Sheehan Syndrome
Description
Postpartum hypopituitarism following ischaemic necrosis of the anterior pituitary gland. Pituitary necrosis occurs secondary to hypophyseal portal vessel thrombosis following significant postpartum haemorrhage, hypovolaemia, and shock.
Hypopituitarism leads to impaired of thyroid, adrenal and ovarian function. Early clinical features includes failure to lactate, breast involution, and amenorrhoea. Delayed features include loss of axillary/pubic hair, breast/genital atrophy and signs and symptoms of hypothyroidism and adrenal insufficiency.
The association of pituitary necrosis with postpartum shock was first described in 1937 by Harold Leeming Sheehan (1900-1988). Sheehan reported on the pathogenesis and consequences of postpartum pituitary necrosis in more than ten publications between 1937 and 1968
History
1913 – Polish pathologist Leon Konrad Glinski (1870-1918) described two cases of women who died following pregnancy both demonstrating extensive pituitary necrosis at post mortem.
- Case 1: a 37-year-old woman who died of generalised sepsis nine days after a cesarean section.
- Case 2: a 33-year-old woman who died of heart failure 6 weeks following miscarriage at six months with significant uterine haemorrhage
The extensive necrosis was attributed to thrombosis in the hypophyseal arteries. Glinski concluded that if the process were extensive, it could affect pituitary function
1914 – German physician and pathologist, Morris Simmonds (1855-1925) described a case of chronic hypopituitarism in a woman who died 11 years after surviving severe puerperal sepsis following the birth of her fifth child. Autopsy revealed the pituitary was severely atrophied. Simmonds proposed pituitary necrosis secondary to mycotic bacterial emboli.
Eine bis dahin gesunde Frau erkrankt an schwerer Puerperalsepsis. Sie erleidet eine septische Nekrose des Hirnanhangs. Infolge des Verlustes dieses lebenswichtigen Oigans treten schwere Ausfallserscheinungen: Menopause, Muskel-schwäche, Schwindel und Bewußtlosigkeitsanfälle, Anämie, rasches Altern, kurzum, ein „Senium praecox” ein. Die Testierenden intakten Drüsenfragmente atrophieren allmählich in dem umgebenden Bindegewebe. Das Organ wird absolut insuffizient, die Frau geht im Koma zugrunde. Die Sektion ergibt als einzige Todesursache einen fast totalen Schwund der Hypophysis.
