Stingray envenoming
aka Toxicology Conundrum 012
While riding in a boat off the North Queensland coast a 12 year-old boy was struck by a large fish that had catapulted itself out of the water. The fish was a ray of unknown type, with a wingspan of about 1 m. The boy immediately complained of pain in his chest and difficulty breathing. His companions noticed a wound next to his left nipple, as well as another puncture wound near his left knee. He was taken to shore and and arrived at the nearest medical clinic 30 minutes after the time of injury. [Case based on Fenner et al 1989]

Questions
Q1. Where are stingrays found and what types are there?
Answer and interpretation
Rays are the largest type of venomous fish. They are flat-bodied and cartilaginous. They are among the commonest causes of fish-related injury and/or envenoming worldwide (e.g. over 200 cases per year in the United States). Injury is usually the result of traumatic contact with the stinging barb(s) of the animal’s tail.
Numerous species are found in waters all around Australia. Rays are also found in temperate and tropical waters worldwide, including tropical freshwater systems in South America, Africa, and South East Asia.
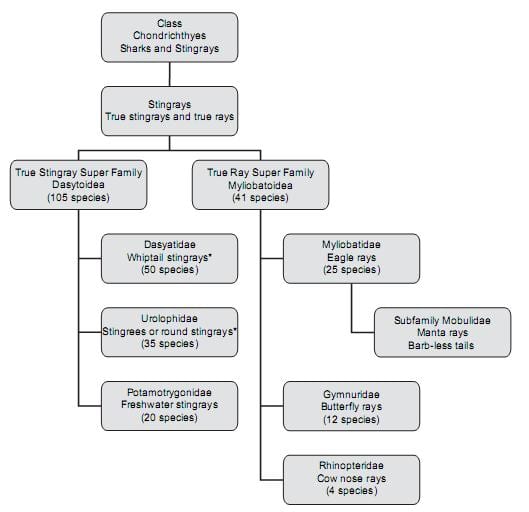
Classification of the 150 plus species of ray is controversial, but the major types of “true rays” (Rajiformes) include:
- “True” Stingrays (Family Dasytididae)
- Stingrees or round stingrays (Family Urolophidae)
- Butterfly rays (Family Gymnuridae)
- Sixgill stingrays (Family Hexatrygonidae)
- Eagle, Bull, Devil, Manta and Cownose rays (Family Myliobatidae)
- Deepwater stingrays (Plesiobatidae)
- River stingrays (Potamotrygonidae)
Q2. How do ray injuries and envenomings occur?
Answer and interpretation
Stingrays have acquired an undeserved notoriety, particularly following the death of Steve Irwin.
They are placid animals that are non-threatening to humans except in special circumstances (unlike some of their elasmobranch cousins, the sharks). Fatalities from stingray encounters are rare.
Stingray spines consist of stilletto-like, backward-pointing, serrated barbs made of a hard bone-like cartilagenous material called vasodentin. The spine has two ventral grooves lined with venom-secreting glandular cells and the entire structure is contained within an integument that rips open when a target is struck. This can result in deep lacerations or punctures with the introduction of venomous foreign material.

Typically, injury occurs when a person accidentally encounters a ray lying still on the sea bed, where they like to fed on mollusks, marine worms and crustaceans. On perceiving a threat stingrays defend themselves with their whip-like barbed tails, which may bear single or multiple spines. Their tails are highly maneuverable and can jack-knife forwards or sideways at high speed.
The common mechanisms of injury include:
- an unsuspecting wader stepping on the stingray
- a diver swimming over a stingray (or rarely even beside a stingray)
- handling of a netted or hooked stingray, or an aquarium exhibit
‘Freak’ injuries may also occur. For example, the case that opened this ‘toxicology conundrum’ is based on a rare report of an out-of-the-water contact with a leaping ray. Another unusual stingray injury resulted from the accidental ingestion of a stingray barb that became lodged in the throat of a 76 year-old woman [case report by Gan et al, 2008]. Over time the barb migrated and caused a transient ischemic attack after traversing her right common carotid artery! Another unlucky case reported in 1978 involved a deckhand who fell over with a stingray barb safely tucked away in the pocket of his trousers — somehow the fall contrived to drive the tip of the barb into the unfortunate chap’s penis…
Q3. Describe the effects and clinical importance of stingray venom?
Answer and interpretation
The clinical effects of stingray injury can be summarized as:
- direct trauma and the potential for retained foreign bodies
- local or systemic envenoming
- exposure to marine pathogens
Stingray wounds often bleed profusely initially, followed by severe local pain progressing over the next 15-90 minutes. The wound may be ragged and gaping. The direct trauma from the stinging barb is generally of much greater clinical significance than the envenoming syndrome. However, stingray venom should not be dismissed as clinically irrelevant.
Stingray venoms are poorly understood, for reasons that include the absence of “milkable” venom glands (stingrays can’t be milked!), difficulties in extracting and isolating the venom, and the physical instability of venom constituents.
