Super Docs 2.0
As the plane descended over the Southern Alps and through the Canterbury Plains, making it’s way east to the Pacific Ocean like the Waimakariri, I couldn’t help but feel excited to be returning home. Home being the shaky isles of New Zealand and my six-week medical elective being in the particularly shaky city of Christchurch.
Although Perth has been my new home since 2007, I spent the four years prior to that gaining my undergraduate degree in Christchurch; four years which I look back on with great fondness. Unfortunately much has changed since then in this once beautiful city. The devastating earthquake of February 2011 which levelled the CBD and claimed 185 lives has forever changed the city’s landscape. Much has changed in my life too. I began university in Christchurch as a fresh-faced engineering student, before an unlucky rugby tackle ruptured my spleen and almost had me confirming whether they really do play rugby in heaven. Faced with my own mortality, I had a change of perspective on what I wanted to do with my life, which ultimately led me away from Christchurch and engineering and into Perth and medicine.
As I was returning to this somewhat familiar city, I was also returning to a somewhat familiar elective environment; the headquarters of seven-times Super Rugby Champions, the Crusaders. Due to my passion for the game and prior sports science qualifications, I was afforded the chance to undertake a ‘strength and conditioning’ internship with them the prior summer. It was a dream opportunity I couldn’t let pass by and during that time I got to work with the medical team, including their team physician and 2011 Rugby World Cup winning All Blacks physician, Dr Deb Robinson.
Based in the Crusaders’ newly built, world-class training facility in St Albans, my elective kicked off concurrently with the second phase of preseason in early January 2016. First business on Monday morning was a 7am medical meeting with a number of management. The head physiotherapist presented the players and they would be discussed by the medical team to varying degrees depending upon their injury status and/or stage of rehabilitation. Some players were of particular interest, the ‘long-term-injury group’, having undergone reconstructive surgery for shoulders, chests, thumbs and knees at the end of 2015. This group were rehabilitating intensely to return to play as soon as possible, as the start of the 2016 Super Rugby season loomed large.
Following the meeting, the players would begin to trickle through the medical room for medical checks and strapping. The physiotherapists were inevitably kept busy taping the team together. For instance, any player that has ever had a significant ankle injury will have that ankle strapped for every training and match for the rest of their career. Then that’s not to mention all of the shoulders, knees, elbows, wrists, backs and digits that require attention. At one point, one player had a person working simultaneously on all four of his limbs. Dr Robinson and I would also be kept busy with the general GP-presentations and plentiful array of soft-tissue complaints. She would examine all new injuries and reassess any rehabilitating athletes for ongoing management. PCLs, MCLs, achilles tendons and calf strains were ‘run-of the-mill’ presentations, but some of the more unusual complaints were a series of necrotic skin ulcers due to suspected whitetail spider bites.
By 9am sharp, everyone is in the ‘strategy room’ for the team meeting. Prior learnings are discussed as the tone and plan for the day are set. Sometimes the group would disband into their ‘mini teams’ to clarify a particular tactical situation before presenting back to the larger group. This form of learning helped to engage the players, gave them the chance to take ownership of the game plan and gave leaders the opportunity to develop. Following the meeting, the physiotherapists led a series of mobility and priming exercises in the state-of-the-art gymnasium to prepare the players to train on the field.
Morning preseason trainings could be a torrid affair for the players. Lasting up to 2 hours, the men were put through a series of physically and mentally challenging drills that were run with military precision. Drills were generally based on skills, units, maps or my favourite, conditioning. The conditioning blocks were fiercely competitive and could involve anything from brutally simple shuttle runs, modified games of ‘touch’ rugby to wrestling interspersed with more running. Either way, there was lots of running and many pain-riddled faces.

Simultaneously, the ‘long-term injury group’ were rehabilitating with a physiotherapist and trainer. Anybody who has had to rehabilitate from an injury will empathise with how much of a monotonous grind the process can be. However, it was impressive the variety of programming the team had put together to make the rehabilitation process effective and efficient, yet at the same time being engaging and stimulating for the athletes. A variety of cross-training disciplines, game-specific skills and competitive drills brought out the best in the players.

With rugby being professional for over 20 years now, technology plays a significant role in the game. During training, coaching staff have access to a growing inventory of tools including headset communication, video analysis and real-time GPS monitoring. With apps already in use that monitor player wellness and the potential for non-invasive blood testing on the horizon, today’s professional coach is inundated with more player performance markers than ever before. The sheer volume could have them all at sea, which is why specialist analysts are now employed to make sense of it all. Despite their expertise, the challenge for the future still remains to find tangible meaning in this ocean of data.
Following training, the players would recover and rest before the afternoon session. Recovery was as much a part of ‘training’ as the actual training. Players were required to spend quality time stretching, rehydrating, refuelling, having ice baths and applying compression garments if required. Some players would often be seen in the medical room utilising the ‘cold-therapy compression systems’ or the ‘graduated compression boots’ to aid their recovery. Even at a few thousand dollars each, some players have bought their own which they use in the comfort of their home or overnight in bed.
