Stroke Infarction: Posterior Circulation
This document relates to posterior circulation infarction, which presents unique diagnostic challenges. Signs are often subtle and non-specific, commonly limited to nausea, vomiting, and vertigo.
Ischaemic stroke is defined as an episode of neurological dysfunction caused by a focal cerebral, spinal, or retinal infarction.
The preferred terminology is cerebral infarction or cerebral haemorrhage, as these represent distinct pathophysiological entities with different management strategies.
The most catastrophic variant is basilar artery infarction.
Time-critical interventions:
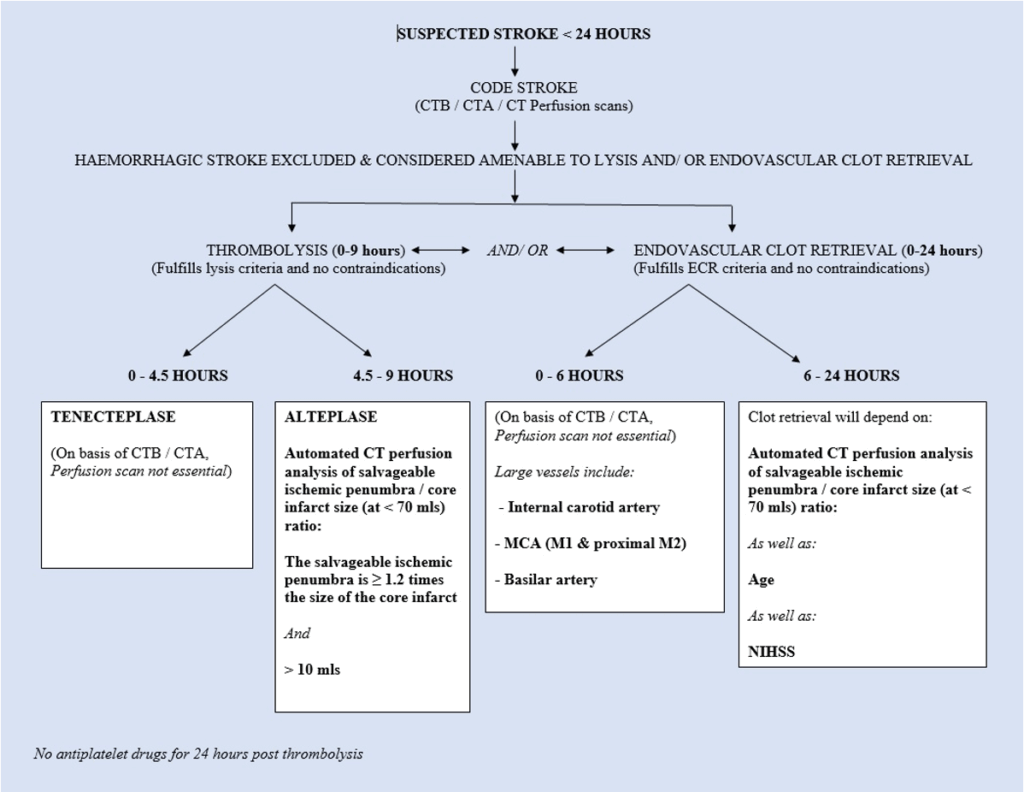
- IV thrombolysis: within 9 hours of symptom onset
- Endovascular clot retrieval: within 6 hours, or in selected cases up to 24 hours
Tele-stroke systems and streamlined transfer protocols to neurointervention centres are key to timely management.
See also:
- Stroke infarction – posterior circulation – basilar artery
- Stroke infarction – endovascular clot retrieval
- Stroke infarction – thrombolysis
- Stroke infarction – Oxfordshire classification
History
Historically, “stroke” was defined as a vascular disturbance resulting in a focal neurological deficit lasting at least 24 hours. This time frame is arbitrary and not based on pathophysiology.
The term “stroke” was first introduced into medicine in 1689 by English physician William Cole in his work A Physico-Medical Essay Concerning the Late Frequencies of Apoplexies. Prior to this, the term “apoplexy” was commonly used, dating back to Hippocrates around 400 BC.