Stingray venom components include:
- thermolabile toxic proteins such as phosphodiesterases and 5′ nucleotidases
(one study found that about 90% of stingray victims have total relief of pain after 30 minutes of hot water immersion of the wound site) - degradative enzymes such as hyaluronidases
- non-protein components such as serotonin and numerous as yet unidentified substances.
Stingray venom local effects include:
- severe pain at the site of injury
- tissue necrosis — myonecrosis (in some situations involving cardiac muscle) is often noted in histological specimens of wounds
Stingray venom systemic effects are associated with viscus penetration, and rarely, if ever, occur in those with peripheral stingray injuries only. Cardiotoxic effects have been demonstrated in humans and experimental animals, but stingray venom does not have anticoagulant, hemolytic, or neuromuscular-blocking properties.
Reported systemic effects include:
- nausea and vomiting, diarrhoea
- salivation
- sweating
- respiratory depression
- muscle fasciculations and cramps
- syncope and hypotension
- convulsions
- cramping abdominal pain
- arrhythmias (including bigeminy, all degrees of heart block and asystole)
- myocardial ischaemia
Q4. What types of injuries do stingrays inflict?
Answer and interpretation
Stingrays typically inflict deep lacerations and puncture wounds.
The injuries most commonly affect the limbs and may involve various structures including tendons, muscle, joints, nerves, and vessels.
Penetrating neck, chest and abdominal trauma may also occur with the potential for life-threatening damage to the structures just mentioned, as well as potential airway compromise and damage to internal organs.
Penetrating chest injuries are probably the most dramatic and feared injuries that may occur. These injuries are highly lethal. Notable cases from Australasia include:
- 1938 — An autopsy demonstrated that a New Zealand woman died from a stingray bard that transfixed both ventricles of the heart.
- 1945 — An Australian soldier was killed by a ventricular injury inflicted while swimming in St. Kilda Baths near Melbourne. His wound was 7.6 cm long but no barb was found, and no stingray was positively identified.
- 1989 — The case that inspired this “toxicology conundrum” – a 12 year old boy died (after being discharged well) 6 days after a chest wound inflicted by a stingray barb. Autopsy revealed a left pleural effusion and a necrotic right ventricular wound with a 1 cm rind of clotted pericardial blood. However, the offical cause of death was pericardial tamponade from chemical (rather than traumatic) myocardial necrosis, presumably attributable to the local cardiotoxic/ myotoxic effect of the stingray venom.
- 2006 — The tragic death of Steve Irwin; a stark reminder of relative insignificance of stingray venom compared to the severe direct trauma that can occur.
Delayed complications of stingray injury may include:
- retained foreign bodies (fragments of barbs, the spine integument, and venom-secreting glandular tissue) may migrate causing local tissue injury or result in granulomatous foreign body reactions.
- formation of pseudoaneurysms or arteriovenous fistulae
- delayed infectious complications (see Q6)
Oh yeah — and don’t put your fingers in a stingray’s mouth unless you want to see what effect their carapace-crushing teeth has on soft human flesh…
Q5. Describe your approach to managing this patient?
Answer and interpretation
Prehospital
- Remove the victim from the water
- Reassure the patient, consider oral analgesia
- Early wound irrigation with water unless this compromises hemorrhage control
- Hot water immersion — also immerse an unaffected limb to ensure water temperature is tolerable and so prevent burns
- Transport all patients to a medical facility unless the injury is trivial
- Do not remove the spine unless certain that it is only superficially embedded
- Control hemorrhage by applying local pressure to the wounds with elevation of the affected body part
- Do not apply a tourniquet or pressure immobilization bandage (PIB)
Resuscitation —
Stingray injury is rarely life-threatening but potential life threats that may require immediate intervention should be considered. They include:
- penetrating thoracic trauma – immediate or delayed cardiac tamponade, hemopneumothorax
- cervical lacerations with airway compromise
- penetrating vascular wounds with hemorrhagic shock
- delayed wound infections with gangrene, wound botulism, and septic shock
- penetrating thoracic trauma – perforated viscus
- Patients with potential life-threats should be managed in an area equipped for cardiorespiratory monitoring and resuscitation
Patients requiring opioid analgesia may be discharged when they have been asymptomatic for a period of 4 hours
Supportive care and monitoring —
Analgesia
- hot water immersion
- consider regional anesthesia if refractory to hot water immersion
(avoid local adrenaline injections as it may delay microvascular clearance and increase the risk of local necrosis) - oral and intravenous analgesia as required
Wound management
- Careful wound examination, removal of foreign material, irrigation and debridement
- Heal by secondary intention; consider use of an alginate-based dressing
- Consider antibiotic administration (see Q6)
- Tetanus prophylaxis
- The role of hyperbaric oxygen therapy in treating stingray wound-related infections is uncertain
