Seafood poisoning
aka Toxicology Conundrum 036
A 31 year-old man and his 27 year-old wife present to the emergency department a few hours after eating at a seafood restaurant. In addition to nausea and vomiting, they both complain of altered sensation affecting their hands and feet. Both patients were previously well.
Questions
Q1. Based on the limited clinical information, what types of seafood poisoning syndromes could be affecting these patients?
Answer and interpretation
Numerous types of seafood poisoning can cause symptoms of gastroenteritis and paraesthesiae (abnormal skin sensations like ‘pins and needles’)
The differential diagnosis includes:
- Amnestic shellfish poisoning
- Ciguatera poisoning
- Neurotoxic shellfish poisoning
- Palytoxin poisoning
- Paralytic shellfish poisoning
- Tetrodotoxin poisoning
Other types of seafood food poisoning cause gastroenteritis, but do not specifically cause paraesthesiae:
- diarrhetic shellfish poisoning
- scombroid poisoning
- bacterial food poisoning
Paraesthesiae could also be caused by secondary alkalemia:
- hyperventilation-induced respiratory alkalosis, or
- vomiting-induced metabolic alkalosis
Q2. If one of the patients complains that the cold bed rails in the emergency department are “burning hot”, what would be the likely diagnosis and why?
Answer and interpretation
Ciguatera poisoning
Hot-cold reversal, better termed cold allodynia, is considered almost pathognomonic of ciguatera poisoning (other dinoflagellate toxins such as palytoxin may mimic ciguatoxin). The phenomenon is probably not a true reversal of temperature sensation, rather pain sensation is altered such that cold is experienced as a burning pain. The mechanism for this is obscure.
Q3. What toxin is responsible for each of the following seafood poisoning syndromes?
Amnestic shellfish poisoning
Domoic acid (stimulates glutamate receptors)
Ciguatera poisoning
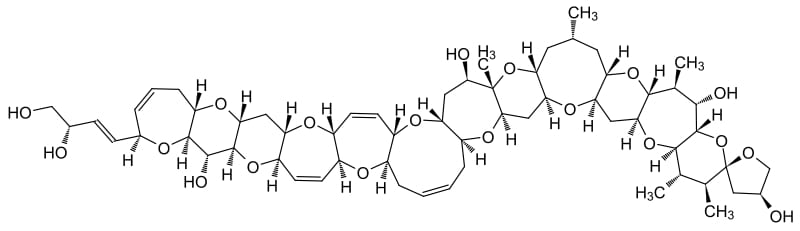
Ciguatoxin (a family of toxins that cause sodium channel activation and the stimulation of cholinergic receptors)
Diarrhetic shellfish poisoning
Various diarrhetic toxins: okadeic acid, azaspiracid, dinophysitoxins (and no, I didn’t make these words up…)
Neurotoxic shellfish poisoning
Brevetoxin
Palytoxin poisoning
Palytoxin/ clupetoxin (a potent vasoconstrictor that alters sodium and potassium flux across cell membranes)
Paralytic shellfish poisoning
Saxitoxin (a potent sodium channel blocker that may be lethal in <1mg doses — a contaminated mussel may contain 20mg of saxitoxin!)
Scombroid poisoning
Scombrotoxin (biogenic amines produced from histidine breakdown)
Tetrodotoxin poisoning
Tetrodotoxin (sodium channel blocker)
Q4. What are the typical clinical features for each of the following seafood poisoning syndromes?
Amnestic shellfish poisoning
- Gastroenteritis, mutism, myoclonus, headaches, seizures, coma.
- Hypotension and bronchorrhea may occur.
- Chronic peripheral neuropathies and memory impairment
Ciguatera poisoning
- Vomiting and watery diarrhoea, ‘hot-cold reversal’ (cold allodynia), headache, paraesthesiae of the mouth and extremities, pruritis, myalgias, weakness; rarely seizures and respiratory arrest.