In the 1950s, the term transient ischaemic attack (TIA) was introduced by Charles Miller Fisher (1913-2012) to describe temporary vascular-related episodes of brain dysfunction not qualifying as strokes.
The term cerebrovascular accident (CVA) is now discouraged.
Classification
According to the Oxfordshire Community Stroke Project (OCSP):
- TACI: Total anterior circulation infarct
- PACI: Partial anterior circulation infarct
- LACI: Lacunar infarct
- POCI: Posterior circulation infarct
POCI includes:
- Brainstem signs ± homonymous hemianopia
- Ipsilateral cranial nerve with contralateral motor/sensory signs
- Bilateral motor/sensory signs
- Conjugate gaze palsy
- Coma (basilar artery involvement)
- Cerebellar signs (without ipsilateral hemiparesis)
- Isolated homonymous hemianopia
Importantly, not all POCI strokes present with clear localising signs. Up to 10% of cerebellar infarctions present solely with nausea, vomiting, and vertigo, without focal neurological findings.
Pathophysiology
Causes of posterior circulation infarction:
- Thrombosis (atherosclerosis)
- Embolism:
- Cardiac origin
- Atheroembolism from large vessels
- Carotid/vertebral artery dissection
- Migraine
- Inflammatory vasculitis
- Hypoperfusion, particularly in watershed areas
- Procoagulant disorders
The ischaemic penumbra
Occlusion leads to rapid infarction of a central core. Surrounding this is the ischaemic penumbra — partially perfused, potentially salvageable tissue.
- Viability can be preserved if perfusion is restored within:
- 4.5 hours with thrombolysis
- 24 hours with clot retrieval
Clinical features
Posterior circulation stroke often presents atypically.
Non-specific features:
- The three Vs:
- Vomiting
- Vertigo
- Visual disturbance
- Altered consciousness or coma
Specific features (less common):
- Cerebellar signs
- Cranial nerve or long tract signs
Differentiating central vs peripheral vertigo is critical. See the Vertigo document for detailed guidance.
Investigations
