Stroke Infarction: Anterior Circulation
Ischaemic stroke is defined as an episode of neurological dysfunction caused by focal cerebral, spinal, or retinal infarction. However, the preferred terminology is cerebral infarction or cerebral haemorrhage, as these represent distinct pathologies requiring different management strategies.
An overarching term, acute brain attack, has been proposed. Given the connotations, “acute cerebral syndrome” might be more appropriate, but as “ACS” is already used for acute coronary syndrome, acute cerebral event (ACE) could be considered.
This document focuses on cerebral infarction within the anterior circulation.
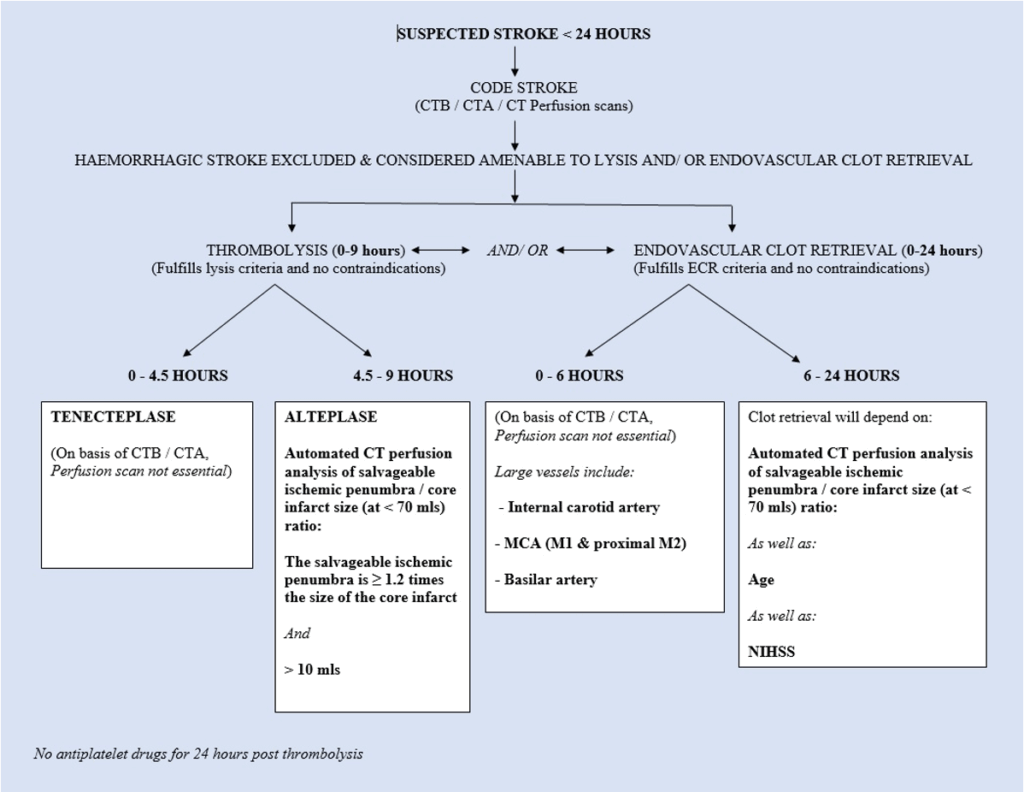
Time-critical interventions in acute ischaemic infarction include:
- IV thrombolysis within 9 hours of symptom onset.
- Endovascular clot retrieval within 6 hours, or in selected cases, up to 24 hours.
Tele-stroke consultation systems and rapid assessment and transfer protocols to neurointervention stroke centres have been developed to facilitate these treatments.
See also separate documents on:
- Stroke Infarction — Posterior Circulation
- Stroke Infarction — Posterior Circulation — Basilar Artery
- Stroke Infarction — Endovascular Clot Retrieval
- Stroke Infarction — Thrombolysis
- Stroke Infarction — Oxfordshire Classification
History
Historically, “stroke” was defined as a vascular disturbance resulting in a focal neurological deficit lasting at least 24 hours. This time frame is arbitrary and not based on pathophysiology.