- Chronic paraesthesiae, pruritis and neuropsychiatric symptoms last for years in some patients
Diarrhetic shellfish poisoning
- Vomiting, abdominal cramps, and severe diarrhoea
Neurotoxic shellfish poisoning
- Gastroenteritis, ataxia, paresthesiae, seizures
Palytoxin poisoning
- Gastroenteritis, paraesthesiae, ataxia, respiratory paralysis
Paralytic shellfish poisoning
- Gastroenteritis, paresthesiae, severe muscle spasms, rhabdomyolysis, hypertension, seizures, respiratory distress, myocardial injury
Scombroid poisoning
- Gastroenteritis, flushed skin, hypotension, urticaria, wheezing
Tetrodotoxin poisoning
- Vomiting, paraesthesiae, muscle twitching, diaphoresis, bradycardia, flaccid paralysis, respiratory paralysis
Q5. Eating what type of seafood typically causes each of the following seafood poisoning syndromes?
Amnestic shellfish poisoning
- mussels, clams, anchovies
Ciguatera poisoning
- reef fish such as: barracuda, red snapper, grouper
Diarrhetic shellfish poisoning
- bivalve mollusks
Neurotoxic shellfish poisoning
- bivalve mollusks, whelks
Palytoxin poisoning
- parrotfish, crabs, mackerel, sardines
Paralytic shellfish poisoning
- bivalve shellfish affected by ‘red tide’ dinoflagellates
Scombroid poisoning
- tuna, mahi-mahi, bonito, mackerel
Tetrodotoxin poisoning
- pufferfish, sunfish, porcupinefish, others…
Q6. How long after ingestion does the onset of clinical features of toxicity occur for each of the following seafood poisoning syndromes?
Amnestic shellfish poisoning
- minutes to hours
Ciguatera poisoning
- 1 to 6 hours (or longer in mild cases)
Diarrhetic shellfish poisoning
- 30 minutes to 2 hours
Neurotoxic shellfish poisoning
- minutes to 3 hours
Palytoxin poisoning
- hours
Paralytic shellfish poisoning
- <30 minutes
Scombroid poisoning
- minutes to hours
Tetrodotoxin poisoning
- <1 hour
Q7. What is the ultimate source of toxin for most seafood poisoning syndromes?
Answer and interpretation
Dinoflagellates
Dinoflagellates are tiny flagellated protists. They are marine plankton that are eaten by mollusks and fish. They produce various toxins that accumulate in the food chain, when one species eats another on a lower rung of the predatory ladder. For instance, the dinoflagellate Gambierdiscus toxicus produces ciguatoxin. Other dinoflagellates may form algal blooms called ‘red tides’, which are associated with outbreaks of shellfish poisoning.
The toxins that cause scombroid and tetrodotoxin poisoning are not produced by dinoflagellates.
Concerns have also been raised about the safety of eating fish given the accumulation of toxins such as mercury, dioxin and PCBs in the food chain. Overall, the health benefits of including fish in one’s diet exceeds any risks.
New dinoflagellate toxins will undoubtedly be discovered in the future — this post is cannot hope to be comprehensive.
Q8. How is the toxin that causes scombroid produced?
Answer and interpretation
Scombrotoxin consists of histamine (and probably other biogenic amines) produced by the breakdown of histidine in the muscles of poorly refrigerated fish.
Hence the symptoms can mimic an allergic reaction.
The conversion of fish muscle histidine to histamine is enzymatically catalysed by histidine decarboxylase produced by the gram-negative bacterium Morganella morganii. This occurs at temperatures above 16C. Histamine is heat stable, so scombroid poisoning can occur even when poorly refrigerated fish has been properly cooked.
Q9. How is it possible that tetrodotoxin is found in species as diverse as a newt, the blue-ringed octopus and puffer fish?
Answer and interpretation
Tetrodotoxin is produced by bacteria, such as Vibro alginolyticus, that coexist with many different animal species.