Blood tests:
- FBC, U&Es, glucose
- Coagulation profile (important for thrombolysis decisions)
- Fasting lipids
- CRP/ESR if vasculitis suspected
ECG:
- Look for AF or atrial flutter
Imaging:
- CT scan: rule out haemorrhage
- CT angiogram: assess for large vessel occlusion
- CT perfusion: identify salvageable penumbra (note: less sensitive for small posterior lesions)
MRI/MRA:
- Best for cerebellar/brainstem infarction and vertigo
- Superior for detecting small infarcts and vascular pathology
- Required if CT-based imaging is inconclusive
Echocardiography:
- Consider in stroke with unclear aetiology
- TOE preferred for valvular or aortic arch pathology
Management
1. ABC and supportive care
- Oxygen only if SpO₂ < 95%
- IV access and normal saline (avoid glucose)
2. Glucose
- Treat hypoglycaemia
- Avoid tight glucose control; use conservative insulin as needed
3. Nil orally
- Until assessed by a speech pathologist
4. Blood pressure management
- Monitor closely
- Treat if >220/120 mmHg (unless thrombolysis planned: target <185/110 mmHg)
- Preferred IV agents: nicardipine, labetalol, GTN, hydralazine
5. Antiplatelet therapy
- Withhold if thrombolysis is planned
- Start after haemorrhage excluded via CT
- Options:
- Aspirin 300 mg stat, then 100–150 mg daily
- Clopidogrel 75 mg (if aspirin contraindicated)
- Asasantin for long-term use (aspirin + dipyridamole)
6. Thrombolysis
- Standard care in eligible patients within 9 hours
- Use tPA (alteplase)
- Requires experienced team and protocols
7. Endovascular clot retrieval
- For large vessel occlusion within 6–24 hours
- ICA, MCA (M1/M2), basilar artery
- Selection based on perfusion mismatch
8. Anticoagulation
- Not recommended unless cardioembolic cause
- For patients on warfarin:
- Continue if minor stroke
- Withhold 5–7 days if large infarct
9. Neurosurgery
- Consider hemicraniectomy for large cerebellar infarct with brainstem compression
- Decision based on clinical and functional status
10. Cerebral oedema
