R&R In The FASTLANE 111
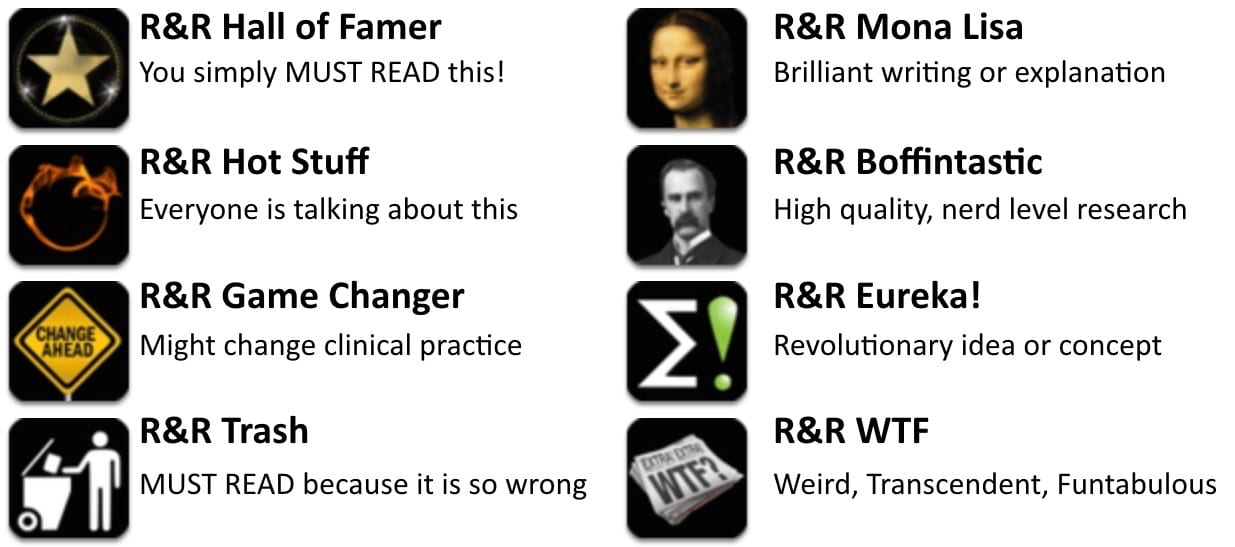
Welcome to the 111th edition of Research and Reviews in the Fastlane. R&R in the Fastlane is a free resource that harnesses the power of social media to allow some of the best and brightest emergency medicine and critical care clinicians from all over the world tell us what they think is worth reading from the published literature.
This edition contains 6 recommended reads. The R&R Editorial Team includes Jeremy Fried, Nudrat Rashid, Soren Rudolph, Anand Swaminathan and, of course, Chris Nickson. Find more R&R in the Fastlane reviews in the : Overview; Archives and Contributors
This Edition’s R&R Hall of Famer
Marik P, Bellomo R. A rational approach to fluid therapy in sepsis. Br J Anaes 2015. PMID: 26507493
- In the wake of ProCESS, ARISE and PROMISE, the 3 trials that finally put ‘Early Goal Directed Therapy’ to bed, how should we manage the fluid state of patient’s with septic shock? This opinionated review by two of the biggest brains in the business, Marik and Bellomo, suggests a haemodynamically guided, restricted fluid resuscitation strategy largely based on known physiology and what science currently offers us. ScvO2, CVP and lactate all get bashed (as expected).
- Assessment of fluid responsiveness and assessment of the risk-benefit of fluid boluses is emphasised, as is the role of early noradrenaline infusions. Saline gets dealt with harshly IMO, especially given the recent SPLIT trial’s finding that low volume saline administration in ‘all comer’ ICU patients appears safe. A great read – provocative and largely convincing (until the next big trial at least).
- Recommended by: Chris Nickson
Peterson N et al. Size matters: how accurate is clinical estimation of traumatic wound size? Injury. 2014; 45(1): 232-6. PMID: 22592151
- Interestingly, male physicians overestimate wound size and female physicians underestimate. Wonder what Freud would have to say about it.
- Recommended by: Seth Trueger
Aldous S et al. The incremental value of stress testing in patients with acute chest pain beyond serial cardiac troponin testing. Emerg Med J 2015. PMID: 26511125
- Thousands ruled-out, hundreds stress tested – and only a handful of true positives and just as many false positives.
- Recommended by: Ryan Radecki
- Read More: What Did We Find on Stress Testing? (EM Lit of Note)
Boutis K et al. The Diagnosis of Concussion in a Pediatric Emergency Department. J Pediatr 2015; 166(5):1214-20. PMID: 25919731
- This study from Canada looked at the ED diagnosis of concussion in a convenience sample of 495 kids within 2 weeks of head injury and found that compared to the Zurich criteria, ED physicians underdiagnosed concussion. ED physicians diagnosed concussion in 40.4% of the patients, while the Zurich criteria for concussion were fulfilled by 89.5%. Concussion was more likely to be diagnosed in kids >10 years old, those playing collision sports, those with an injury >1 day prior, or 3+ symptoms. This criteria, in this case defined by SCAT3 (not validated in all head trauma/cumbersome in ED), may represent another area of overdiagnosis as it’s not clear what impact this diagnosis has on patient oriented outcomes.
- Recommended by: Lauren Westafer
Doluoglu OG et al. Can sexual intercourse be an alternative therapy for distal ureteral stones? A prospective, randomized, controlled study. Urology 2015; 86(1):19-24. PMID: 26142575
- Forget the tamsulosin. In this small study, sex 3 times/week doubled the rate of stone passage in comparison to tamsulosin or placebo (83.9% vs. 47.6% vs. 34.8%). The study brings up more methodologic issues that we can address (blinding? sham-sex arm? confirmation of sex? prohibiting intercourse/masturbation in other groups) but we’d all like to believe this to be true. Finally, some “busy” work we can send patients home with. PS: only men included in the study.
- Recommended by: Anand Swaminathan
de Lange DW et al. Extracorporeal membrane oxygenation in the treatment of poisoned patients. Clin Toxicol 2013; 51: 385-393. PMID: 23697460
- Veno-venous extracorporeal membrane oxygenation (VV ECMO) is used for refractory respiratory failure, while veno-arterial (VA) ECMO is used for refractory cardiopulmonary failure. Indications for VV ECMO have included severe ARDS and status asthmaticus, and VA ECMO has been used after massive MI and poisoning by cardiotoxic drugs. This article reviews techniques, indications, contraindications and complications of VV and VA ECMO. A literature review of ECMO in poisoned patients is also included.
- Recommended by: Meghan Spyres
New Jersey Emergency Physician with academic focus on resident education and critical care in the ED. Strong supporter of FOAMed and its role in cutting down knowledge translation | @EMSwami |