The term “stroke” was first introduced into medicine in 1689 by English physician William Cole in his work A Physico-Medical Essay Concerning the Late Frequencies of Apoplexies. Prior to this, the term “apoplexy” was commonly used, dating back to Hippocrates around 400 BC.
In the 1950s, the term transient ischaemic attack (TIA) was introduced by Charles Miller Fisher (1913-2012) to describe temporary vascular-related episodes of brain dysfunction not qualifying as strokes.
The term cerebrovascular accident (CVA) is now discouraged.
Classification
Cerebral infarction can be classified according to the Oxfordshire Community Stroke Project (OCSP) classification:
- TACI (Total Anterior Circulation Infarct):
- Triad of:
- Contralateral hemiparesis and/or hemisensory loss (face, arm, leg)
- Higher cortical dysfunction (e.g., dysphasia or visuospatial neglect)
- Homonymous hemianopia
- If altered consciousness or unable to test, the second two are usually assumed.
- Triad of:
- PACI (Partial Anterior Circulation Infarct):
- Two of the TACI features
- Isolated higher cortical dysfunction
- Limited motor/sensory deficit (e.g., confined to one limb or face and hand)
- LACI (Lacunar Infarct):
- Four types:
- Pure motor (face, arm, leg) — most common
- Pure sensory (face, arm, leg)
- Sensorimotor (face, arm, leg)
- Ataxic hemiparesis
- Four types:
- POCI (Posterior Circulation Infarct):
- Brainstem signs ± isolated homonymous hemianopia:
- Ipsilateral cranial nerve with contralateral motor/sensory deficit
- Bilateral motor/sensory deficit
- Conjugate eye movement disorder
- Coma (basilar artery infarcts)
- Cerebellar signs without ipsilateral hemiparesis/sensory signs
- Isolated homonymous hemianopia
- Brainstem signs ± isolated homonymous hemianopia:
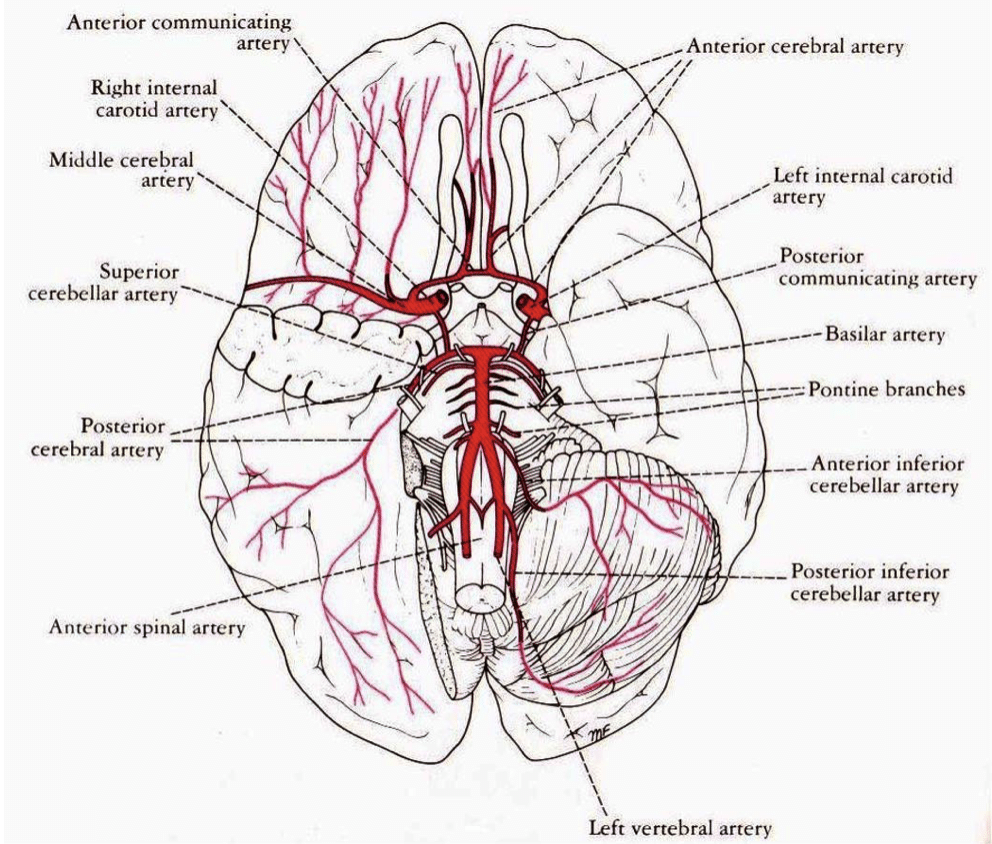
Pathophysiology
Causes of vascular occlusion include:
- Thrombosis due to atherosclerotic disease
- Embolic disease:
- Cardiac source
- Atherosclerotic disease of large arteries
- Carotid/vertebral artery dissection
- Migraine
- Inflammatory vasculitis
- Hypoperfusion/stasis:
- Especially in watershed regions between cerebral arterial territories
- Procoagulant disorders
The Ischaemic Penumbra
Following cerebral artery occlusion, a central core of tissue becomes infarcted within minutes. Surrounding this is the ischaemic penumbra—a region of partially perfused tissue that may remain viable if blood flow is restored promptly.