- Mannitol or hyperventilation in raised ICP
- Steroids not recommended
11. Speech pathologist assessment
- Within 24 hours for oral intake suitability
12. IDC
- If needed, without delaying other priorities
13. Pyrexia
- Treat fever and any infection promptly
- Use paracetamol and cooling as required
disposition
- Transfer to thrombolysis-capable ED
- Activate CODE STROKE protocols
- Consider endovascular clot retrieval for strokes within 6–24 hours
- Admit to a stroke unit — shown to reduce morbidity and mortality
Appendix 1
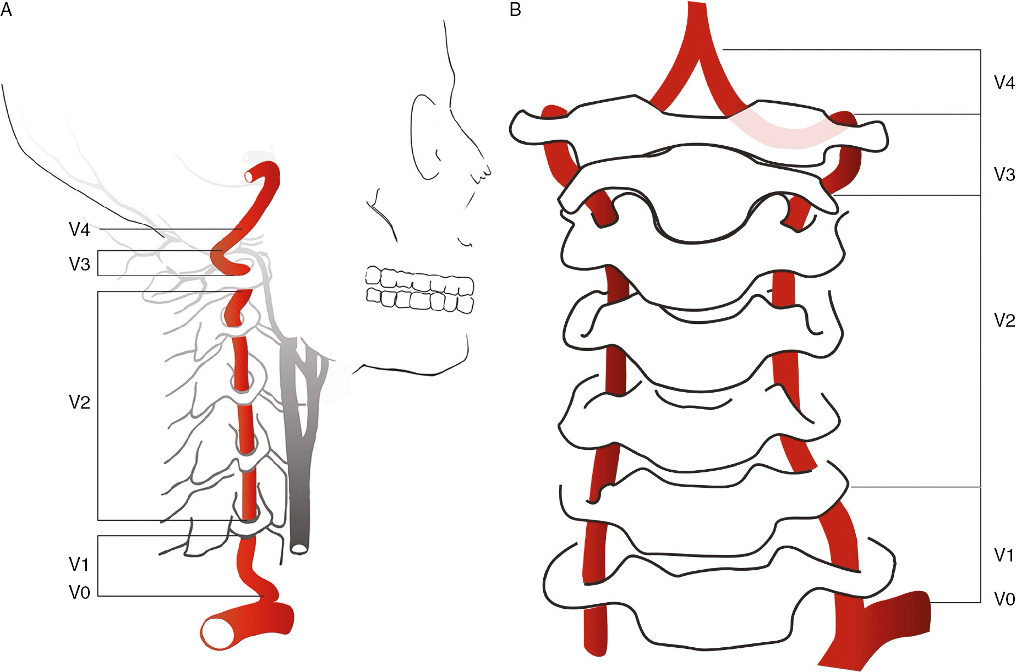
Vertebral artery anatomy:
The vertebral artery is typically divided into 4 segments:
- V1 (Preforaminal): From the subclavian origin to the transverse foramen of C6
- V2 (Foraminal): From the transverse foramen of C6 to the transverse foramen of C2
- V3 (Atlantic, extradural or extraspinal): From C2 to the dura
- V4 (intradural or intracranial): Within the dura to the confluence that forms the basilar artery
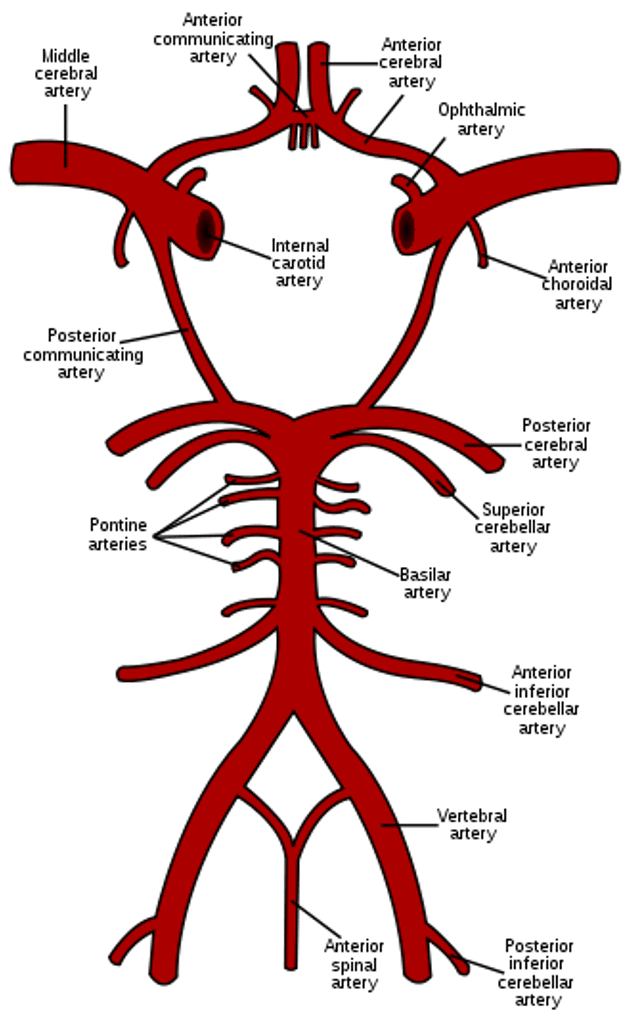
The posterior fossa arterial circulation
Appendix 2
Case Study 1
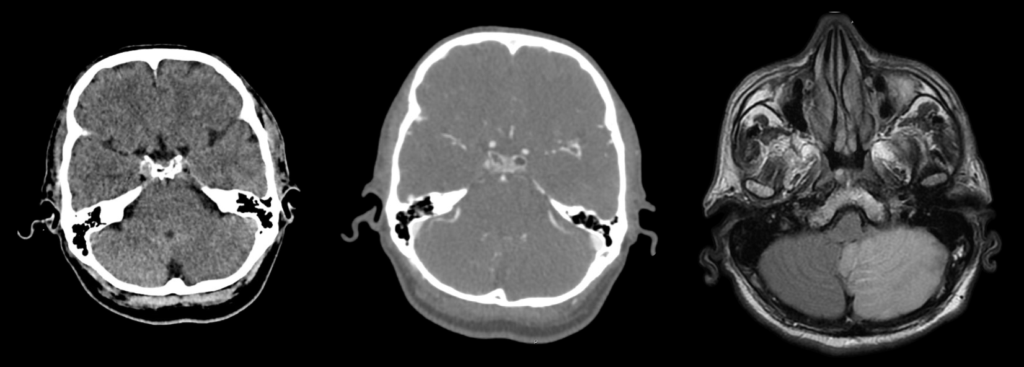
A 62 year old man presented with an indistinct history of unrelenting nausea and mild “dizziness”. Clinical examination was inconclusive, including for “HINTS”, apart from a subtle ataxia. CT scan (above left) and CT angiogram (above right) showed no obvious abnormality.
A CODE STROKE was not activated which meant that a CT perfusion scan was not performed.
Several days later, an MRI scan was performed, as the patients symptoms had not resolved. This showed a surprisingly spectacular ischaemic lesion of the left cerebellum, considering the subtlety of his symptoms and signs.
This case demonstrates the challenges of clinical assessment in posterior circulation stroke, the importance of the CT perfusion scan in a CODE STROKE protocol, and the superiority of MRI as an imaging modality in stroke. (Case photographs, courtesy Dr. Peter Cheng, May 2019).