Consider invasive monitoring if hemodynamically unstable (central venous access and cardiac output monitoring such as PiCCO or a pulmonary artery catheter)
Investigations — as required to detect/ confirm local and systemic effects of stingray injury and complications:
ECG and continuous monitoring (arrhythmia, ischemic changes, conduction blocks)
Imaging
- Chest radiograph (haemopneumothorax)
- Wound radiograph (may detect foreign bodies)
- Ultrasound (if undetected foreign body suspected, extended FAST scan for thoraco-abdominal trauma)
- Echocardiography (suspected cardiothoracic injury or cardiotoxicity)
- CT neck/ chest/ abdomen (hemodynamically stable major penetrating trauma patient)
- MRI (if undetected foreign body suspected)
Laboratory
- FBC, UEC, LFTs, troponin, CK (cardiac injury or cardiotoxicity, abdominal trauma, multi-organ dysfunction, coexistent disease)
- wound swab (consider if high risk of infection — specify seawater involvement on the request form)
- blood cultures (if septicaemia suspected)
Decontamination, Enhanced elimination, Antidotes — nil
Disposition —
Severe stingray injury or complications present:
- Patients with airway compromise or hemodynamic instability due to trauma may required immediate surgical intervention
- Early cardiothoracic/ trauma surgery referral of confirmed or suspected penetrating injuries of chest or abdomen
- Wounds that cannot be adequately explored and debrided in the ED require appropriate surgical review
- Infected stingray injuries may require consultations with an Infectious Disease specialist or Microbiologist
Non-severe stingray injury:
- Patients with minor injuries without clinical features of systemic envenoming at 2 hours do not require further medical observation
Q6. When should antibiotics be used in stingray injury? What should be used and why?
Answer and interpretation
Stingray injuries are at risk of infectious complications. Contributing factors include:
- The retention of foreign matter may act as a nidus of infection
- The wounds may be deep punctures that do not drain freely and have ragged edges
- Stingray venom may contribute to local tissue necrosis
- The injury itself may introduce marine pathogens such as Vibrio species causing necrotic wound infection.
(Other infective organisms may include Streptococcus, Staphylococcus, Aeromonas, and Clostridium spp.)
Local wound infection may be complicated by:
- Ecthyma gangrenosa
- osteomyelitis or septic arthritis
- septicemia
- rarely necrotising fasciitis and bizarre infections
- death due to tetanus has been reported after stingray injury
The most important factors in preventing infection are likely to be early wound irrigation, debridement and the removal of any foreign material.
Antibiotic cover should be considered for large or established wounds, especially if irrigation or debridement was delayed, and for penetrating wounds. Clark et al (2007) reported high rates of representation with local wound infections among stingray injured patients who were not given prophylactic antibiotics. In Australia, commonly used prophylactic antibiotics for wounds exposed to seawater include doxycycline 100mg daily or ciprofloxacin 500mg twice daily (or as dictated by wound cultures).
Q7. How might stingray injuries be prevented?
Answer and interpretation
The simple answer to avoid marine envenomings to avoid the sea (although that’s probably no guarantee of safety…)
For those brave souls that are drawn to the salty underworld, some tips to help stay safe include:
- Be aware of known stingray habitats
- Keep your eye on the sea floor – and be extremely cautious if the water is murky
- When wading probe ahead with a stick and shuffle your feet along the sea floor to avoid stepping on a stingray and to encourage nearby stingrays to move away
- Be wary of cruising along the sea bed when snorkeling or diving, particularly in known stingray habitats
- Remember that dive suits and dive boots offer little protection against a stingray barb
- Remember that the excised sting of a ray may still be dangerous (blokes – don’t carry it around in your trouser pocket!)
- Don’t attempt to handle a netted or hooked stingray
- Don’t try to pet the friendly looking bull ray in your local aquarium…
Finally, amidst all this doom and gloom, we should remember that there are people in the water alongside stingrays all the time and injuries are proportionally uncommon, and usually minor when they do occur.
References
- Diaz JH. The evaluation, management, and prevention of stingray injuries in travelers. J Travel Med. 2008;15(2) 102-109. [PMID 18346243]
- Fenner PJ, Williamson JA, Skinner RA. Fatal and non-fatal stingray envenomation. Med J Aust. 1989;151(11-12):621-625 [PMID 2593906]
- Clark RF, Girard RH, Rao D, Ly BT, Davis DP. Stingray envenomation: a retrospective review of clinical presentation and treatment in 119 cases. J Emerg Med. 2007 Jul;33(1):33-7. [PMID 17630073]
- Weiss BF, Wolfenden HD. Survivor of a stingray injury to the heart. Med J Aust. Jul 2 2001;175(1):33-34. [PMID 11476200]
- Gan DCC, Huilgol RL, Westcott MJ. Transient ischaemic attack caused by an ingested stingray barb. MJA 2008; 189 (11/12): 668-669. [PMID 19061468]

CLINICAL CASES
Toxicology Conundrum
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC

thank you for making this article very useful and keep up the good work