- Thrombolysis can salvage penumbral tissue if administered within 9 hours.
- Endovascular clot retrieval may be effective up to 24 hours in selected cases.
Early identification and reperfusion of the penumbra are critical to improving outcomes.
Clinical Assessment
History:
- Time of symptom onset: Crucial for determining eligibility for thrombolysis (within 9 hours) or clot retrieval (up to 24 hours in selected cases).
- Comorbidities and functional status: Assess using the Modified Rankin Scale.
- Past medical history: Focus on cardiac disease, arrhythmias (especially AF), and contraindications to thrombolysis.
- Medications: Note use of aspirin, warfarin, or DOACs.
Examination:
- ABC assessment, including gag reflex.
- Bedside glucose level.
- Neurological assessment:
- Glasgow Coma Scale (GCS)
- OCSP classification to localize vascular territory
- NIH Stroke Scale (NIHSS) for severity assessment
Differential diagnoses:
- Space-occupying lesions
- Extra-axial traumatic haemorrhage (subdural or extradural)
- Venous sinus thrombosis
- Metabolic disorders (e.g., hyponatraemia, hypoglycaemia, Wernicke’s encephalopathy)
- Todd’s paresis
- Demyelinating disease
- Psychogenic causes
Investigations
Blood tests:
- FBC
- U&Es/glucose
- Clotting profile:
- Elevated INR contraindicates thrombolysis
- Consider procoagulant screen in younger patients
- Fasting lipids (not an ED priority)
- CRP/ESR if vasculitis is suspected
ECG:
- Monitor for AF or ischaemic changes
- Continuous monitoring recommended for at least 24 hours
CXR:
- Assess for cardiomegaly or aspiration
- Should not delay other investigations
CT Brain Imaging:
- Non-contrast CT: Mandatory to differentiate between ischaemic and haemorrhagic stroke