Appendix 3
Appendix 4
References
Publications
- Cole W. A physico-medical essay concerning the late frequency of apoplexies. 1693
- Fisher M. Occlusion of the internal carotid artery. AMA Arch Neurol Psychiatry. 1951 Mar;65(3):346-77
- Nogueira RG et al; DAWN Trial Investigators. Thrombectomy 6 to 24 Hours after Stroke with a Mismatch between Deficit and Infarct. N Engl J Med. 2018 Jan 4;378(1):11-21.
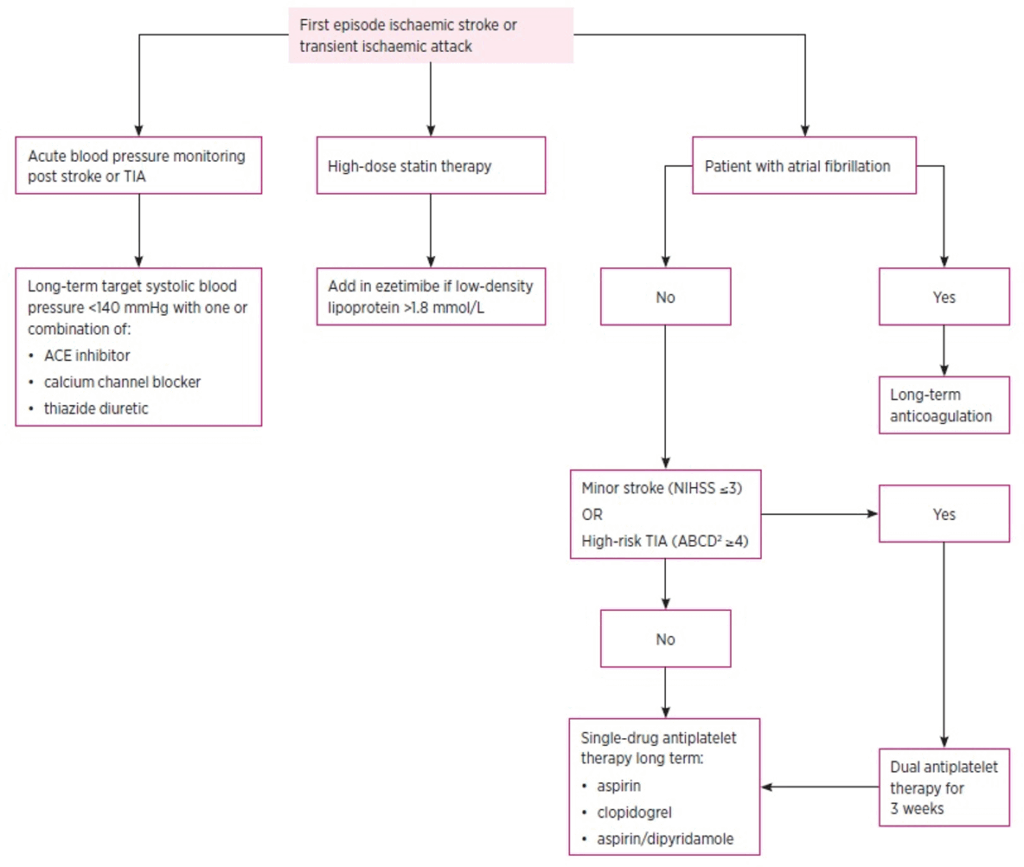
- Tremonti C, Thieben M. Drugs in secondary stroke prevention. Aust Prescr. 2021 Jun;44(3):85-90.
- Clinical Guidelines for Acute Stroke Management – National Stroke Foundation
- Brazis PW, Masdeu JC, Biller J. Localization in Clinical Neurology. 8e 2021
- Fuller G. Neurological Examination Made Easy. 6e 2019
- O’Brien M. Aids to the Examination of the Peripheral Nervous System. 6e 2023
FOAMed
- Coni R. Neuro 101: Cerebral Hemispheres. LITFL
- Nickson C. Stroke Thrombolysis. LITFL
Fellowship Notes
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner
Educator, magister, munus exemplar, dicata in agro subitis medicina et discrimine cura | FFS |