Tetrodotoxin is found in:
- fish — pufferfish, sunfish, angelfish.
- amphibians — toads and newts (aka tarichatoxin)
- invertebrates — ribbon worms, arrow worms, flatworms
- mollusks — blue-ringed octopus (aka maculotoxin), xanthid crabs, sea slugs
Q10. Is the taste of seafood resulting in seafood poisoning syndromes altered?
Answer and interpretation
In most cases of seafood poisoning the taste of the seafood is not altered.
There are exceptions, such as the fish responsible for:
- scombroid poisoning — may taste peppery
- palytoxin poisoning — may taste bitter
Q11. Describe the management of toxic seafood poisoning, including specific therapies that may be beneficial for specific types of seafood poisoning.
Answer and interpretation
As always, initial resuscitation and ongoing supportive care are the mainstays. Most cases are self-limiting and not life-threatening.
Resuscitation and supportive care
- intubation and ventilation may be required for respiratory depression, coma or seizure control
- fluid resuscitation for hypotension and/or shock resulting from gastroenteritis or cardiovascular toxicity
- bradycardia may require treatment with atropine (e.g. tetrodotoxin poisoning)
- benzodiazepines for seizure control
- antiemetics for nausea and vomiting
- analgesia for abdominal cramps or muscle pain
- observation for 6 hours to monitor for the delayed onset of symptoms
Decontamination
- not usually indicated
- activated charcoal may be given in potentially life-threatening seafood poisoning (e.g. following pufferfish ingestion)
Specific therapy may be required for:
Scombroid poisoning
- Symptomatic treatment with antihistamines. Bronchodilators are rarely required.
- Very rarely the presentation may mimic anaphylaxis requiring adrenaline.
Ciguatera poisoning
- Mannitol (0.5-1g/kg IV, ideally within 72 hours of symptom onset) is still recommended by some experts despite a double-blind randomised controlled trial that found no benefit*. […this study did have flaws: most cases were given mannitol late, the subgroup analysis of those receiving mannitol early (within 24 hours) was underpowered and case diagnoses were not confirmed by toxin assays of fish samples.]
- Mannitol’s beneficial effects (if any) may be related to a decrease in neuronal edema, free radical scavenging or sodium/ potassium channel modulation. Mannitol will induce an osmotic diuresis and should only be administered following adequate rehydration of the patient.
- Chronic neuropsychiatric symptoms may respond to fluoxetine, and neuropathic pain may respond to amitriptyline and/or gabapentin. The evidence base for these treatments is purely anecdotal.
- Patients need to be aware of precipitants that may trigger a relapse — potential triggers include: ethanol, eating fish and other various other foods (including caffeine, nuts, chicken and pork), dehydration and over-exertion. Potential triggers should be avoided for 6 months following symptom resolution.
References
- Brett MM. (2003) Food poisoning associated with biotoxins in fish and shellfish. Current Opinion in Infectious Diseases, 16(5), 461-5. PMID: 14501999
- Friedman MA, et al (2008). Ciguatera fish poisoning: treatment, prevention and management. Marine Drugs, 6 (3), 456-79 PMID: 19005579
- Lawrence DT, et al. (2007) Food poisoning. Emergency Medicine Clinics of North America, 25(2), 357. PMID: 17482025
- Mozaffarian D, Rimm EB. (2006) Fish intake, contaminants, and human health: evaluating the risks and the benefits. JAMA, 296(15), 1885-99. PMID: 17047219
- Olson, K. Poisoning and Drug Overdose (5th edition). McGraw-Hill, 2006.
- Schnorf H, Taurarii M, Cundy T. (2002) Ciguatera fish poisoning: a double-blind randomized trial of mannitol therapy. Neurology, 58(6), 873-80. PMID: 11914401
- Watkins SM, et al. (2008) Neurotoxic shellfish poisoning. Marine drugs, 6(3), 431-55. PMID: 19005578
Video References

CLINICAL CASES
Toxicology Conundrum
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
