That optic disc doesn’t look right…2
aka Ophthalmology Befuddler 009b [Patient 1] [Patient 2]
Patient 2
A elderly man is found in his home unconscious after his son was unable to contact him on the phone. As part of a neurological work up, funduscopy is performed.
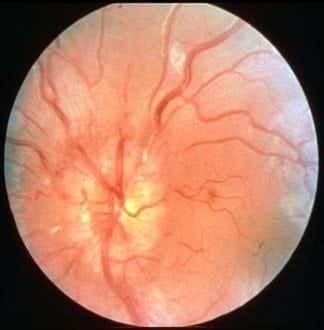
Findings similar to this are seen in the left eye:
Questions
Q1. What does funduscopy show?
Answer and interpretation
Papilloedema
The observed features include:
- swelling of the optic disc
- blurring of the disk margins
- hyperemia
- loss of physiologic cupping
- Flame-shaped hemorrhages and yellow exudates appear near the disk margins as edema progresses.
When observed in real time there may be obliteration of spontaneous venous pulsations (absent in 20% of normal people anyway).
Q2. What symptoms are usually associated with this finding?
Answer and interpretation
Papilloedema itself is usually asymptomatic.
There may be episodes of transient, often bilateral visual loss (lasting seconds), precipitated by rising from a lying or sitting position as a result of intracranial pressure changes.
Otherwise the presentation reflects the underlying cause and symptoms of raised intracranial pressure (e.g. headache and vomiting, worse in the morning) may be present.
Q3. Compare and contrast the expected examination findings of the conditions affecting Patient 1 and Patient 2
Answer and interpretation
Papillitis (optic neuritis):
- pupilary reaction — RAPD present
- visual acuity — reduced
- colour vision — red desaturation
- visual fields — large central scotoma
- pain on eye movement — present
- localisation — usually unilateral
- fundoscopy — blurred disc margins
Papilloedema:
- pupilary reaction — normal
- visual acuity — normal (transient loss)
- colour vision — normal
- visual fields — large blind spot, peripheral constriction
- pain on eye movement — present
- localisation — usually bilateral
- fundoscopy — blurred disc margins, no venous pulsation
Watch this RootAtlas video to see what spontaneous venous pulsations look like on funduscopy.
Q4. What are the possible underlying causes of this condition?
Answer and interpretation
Intracranial
- space-occupying lesions (e.g. neoplasms, trauma, infection, and vascular causes)
- benign intracranial hypertension (trauma, drugs, idiopathic, Addisons, sinus thrombosis)
- central venous sinus thrombosis
- meningoencephalitis
CSF
- hydrocephalus – obstructive, communicating (production vs. absorption of CSF)
- high CSF protein — e.g. Guillain-Barre Syndrome
Extracranial
- central retinal vein occlusion (CRVO)
- retro-orbital mass
- hypertension (grade IV)
When you perform funduscopy on the man’s other eye you see a similar appearance to this:

Q5. What is shown?
Answer and interpretation
Optic atrophy
Atophy is a misnomer — it is not a result of disuse!
Q6. What is the key feature of this condition on fundoscopy?
Answer and interpretation
A pale insipid optic disc (loss of the normal yellowish colour), with absence of normal physiological cupping.
Q7. What are the causes of this abnormality?
Answer and interpretation
Optic atrophy may be the end stage of:
- chronic papiloedema
- chronic optic neuritis
- glaucoma
- optic neuropathies (e.g. toxic, metabolic, ischemic and compressive)
- familial, e.g. retinitis pigmentosa
Q8. What is pseudopapilloedema?
Answer and interpretation
Pseudopapilledema mimics papilloedema and may result from the presence of optic disc drusen or a congenitally anomalous disc.
The optic disc is not truly swollen — the characteristic findings include:
- Vessels overlying the disc are not obscured
- the disc is not hyperemic
- surrounding nerve fiber layer is normal.
- spontaneous venous pulsations are usually present.
Further investigation may still be required to rule out raised intracranial pressure.
References
- Beck RW, Cleary PA, Trobe JD, Kaufman DI, Kupersmith MJ, Paty DW, Brown CH. The effect of corticosteroids for acute optic neuritis on the subsequent development of multiple sclerosis. The Optic Neuritis Study Group. N Engl J Med. 1993 Dec 9;329(24):1764-9. PMID: 8232485.
- The 5-year risk of MS after optic neuritis. Experience of the optic neuritis treatment trial. Optic Neuritis Study Group. Neurology. 1997 Nov;49(5):1404-13. PMID: 9371930.
- Patel V, Oetting TA. Optic Nerve Drusen: 19 year-old female with blurred vision. EyeRounds.org
- Sellebjerg F, Nielsen HS, Frederiksen JL, Olesen J. A randomized, controlled trial of oral high-dose methylprednisolone in acute optic neuritis. Neurology. 1999 Apr 22;52(7):1479-84. PMID: 10227638.
- Ehlers JP, Shah CP, Fenton GL, Hoskins EN. The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease Lippincott Williams & Wilkins
- NSW Statewide Opthalmology Service. Eye Emergency Manual — An illustrated Guide. [Free PDF]
OPHTHALMOLOGY BEFUDDLER
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