- CT Angiography (CTA): Evaluates vascular anatomy and identifies occlusions
- CT Perfusion: Assesses cerebral blood flow and identifies salvageable penumbra
MRI/MRA:
- More sensitive than CT for early infarction
- Sequences include:
- Diffusion-weighted imaging (DWI)
- FLAIR
- T2-weighted imaging
- MRA/MRV
- Perfusion imaging (with gadolinium)
Echocardiography:
- Consider if embolic source is suspected
- Transoesophageal echocardiography (TOE) is more sensitive for valvular and atrial pathology
Management
1. Immediate Care:
- Airway, Breathing, Circulation (ABC)
- Oxygen therapy if saturation <95%
- IV access and normal saline (avoid glucose-containing solutions)
- Correct hypoglycaemia urgently
- Nil by mouth until assessed by a speech pathologist
2. Blood Pressure Management:
- Monitor closely in the first 48 hours
- Do not treat unless:
- BP >220/120 mmHg: reduce cautiously by no more than 20% over 24 hours
- Eligible for thrombolysis: reduce to <185/110 mmHg before treatment
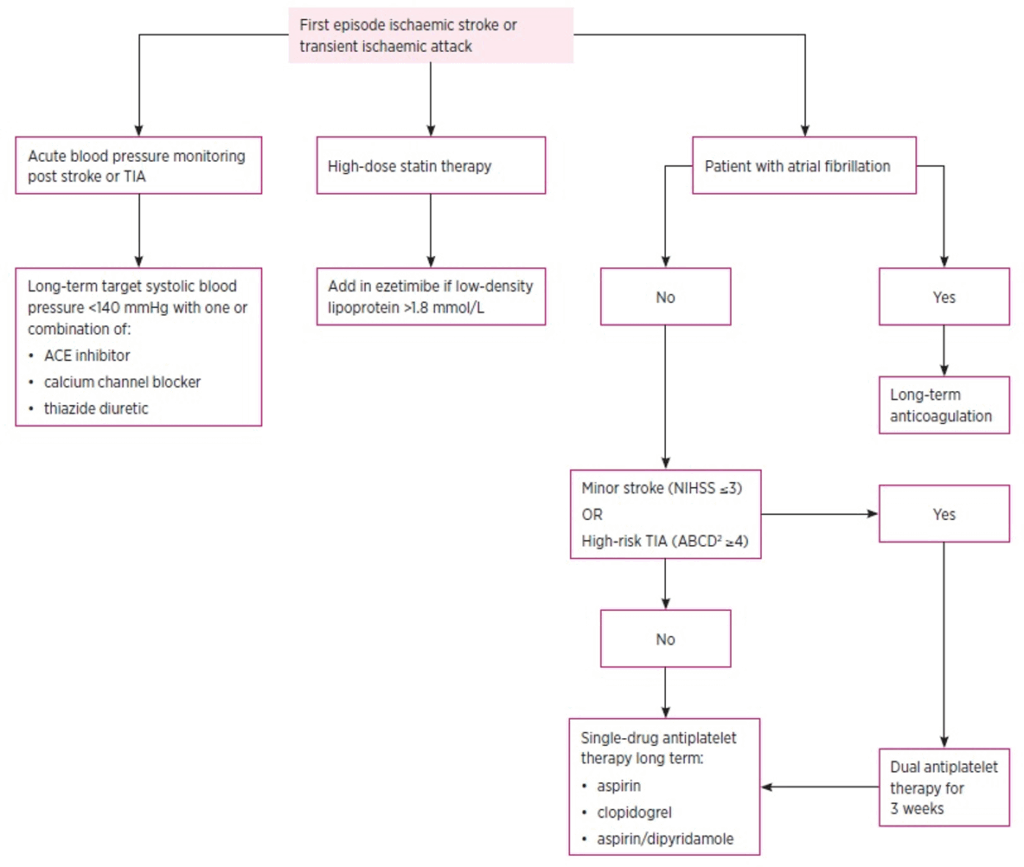
3. Antithrombotic Therapy:
- Post-thrombolysis: Delay antiplatelet therapy for at least 24 hours and after repeat imaging
- No thrombolysis:
- Initiate antiplatelet therapy once haemorrhage is excluded
- Minor stroke/TIA (NIHSS ≤3): Dual antiplatelet therapy for 3 weeks, then monotherapy
- Major stroke (NIHSS >3): Monotherapy preferred
Antiplatelet options:
- Aspirin: 300 mg loading dose, then 75 mg daily
- Clopidogrel: 300 mg loading dose, then 75 mg daily
- Aspirin + Dipyridamole: Consider for long-term prevention
4. Thrombolysis:
- Tenecteplase: Preferred within 4.5 hours
- Alteplase (tPA): Used within 9 hours
- Administer only in centres with appropriate expertise