A previously healthy woman becomes ill with severe puerperal sepsis. She suffers septic necrosis of the pituitary gland. As a result of the loss of this vital organ, severe symptoms occur: menopause, muscle weakness, dizziness and spells of unconsciousness, anemia, rapid aging – in short, “senium praecox.” The remaining intact glandular fragments gradually atrophy in the surrounding connective tissue. The organ becomes completely insufficient, and the woman dies in a coma. Autopsy reveals the sole cause of death to be almost total atrophy of the pituitary gland.
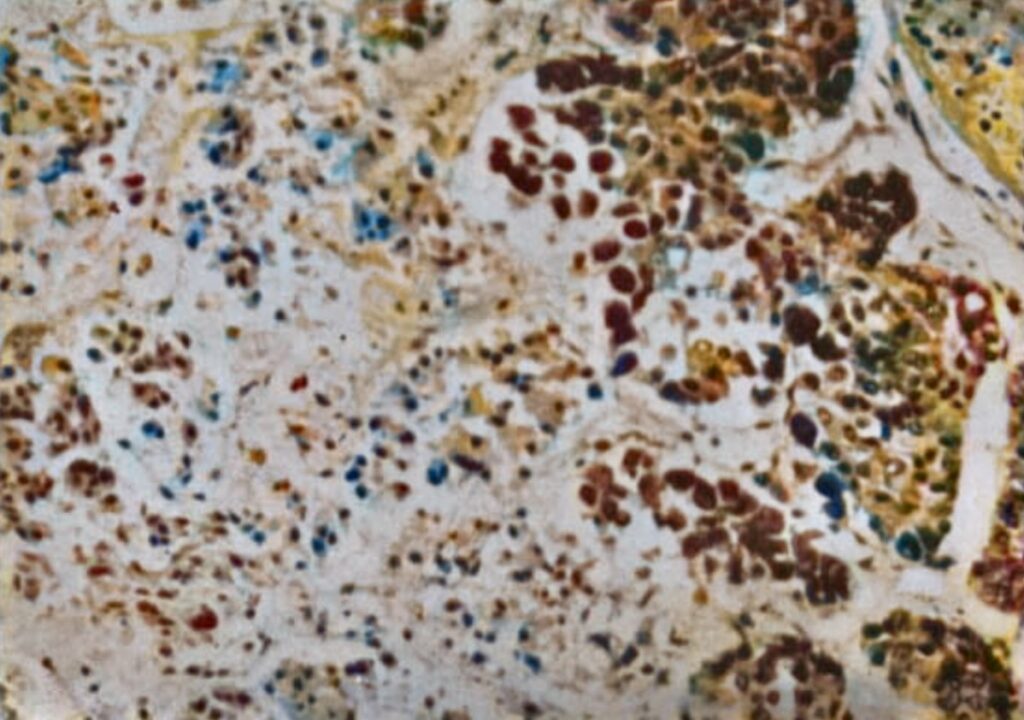
Simmonds went on to study the histology of pituitary glands obtained from patients who died from septicaemia [1916]. He noted that acute focal necrosis from bacterial emboli was common; in patients who survived the acute illness, this necrosis transformed to fibrous atrophy, leading to pituitary hypofunction. He noted that these patients were profoundly emaciated and described the clinical picture as ‘hypophyseal cachexia‘, a term used interchangeably with Simmonds disease for pituitary necorsis/hypofunction in males or females suffering septicememia and unrelated to postpartum complications
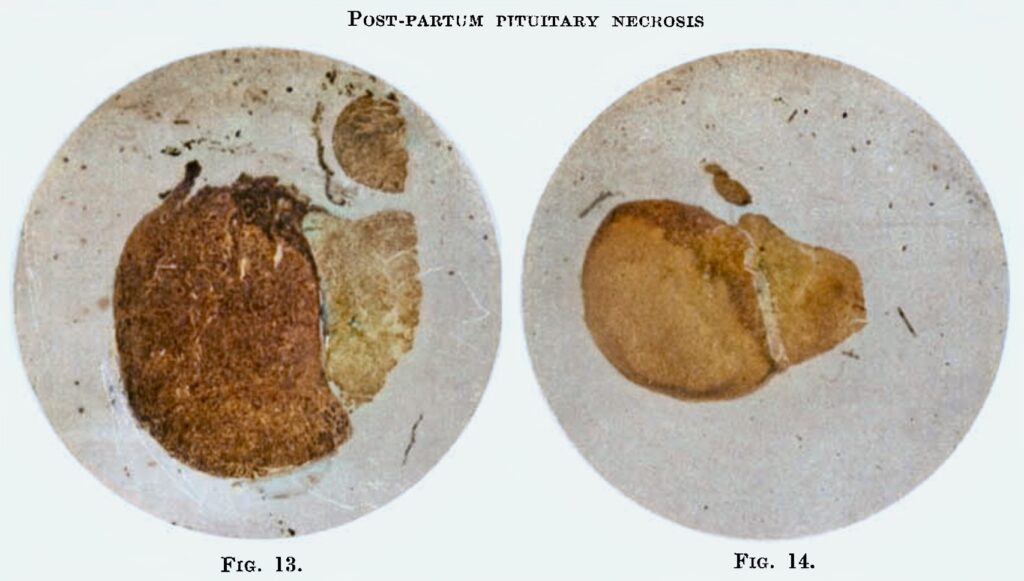
1937 – Sheehan performed a series autopsies of women who had died in late pregnancy, at delivery, or in the puerperium working as a pathologist at Glasgow Royal Maternity Hospital. Sheehan reported 12 of 76 women had extensive destruction of the anterior pituitary and that the common clinical feature was haemorrhagic shock rather than sepsis. He proposed that pituitary necrosis was due to spasm or thrombosis of the arteries to the pituitary rather than from mycotic emboli.
Sheehan also analysed all the previously reported cases of postpartum pituitary necrosis in the literature to demonstrate obstetric haemorrhage as the probable cause, rather than sepsis. He found that even with scant obstetric details in most reports 6 out of the 10 reports were associated with significant obstetric haemorrhage.
