic cardiac arrest using transthoracic US to evaluate the possibility to check the efficacy of chest compressions and to guide changes of hands position in order to improve heart contractility. In 3 out of 6 cases chest compressions were deemed not satisfactory and changes of hands positions guided by US subsequently improved the quality of chest compressions. In the other 3 cases the compression of left ventricle was deemed good and no changes were made. Importantly all US examinations were conducted without interferences with normal standard of care. The authors state that these observations indicate that changes of hands position guided by US could improve the quality of CPR and this area deserves attention and consideration in the future.
- Recommended by Søren Rudolph
Patel MS et al. Association of the 2011 ACGME Resident Duty Hour Reforms With Mortality and Readmissions Among Hospitalized Medicare Patients. JAMA 2014; 312(22): 2364-73. PMID 25490327
- Duty hour rules and regulations are pervasive in US medical training. This study looks at the effect of institution of duty hour restrictions on the outcome of Medicare patients. Although the study is retrospective and derived from large database information, it gives us a peak into the bigger picture of duty hours regulations: patient outcomes. The study authors found no difference in any important outcomes. It is similarly unclear whether these restrictions have improved resident quality of education or quality of life. Large system wide changes duty hour restrictions should, in the future, be implemented not based on theory but actual data of improved outcomes. An accompanying editorial delves into this issue and others.
- Recommended by Anand Swaminathan
Senior Consultant Anesthesiologist, Traumemanager and PHEM doctor. Dedicated to trauma resuscitation, prehospital care and airway management. Barometerbarn | @SorenRudolph |







Magnesium in migraine, another use for magnesium, quite interesting. Can’t get hold of the research paper as it would be nice to scruitinise methods, however single country, small numbers with fantastic results, it all makes me a bit worried about starting using magnesium for migraines in my department. Maybe I’ll give the usual combination: Metoclorpromide, 1L saline iv, an analgesic of patient’s choice, stick them in a dark side room and get myself busy with really sick patients for a couple of hours, buying my time till migraine goes away, for now at least.