5. Endovascular Clot Retrieval:
- Indicated for proximal large vessel occlusions within 6 hours
- Selected patients may benefit up to 24 hours based on imaging
6. Anticoagulation:
- Heparin: Not routinely recommended post-stroke without cardioembolism
- Warfarin:
- Minor stroke: Continue if INR therapeutic
- Major stroke: Withhold for 5–7 days due to haemorrhagic risk
7. Neurosurgery:
- Decompressive hemicraniectomy for malignant MCA infarction in patients ≤60 years
- Posterior fossa decompression for large cerebellar infarcts threatening brainstem compression
8. Cerebral Oedema:
- Mannitol and hyperventilation may be used in deterioration
- Corticosteroids are not recommended
9. Swallow Assessment:
- Speech pathologist assessment within 24 hours
10. Indwelling Catheter (IDC):
- Consider for patients with reduced consciousness
- Should not delay urgent investigations
11. Pyrexia:
- Treat with paracetamol and/or physical cooling
- Investigate and treat underlying infections
12. Statins:
- High-dose statins (e.g., atorvastatin 80 mg, rosuvastatin 40 mg) recommended regardless of cholesterol levels
- Aim for LDL <1.8 mmol/L; add ezetimibe if target
Appendix 1
Appendix 2
Appendix 3
Case Study 1
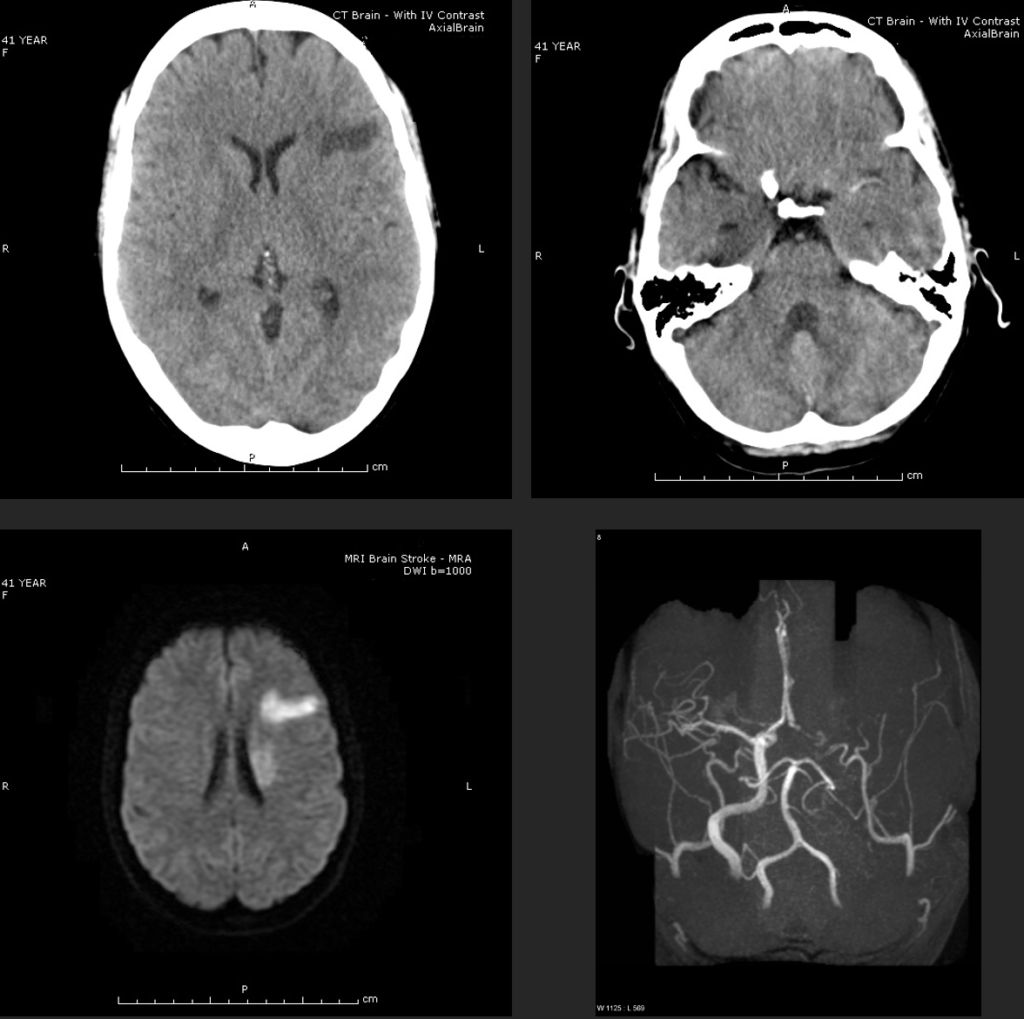
CT scan with contrast of 41 year old female who presented with acute onset, 30 minutes previously, of aphasia and right sided hemiparesis. The left scan shows a hypodense region within the left frontal lobe, without negative mass effect and consistent with recent infarction. The lesion does not enhance diminishing the likelihood of a vascular lesion or tumour. The right scan shows a hyperdense left middle cerebral artery consistent with thrombo-embolic disease.