1949 – Sheehan and Vincent Kirwan Summers (1914-1975) published in the Quarterly Journal of Medicine on the syndrome of hypopituitarism. The paper demonstrated that emaciation and premature senility (previously considered to be essential for the diagnosis of pituitary insufficiency), were not features of the syndrome.
This paper, rather than Sheehan’s earlier papers on pituitary necrosis, prompted global acceptance of the term ‘Sheehan syndrome’ to describe the syndrome of postpartum pituitary necrosis
Associated Persons
- Leon Konrad Glinski (1870-1918)
- Morris Simmonds (1855-1925)
- Harold Leeming Sheehan (1900-1988)
Alternative names
- Postpartum pituitary necrosis
- Glinski syndrome; Reye syndrome;
- Sheehan’s syndrome
- Simmonds syndrome
References
Historical references
- Glinskí LZ. Kazuistiky zmian anatomopatologicznych w paszysadce mózgomej. Przegla̧d Lekarski, 1913; 52: 13–14
- Glinski LK. Anatomische veranderungen der hypophyse. [On Pituitary Atrophy with Fatal Outcome.] Deutsche medizinische Wochenschrift 1913; 39(1): 473.
- Simmonds M. Über Hypophysischwund mit tödlichem Ausgang. Deutsche medizinische Wochenschrift 1914; 40: 322-323
- Simmonds M. Uber kachexie hypophysaren ursprungs. Deutsche medizinische Wochenschrift 1916; 42: 190–91 [Simmonds syndrome]
- Reye E. Die ersten klinischen Symptome bei Schwund des Hypophysenvorderlappens (Simmondssche Krankheit) und ihre erfolgreiche Behandlung. Deutsche Medizinische Wochenschrift, 1928; 54: 696-697
- Sheehan HL. Post-partum necrosis of the anterior pituitary. The Journal of Pathology and Bacteriology 1937; 45(1): 189-214
- Sheehan HL, Murdoch R. Post-partum necrosis of the anterior pituitary: Pathological and clinical aspects. J Obstet Gynaecol Br Emp 1938; 45: 456-472
- Sheehan HL. Post-Partum Necrosis of the Anterior Pituitary. Trans Edinb Obstet Soc. 1938;58:13-28.
- Sheehan HL. Simmonds’s disease due to post-partum necrosis of the anterior pituitary. Quarterly Journal of Medicine, Oxford. 1939; 8(4): 277–309
- Sheehan HL, Summers VK. The syndrome of hypopituitarism, Quarterly Journal of Medicine, Oxford, 1949; 18(4): 319–378
Eponymous term review
- Kovács K. Necrosis of anterior pituitary in humans. I. Neuroendocrinology. 1969;4(3):170-99.
- Kovács K. Necrosis of anterior pituitary in humans. II. Neuroendocrinology. 1969;4(4):201-41.
- Gonzalez JG, Elizondo G, Saldivar D, Nanez H, Todd LE, Villarreal JZ. Pituitary gland growth during normal pregnancy: an in vivo study using magnetic resonance imaging. Am J Med. 1988 Aug;85(2):217-20
- Kovacs K. Sheehan syndrome. Lancet. 2003 Feb 8;361(9356):520-2.
- Tessnow AH, Wilson JD. The changing face of Sheehan’s syndrome. Am J Med Sci. 2010; 340(5): 402-6.
- Karaca Z, Laway BA, Dokmetas HS, Atmaca H, Kelestimur F. Sheehan syndrome. Nat Rev Dis Primers. 2016 Dec 22;2:16092
- Schury MP, Adigun R. Sheehan Syndrome. 2021 Sep 8. In: StatPearls [Internet].
eponymictionary
the names behind the name
BSc (Hons) MBBS, St George’s University of London. Foundation training at St George's University Hospitals NHS Foundation trust and Kingston NHS Foundation trust. RMO in Emergency Medicine at the Sir Charles Gairdner Hospital, Perth preparing for emergency training. When I'm not working I enjoy spending my time outdoors sailing, diving and hiking and hope to combine these passions with my career, pursuing interests in expedition and barometric medicine within my ED work.
BA MA (Oxon) MBChB (Edin) FACEM FFSEM. Emergency physician, Sir Charles Gairdner Hospital. Passion for rugby; medical history; medical education; and asynchronous learning #FOAMed evangelist. Co-founder and CTO of Life in the Fast lane | On Call: Principles and Protocol 4e| Eponyms | Books |