During these morning sessions I tried to make myself useful in whatever capacity I could. Whether that meant preparing strapping tape for the physios, running waters for the trainers, or being an extra body in a drill, you tried to add value where you could. However, I was obviously wanting to learn and contribute as much as possible in a medical sense. Learning was fairly straight forward; the medical team have a wealth of knowledge, with decades of experience, and were only too happy to share it with you if you were keen and eager. Having access to medical databases and the skills to search them meant I could readily contribute by way of researching the current literature. At times it was to educate a player on alternative treatment they heard an athlete was receiving elsewhere, to finding the latest cases on return to play times for specific injuries. Furthermore, I was readily able to help with the team’s baseline concussion testing. We baseline tested every player using the World Rugby endorsed Sideline Concussion Assessment Tool (SCAT 3), then also tested a number of players with an online, card-based, reaction-time tool developed by CogSport. These tools can be used again throughout the season if the player is suspected to have suffered a concussion and help guide management via the ‘graduated return to play protocol’. Moreover, when Dr Robinson could not be present, I could be her eyes and ears on the field, ready to assist with examining or managing any minor medical presentations with her recommendations.
In the afternoon, the players would reconvene to split into forwards and backs to have a smaller field-based training (meaning the backs would play games while the forwards threw each other around) followed by a weights session. During this time, I would usually head with Dr Robinson to see patients with her at ‘Sportsmed Canterbury’. ‘SportsMed’ is a large multi-disciplinary practise on the edge of the Christchurch CBD comprising physiotherapists, podiatrists, chiropractors, massage therapists, nutritionists and of course, sports doctors. There were nine doctors in total, four of whom were accredited sports physicians and the rest at various stages of training and experience. Between them there was the current Crusaders doctor, Deb, but also prior Crusaders doctors, the current 2015 World Champion All Blacks doctor, the previous 2011 World Champion All Blacks doctor, the Black Caps T20 cricket doctor, the Canterbury Tactix netball doctor, Canterbury ITM Cup doctor (current domestic rugby champions), the Baby Blacks NZ U20 rugby doctor, a New Zealand triathlon legend and a netball hall of fame inductee to round it out. Fair to say, there was a lot of sports medicine knowledge walking those halls.
Sports Medicine is a relatively new specialty through the Australasian College of Sports Physicians. The sports physician’s role is developing, but has been described as the “prevention, diagnosis, treatment and rehabilitation of injuries or medical conditions, that occur during or after physical exercise.” It would be an article unto itself detailing everything I learnt in clinic, therefore, in short, I saw a multitude of sports and musculoskeletal presentations from a diverse section of society with a number of sports doctors. I observed their history-taking, examination techniques, imaging interpretation, management processes and consultation styles. I observed many cortisone injections and I performed my own for the first time. I observed extracorporeal shockwave therapy. I spent time with podiatrists and learnt how they make orthotics. I attended registrar training, radiology tutorials, sports orthopaedic journal club and any other opportunity I was afforded. However, what I didn’t see in six full weeks, was a single ‘sick’ patient. Not one. This can be quite a shift in thinking for some doctors, especially student doctors, that the vast majority of your patients can be perfectly well. To be frank, a lot of them are even better than that, they’re young and active, with a normal BMI, no regular medications and are motivated to get better.
That in itself is a positive and when I think of other positives from the six week experience, I cringe to admit that I genuinely enjoyed all of it. The overarching highlight though would have been being part of two such fantastic teams at the Crusaders and SportsMed Canterbury. I have rarely come across environments as driven yet welcoming, as high-achieving yet humble. Being around such motivated people made for an inspiring and enjoyable workplace. It’s also unlikely to be a surprise that I love sport, being active and outdoors, and so too do these people. They make it a priority, which also makes for a vibrant, fun and healthy culture.
Among a number of other highlights, I was lucky enough to be part of a promotional visit to the Crusaders’ regional areas to engage with the community and fans. We visited the Northern Canterbury rural communities of Amberley, Hanmer Springs, Culverden and Glenmark, meeting in places as diverse as a petrol station, a bank and the trusty local rugby club. It was an action-packed road trip where we were greeted by throngs of excited kids and welcoming parents. Some stops were a simple signing session, others involved pumping petrol for the punters, cooking a BBQ lunch and running skills sessions for the kids. Despite my initial feelings of being an imposter in this public setting, I found this a really enjoyable and fulfilling day. Engaging with the kids, and even the stereotypically reserved kiwi male farmer, reminded me of when I was a kid dreaming of being an All Black and how much fun rugby is and it’s place in the New Zealand psyche.
Another highlight was undoubtedly travelling to my hometown of Invercargill for the preseason game against the reigning Super Rugby Champions, the Highlanders. Although I have been a part of Super Rugby match day proceedings in Perth before, I had never been part of an ‘away’ game, nor had the opportunity to walk the touchline as a game day medic. Being a part of the prematch rituals was a special feeling; the jersey presentation, the meal, the team talk, the bus to the game. To make it even more special was that the game was played in a farmer’s paddock, set amongst idyllic rolling green hills, as part of the annual Agricultural Field Days 60km north of Invercargill. It was the hottest ticket in town as 7,000 locals and farmers rapidly sold the event out. Despite the heavens opening up on kick-off, spirits were barely dampened as both teams put on a decent display of running rugby in slippery conditions. Despite the wet conditions, the ground was exceedingly hard and was the suspected culprit for the only significant injury during the game, a PCL strain. Although the player doesn’t recall the mechanism of injury, hard grounds are notorious for PCL injuries as the tackled player lands on their knees on the unforgiving surface, similar in mechanism to a passenger’s knees hitting the dashboard in a motor vehicle accident. A fantastic and uniquely kiwi event played out for a 31-all draw.
