The Aching Red Photophobic Eye
aka Ophthalmology Befuddler 016
A 60 year-old man presents to the emergency department with a painful and red right eye. The pain started yesterday, and has progressed to a deep ache radiating to his right temporal region. His eye pain is exacerbated by eye movements, reading and bright lights.

He has normal visual acuity but has direct and consensual photophobia in his right eye.
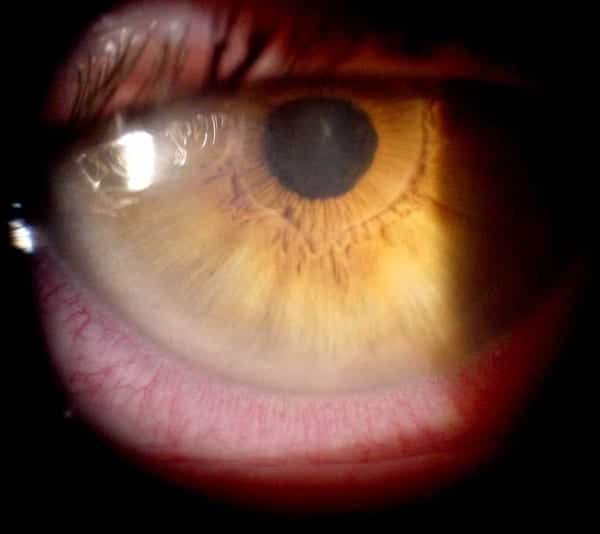
When you look more closely, you see this:
Questions
Q1. What is the likely diagnosis and what are the different types/ terms used to describe this condition?
Answer and interpretation
Uveitis, which unsurprisingly means inflammation of the uveal tract. Note the typical history and important findings of a constricted slightly irregular pupil with ciliary flush (i.e. circumcorneal involvement of the diffusely injected conjunctiva).
Different terms may be used for uveitis depending which components of the uveal tractare involved, such as:
- iritis — inflammation of the iris
- cyclitis — ciliary body
- choroiditis — choroid
Alternatively uveitis may be referred to as:
- Anterior uveitis — aka iridocyclitis, which involves inflammation of the anterior portion of the uveal tract and usually affects young or middle-aged persons.
- Posterior uveitis — which includes vitritis, choroiditis, retinitis, chorioretinitis, or retinochoroiditis.
- Panuveitis — aka diffuse uveitis, which refers to both anterior and posterior involvement.
Uveitis can be acute or chronic/ recurrent.
Q2. What are the underlying causes of this condition?
Answer and interpretation
There are many, many causes of uveitis!
There are 4 broad categories:
- inflammatory
- traumatic
- infectious
- drug-induced
Inflammatory causes
HLA B-27 associated: HLA antigen is present in 30—70% of patients with anterior uveitis, half of whom have an associated systemic disease such as:
- ankylosing spondylitis
- psoriatic arthritis
- reactive arthritis
- inflammatory bowel disease
Non-HLA-B27 associated uveitis may result from numerous underlying systemic conditions such as:
- sarcoidosis
- juvenile idiopathic arthritis
- Behçet disease
- Kawasaki disease
- Multiple sclerosis
- Granulomatosis with polyangiitis (GPA)
Infectious causes:
- Parasitic — e.g. toxoplasmosis (accounts for 25% of retinochoroiditis in the US)
- Viral — e.g. cytomegalovirus (CMV), herpes viruses, adenovirus, measles, mumps, influenza
- bacterial — e.g. tuberculosis, leptospirosis, syphilis
- ricketsial disease — e.g. Lyme disease
Traumatic causes:
- Traumatic iritis, usually secondary to a direct blow from a blunt object
Drug-induced:
- e.g. rifabutin, cidofovir, sulfonamides, pamidronate
NOTE: Uveitis can also occur secondary to other ocular conditions (e.g. lens-induced, post-operative, anterior segment ischemia, tumour).
Q3. What features of this condition should be consider on taking a history?
Answer and interpretation
History:
Anterior uveitis:
- Painful red eye — deep ache radiating to periorbital or temple area, worse with movement and accommodation.
- photophobia.
- +/- blurred vision
Posterior uveitis
- “floaters” and visual changes: blind spots or flashes may be present with retinal involvement.
- Redness or significant pain are usually absent
Features of an underlying cause (see Q2) — inflammatory (HLA-B27 vs non-HLA-B27 associated conditions), infectious traumatic, or drugs.
Duration and previous episodes?
Q4. What are the features of this condition on examination?
Answer and interpretation
Examination:
- Visual acuity: often normal, but may be reduced in posterior uveitis
- Pupils: constricted, may be irregular, and is sluggish in response to light in comparison with the uninvolved eye. Direct and consensual photophobia (the latter may help differentiate anterior uveitis from from superficial causes of photophobia).
- Red reflex — may be normal or altered, e.g. secondary cataract.
- Tonometry — check for secondary glaucoma
Fundoscopy — look for evidence of chorioditis and retiinits, or complications such as retinal detachment.
Slit lamp:
- Conjunctiva — diffusely injected conjunctiva with circumcorneal involvement aka ‘ciliary flush’ (no perlimbal sparing as occurs in conjunctivitis). Tearing, but no purulent discharge.
- Cornea —keratitic precipitates (deposits of white blood cells on the endothelium) may be visualized and are a hallmark of iritis. There are two types: nongranulomatous (small-medium) and granulomatous (large — e.g. sarcoidosis).
- Anterior chamber — cloudy anterior chamber due to inflammatory cells and proteinaceous flare. Synechieae (adhesions of the iris to the cornea or lens) may be present. Look for a hypopyon.
- Posterior chamber — cells and flare may be present in posterior uveitis.
RootAtlas has nice brief videos of nongranulmatous and granulomatous KPs, as well as an excellent ‘must see’ video demonstrating ‘cells and flare’ in the anterior chamber.
Q5. What investigations are required?
Answer and interpretation
Investigations are rarely required as part of the emergency management of uveitis, however they may expedite subsequent treatment.
Investigations may not be required if:
- known underlying cause (e.g. sarcoidosis or drugs)
- mild unilateral nongranulomatous disease with no evidence of systemic disease
Infectious uveitis, although rare, must be ruled out before treatment with immunosuppressive agents. Sometimes it is only suspected after a failure of treatment.
Investigations may include:
- identification of specific findings on ophthalmologic and general examination
- infectious work up — specific serology testing (e.g. syphilis), PCR, and cultures (e.g. STD screen), HIV tests
- HLA-B27 typing
- CXR and/or CT chest if pulmonary symptoms — e.g. sarcoidosis, tuberculosis
- Imaging of the sacroiliac joints if suspected spondyloarthropathy as a diagnosis.
- Colonoscopy if gastrointestinal symptoms or heme-positive stools — e.g. inflammatory bowel disease
Q6. What severe sight-threatening complications may occur as a result of this condition?
Answer and interpretation
Important complications include:
- cataracts
- glaucoma (e.g. due to synechiae)
- retinal detachment
- ophthalmitis
Q7. Describe the management of this condition.
Answer and interpretation
- Urgent referral to ophthalmology.
- Seek and treat underlying causes.
- Treat complications e.g. glaucoma
- Mydriatics (eg, sympathomimetics like phenylephrine HCl) — prevent the formation of synechiae by pupillary dilation.
- Parasympatholytic agents (eg, atropine, cyclopentolate) — produce both mydriasis and cycloplegia reducing pain and photophobia
Treat with corticosteroids after consultation with an ophthalmologist and consideration of a possible infectious etiology:
- Topical corticosteroids (eg, prednisolone acetate 1%) — useful for anterior uveitis, but due to poor penetration are less effective for posterior uveitis
- Systemic corticosteroid therapy — usually reserved for bilateral disease that is refractory to local medication or for patients with significant ocular disability or retinitis
Other immunosuppressants — may be used in steroid-dependent or refractory uveitis.
Q8. What is the appropriate disposition of a patient with this condition?
Answer and interpretation
All cases of uveitis should be discussed with an ophthalmologist.
- Uncomplicated noninfectious uveitis — outpatient management with ophthalmology follow up within 24 hours.
- Refractory or infectious uveitis — usually require admission and further work up
Q9. What is the classic pattern of this condition when it is associated with HLA-B27?
Answer and interpretation
Bilateral recurrent alternating anterior uveitis

Q10. What can be seen in the anterior chamber in the above image?
Answer and interpretation
Hypopyon
With severe inflammation leukocytes can settle in the anterior chamber and form a hypopyon, which is a white or yellowish accumulation of purulent material.
References
- Ehlers JP, Shah CP, Fenton GL, Hoskins EN. The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease Lippincott Williams & Wilkins
- NSW Statewide Opthalmology Service. Eye Emergency Manual — An illustrated Guide. [Free PDF]

OPHTHALMOLOGY BEFUDDLER
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
