That optic disc doesn’t look right…
aka Ophthalmology Befuddler 009a [Patient 1] [Patient 2]
A 31 year-old woman presents with loss of vision in her right eye that has progressed over the last 2 days. She has mild discomfort when her eye moves. On review of systems he mentions that she has had episodes of numbness in her right lower limb and left hand.
Examination confirms that she has reduced visual acuity. A right-sided Marcus-Gunn pupil is also noted.
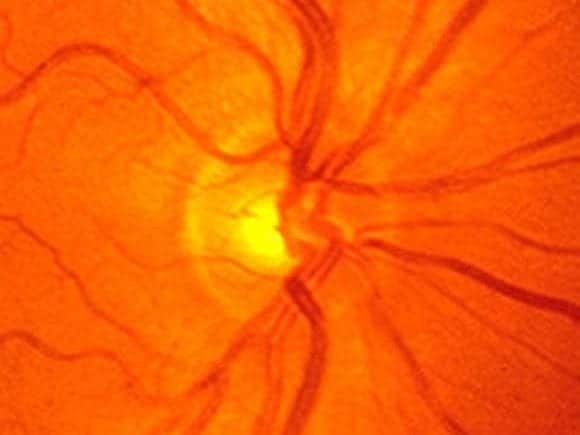
This appearance is seen on funduscopy of the right eye:

The left eye has a normal optic disc:
Following consultation with an ophthalmologist and a neurologist an MRI of her brain and spine is performed. A total of 4 discretes areas of demyelination are seen.
Questions
Q1. What is the likely diagnosis?
Answer and interpretation
Optic neuritis — papillitis is seen on fundoscopy.
The history and MRI findings are suggestive of an underlying diagnosis of new onset multiple sclerosis.
Q2. What features should be sought when taking the history?
Answer and interpretation
The patient is typically female and aged between 18 and 45 years. Check for:
- Painless loss of vision over hours to days, which may be subtle or profound, with a nadir at about 1 week. Determine the rapidity of onset.
- Reduced visual acuity, colour and contrast vision may occur
- Usually it is unilateral, but can be bilateral
- There may have been previous episodes
- There may be orbital pain associated with eye movements
- Other focal neurological symptoms may be present (e.g. paraesthesiase)
- features suggestive of an underlying cause (see Q4), e.g. history of multiple sclerosis
Q3. What are the features on examination?
Answer and interpretation
- Visual acuity — decreased
- Colour vision — decreased
- Visual fields — patchy defects may be present, often arcuate or central
- Pupils — a Marcus-Gunn pupil (a relative afferent pupilary defect or RAPD) may be present.
- Fundoscopy — usually normal (retrobulbar optic neuritis — “neither the patient nor the doctor sees anything!”), papillitis may be present (see below for a comparison with papilloedema).
- Neurological examination — assess for focal neurological defects.
Q4. What are the causes of this condition?
Answer and interpretation
- multiple sclerosis
- familial
- idiopathic
- inflammation
- viral — e.g. infectious mononucleosis, herpes zoster, viral encephalitischildhood infections or vaccinations — e.g. measles, mumps, chickenpoxGranulomatous inflammations — e.g. tuberculosis, syphilis, sarcoidosis, cryptococcusContiguous inflammation of the meninges, orbit, or sinuses.
The differential includes optic neuropathies such as:
- toxic optic neuropathy — e.g ethambutol, chloroquine, nicotine, alcohol
- metabolic optic neuropathy — vitamin B12 deficiency
- ischemic optic neuropathy — diabetes mellitus, giant cell arteritis, atherosclerosis
- compressive optic neuropathy — e.g. orbital tumour, intracranial mass
Q5. What are the Pulfrich phenomenon and Uhthoff sign?
Answer and interpretation
Both of these are occasionally present in optic neuritis:
- Pulfrich phenomenon — altered perception of moving objects
- Uhthoff sign — worsening of optic neuritis symptoms with exercise or increase in body temperature
Q6. What is the role for oral corticosteroids in the early management of this condition?
Answer and interpretation
There is no role — if you’re going to give steroids, give them IV!
There is an increased risk of optic neuritis recurrences in patients treated with oral prednisone.
Q7. What are the effects of steroids on this condition?
Answer and interpretation
Steroid therapy has been found to:
- reduce the risk of initial progression from optic neuritis to clinically definite multiple sclerosis for 3 years, but had no effect at 5 years.
- increases rate of vision return (at 1 and 3 weeks) but does not improve the final visual outcome (at 8 weeks) or alter the frequency of recurrences.
Q8. What is the investigation and management of this condition?
Answer and interpretation
- Urgent ophthalmology referral.
- consider FBC, ESR, CRP and work up of possible inflammatory/ infectious causes.
- consider MRI — especially if atypical or a first episode, usually in consultation with the ophthalmology or neurology service.
In a first episode of optic neuritis or a patient who has not been diagnosed with multiple sclerosis:
- A 14 day course of steroids starting with methylprednisolone 1 g/day IV for 3 days is given if there is any evidence of demyelination on MRI, and may be given even if the the MRI is negative.
Patients known to have multiple sclerosis or have had previous optic neuritis are not treated with steroids and are observed.
Q9. What percentage of people presenting with this condition develop multiple sclerosis at 5 years?
Answer and interpretation
About 30%.
References
- Beck RW, Cleary PA, Trobe JD, Kaufman DI, Kupersmith MJ, Paty DW, Brown CH. The effect of corticosteroids for acute optic neuritis on the subsequent development of multiple sclerosis. The Optic Neuritis Study Group. N Engl J Med. 1993 Dec 9;329(24):1764-9. PMID: 8232485.
- The 5-year risk of MS after optic neuritis. Experience of the optic neuritis treatment trial. Optic Neuritis Study Group. Neurology. 1997 Nov;49(5):1404-13. PMID: 9371930.
- Patel V, Oetting TA. Optic Nerve Drusen: 19 year-old female with blurred vision. EyeRounds.org
- Sellebjerg F, Nielsen HS, Frederiksen JL, Olesen J. A randomized, controlled trial of oral high-dose methylprednisolone in acute optic neuritis. Neurology. 1999 Apr 22;52(7):1479-84. PMID: 10227638.
- Ehlers JP, Shah CP, Fenton GL, Hoskins EN. The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease Lippincott Williams & Wilkins
- NSW Statewide Opthalmology Service. Eye Emergency Manual — An illustrated Guide. [Free PDF]
- Pulfrich C. Die stereoskopie im Dienste der isochromen und heterochromen photometrie. Die Naturwissenschaften 1922;10: Heft 25, 553–64
- O’Doherty M, Flitcroft DI. An unusual presentation of optic neuritis and the Pulfrich phenomenon. J Neurol Neurosurg Psychiatry. 2007 Aug; 78(8): 906–907. [PMC2117749]
- Uhthoff W. Untersuchungen über die bei der multiplen Herdsklerose vorkommenden Augenstörungen. Archiv für Psychiatrie und Nervenkrankheiten. 1890;21: 55-116 and 303-410.
OPHTHALMOLOGY BEFUDDLER
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