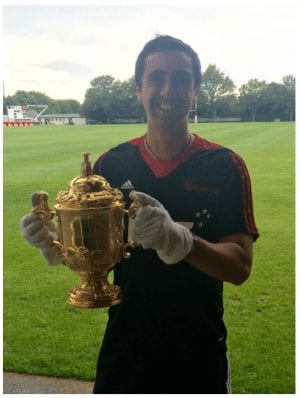
Finally, meeting one of New Zealand’s most prized possessions, “Wiremu”, was also quite special. Wiremu is Maori for William and is the affectionate nickname New Zealand gives to the William Webb Ellis Cup. The trophy is held by the victors of the quadrennial Rugby World Cup tournament, which New Zealand has prevailed in at the last two editions. Tradition goes that you can only touch Wiremu if you have been part of a team that won him, hence the white gloves.
Being a sports physician though can be a different role entirely to being a team physician. In some ways, it has similarities to my prior work in the oil & gas industry. I worked on oil platforms in the Indian Ocean off the west coast of Australia and in these tightly packed environments, you must be a team player that gets on with people. It’s similar in the professional sports team environment, you can’t be on tour for weeks at a time with a personality that doesn’t fit in with the culture. As well as fitting the culture, it’s needless to say that the doctor must be a great sports medicine technician. However, there can be times where the doctor can ‘add value’ outside of their routine scope of work. Dr Peter Brukner has written about this and recalls organising quiz nights, tipping competitions and guest speakers for the many teams he has been involved with over 30 years as a team physician . Everyday I saw Deb add value by being the consummate professional and driving high team-standards. Whether it’s just for common-sense things or a core team value, she always behaves in a manner that reflects a high-calibre outfit and individual, which has flow-on effects to those around her. She is also a very good teacher. Calm, confident and able to communicate with people from diverse backgrounds, she is a master at finding simplicity in complexity. Deb also has a unique ability to understand group dynamics, seeing the broader picture and what is best for the team and the individual. This can be a particularly powerful asset to have when the team doctor may hold the swaying vote within the management group on important issues.
When it comes to important issues, there are none more important than one’s own fragility and Christchurch has faced this in the wake of the 2011 earthquake. An excerpt from the autobiography “My Story” of former Crusader and All Black legend, Dan Carter, portrays in the aftermath of the quake the strong relationship between the Crusaders and the people of Christchurch.
We were keenly aware of what the Crusaders(sic) meant to the city at all times, especially at that moment. We used that week as Crusaders to go out into the community and help with the clean-up. It was the right thing to do, and it felt good, to be able to give back to the city which had given us so much, during its hour of need.
New Zealand ‘hero worships’ their rugby players and with Christchurch having been home to two of the greatest rugby players ever in Richie McCaw and Dan Carter, and the Crusaders being the most successful franchise in Super Rugby history, it has been a factory for ‘rugby heroes’ for over a decade. Furthermore, Cantabrians are notoriously one-eyed, parochial supporters, and even before the quake, the Crusaders meant far more to this city than ‘just a sports team’. Which follows that the Crusaders doctor’s job, is more than ‘just a job’.
Since Day 1 of medical school I had always fancied myself moving into sports medicine, but I can still clearly remember the ‘eureka moment’ when I thought being a sports physician might really be the job for me. During the previous summer at the Crusaders, we were on a training excursion to Taylor’s Mistake beach. The players had set off on a gruelling trail run while I waited on the soft sand for their return. As I tapped away on my laptop, I drifted off into an awareness of the sun on my face, the waves crashing before me, this beautiful beach almost to myself and that I was working in a dream environment. It was a serene moment where I felt pretty damn fortunate. I then turned to my left, saw Dr Robinson and realised “Deb does this for a living!”. Superficial or not, but that was when I really thought sports physician could be for me. As more time went on, that was far from an isolated experience of feeling ‘damn fortunate’ to be doing some of these extra things. Like playing lunchtime touch rugby with the other staff, who happen to be ex-All Blacks. Or tussling with a 120kg prop in boxing, or running a few drills with some of the best backs in the world. I was outdoors and active, learning and ‘working’. They’re perks of a job that could never be described as ‘just a job’.
As I reflect, I feel I’ve almost come full-circle. From the kiwi kid who dreamed of being an All Black, to the seriously injured university player with a new perspective on life. To now, almost a doctor who still dreams of being an All Black, albeit in a different ‘position’. As my journey continues, I hope to keep enjoying it and to one day complete that circle.
Related posts
Māori doctor passionate about sport & exercise medicine. #FOAMed evangelist | @taneeunson | LinkedIn