MRI / MRA scans done 30 minutes after CT scan above. These scans clearly demonstrate the superiority of MRI scanning over CT scanning for acute stroke.
The left scan more clearly shows the original area of infarction within the frontal lobe, but also demonstrates a second lesion, not seen on the CT scan, within the posterior aspect of the corona radiata of less recent duration.
The right MRA scan clearly demonstrates the vascular occlusion pathology. The vertebral and basilar artery system is clearly seen as is the internal carotid system on the right, (the left external carotid system is seen intact). The left internal carotid and left middle cerebral arteries however are completely absent suggesting total occlusion of these vessels.
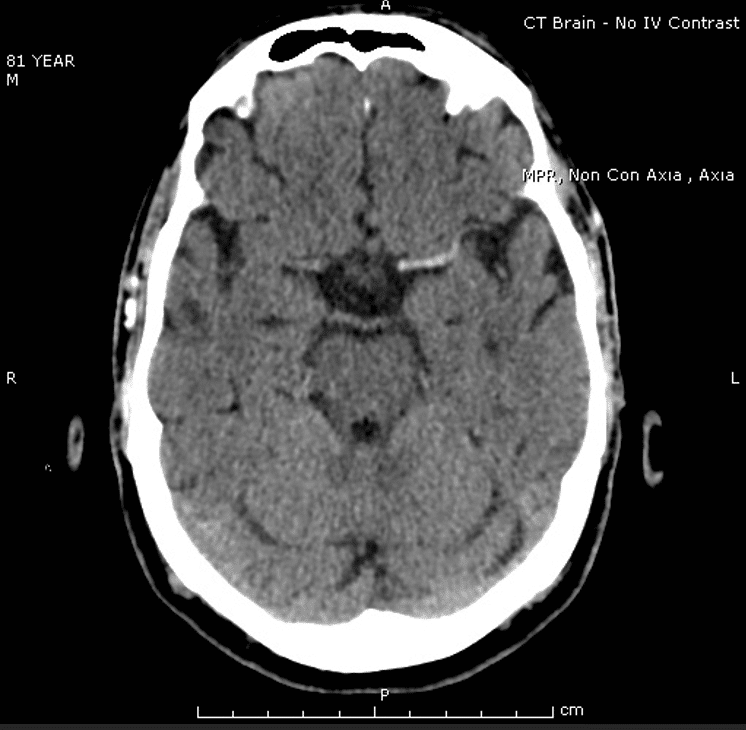
Case Study 2
Appendix 4
References
Publications
- Cole W. A physico-medical essay concerning the late frequency of apoplexies. 1693
- Fisher M. Occlusion of the internal carotid artery. AMA Arch Neurol Psychiatry. 1951 Mar;65(3):346-77
- Tremonti C, Thieben M. Drugs in secondary stroke prevention. Aust Prescr. 2021 Jun;44(3):85-90.
- Clinical Guidelines for Acute Stroke Management – National Stroke Foundation
- Brazis PW, Masdeu JC, Biller J. Localization in Clinical Neurology. 8e 2021
- Fuller G. Neurological Examination Made Easy. 6e 2019
- O’Brien M. Aids to the Examination of the Peripheral Nervous System. 6e 2023
FOAMed
- Coni R. Neuro 101: Cerebral Hemispheres. LITFL
- Nickson C. Stroke Thrombolysis. LITFL
Fellowship Notes
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner
Educator, magister, munus exemplar, dicata in agro subitis medicina et discrimine cura | FFS |


