Third disease
Rubella (German measles)
Rubella (German measles) is a contagious viral exanthem with generally mild symptoms in children but devastating consequences during pregnancy. It is caused by the rubella virus, a single-stranded RNA virus of the genus Rubivirus in the Matonaviridae family (formerly Togaviridae).
The virus spreads via respiratory droplets and has a predilection for the 5–9 year age group. Before widespread immunisation, rubella epidemics occurred every 6–9 years.
Acquired rubella typically presents with low-grade fever, postauricular lymphadenopathy, and a maculopapular rash beginning on the face and spreading downwards. Forchheimer spots may appear on the soft palate. Up to 60% of adolescent females experience arthralgia. The infected individual is contagious from 7 days before until 7 days after the rash appears.
Congenital Rubella Syndrome (CRS) results from maternal infection during early pregnancy, particularly within the first 10 weeks of gestation. CRS can cause a triad of deafness, cardiac defects, and cataracts, along with microcephaly, hepatosplenomegaly, and developmental delay. Rubella vaccination (introduced in 1969) has dramatically reduced CRS in countries with established immunisation programs.
Synonyms of third disease: Rubella, rötheln, röteln, German measles, rubeola sine catarrho, rubeola notha (Babington), bastard or hybrid measles, rosalia idiopathica (Richardson), essera Vogelii, little red, little measles, thre-day-measles.
English physician Clement Dukes (1845–1925) introduced the numbering system for childhood exanthems in 1900. He categorised them by clinical presentation into: First: measles; Second: scarlet fever; Third: rubella; and Fourth: Filatov-Dukes disease. Later additions – Fifth: erythema infectiosum (1905, Cheinisse); and Sixth: roseola infantum (1910, Dreyfus)
Clinical Manifestations
- General features: Often mild or subclinical, especially in children. Symptoms may include low-grade fever, malaise, sore throat, and headache.
- Lymphadenopathy: Hallmark feature — tender, generalised lymphadenopathy, especially postauricular, suboccipital, and cervical nodes. Can precede the rash by 5–7 days and persist after it fades.
- Arthralgia/arthritis: Common in adolescent girls and women (~60%), often affecting fingers, wrists, and knees; usually transient.
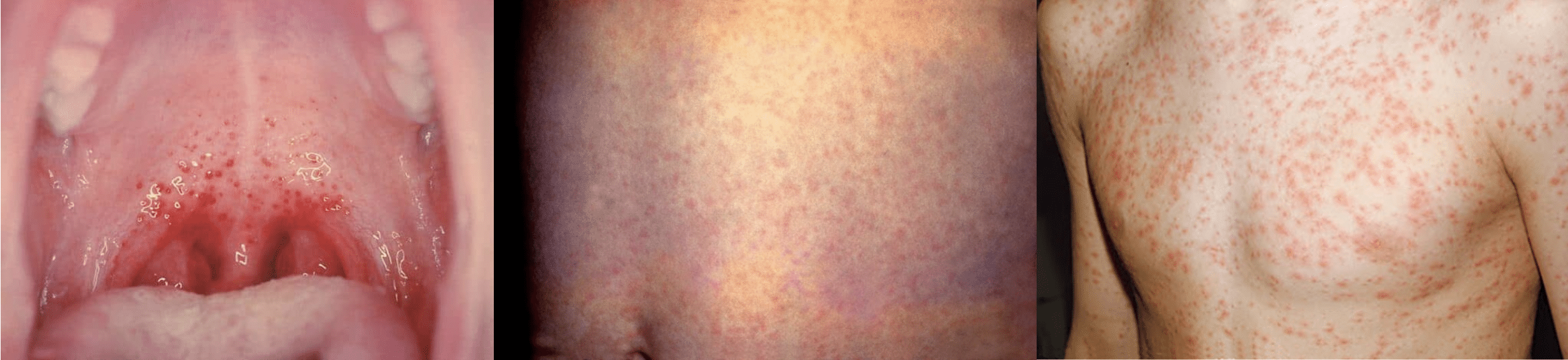
- Rash: Faint pink maculopapular eruption starting on the face → spreading caudally to trunk and limbs within 24h.
- May coalesce, particularly on the trunk
- Resolves within 1–3 days in same order as it appeared
- Often accompanied by desquamation
Key Signs
- Forchheimer spots: Discrete red petechiae on soft palate (~20% of cases); not pathognomonic.
- Lymphadenopathy pattern: Tender posterior cervical and postauricular nodes are strongly suggestive of rubella in the context of rash.
- Non-specific viral prodrome: May mimic mild upper respiratory infection.
Diagnosis
Primarily clinical in outbreak settings. Confirmatory tests include:
- Rubella-specific IgM antibodies (serology)
- RT-PCR for rubella RNA (throat, nasal, or urine samples)
- Paired serology showing IgG seroconversion (especially useful for retrospective CRS diagnosis)
Treatment
- Supportive care only – hydration, antipyretics, rest
- No antiviral therapy available
- Isolation for 7 days after rash onset to prevent spread, especially to pregnant contacts
Differential Diagnosis
- Other exanthems: Measles, scarlet fever, roseola, parvovirus B19
- Mononucleosis (EBV/CMV): particularly with prominent pharyngitis and lymphadenopathy
- Drug eruptions and enteroviral infections
- Zika virus: relevant in tropical/travel medicine context due to similar rash and CRS risk
Complications
- Acquired rubella: typically self-limiting; rare complications include thrombocytopenia, encephalitis, and neuritis
- Congenital Rubella Syndrome (CRS):
– Occurs when infection acquired during pregnancy (esp. <10 weeks)
– Classic triad: sensorineural deafness, cataracts, and congenital heart disease
– Other findings: microcephaly, hepatosplenomegaly, developmental delay, blueberry muffin lesions
– Infants with CRS can shed virus for up to a year → infection risk to others
History of third disease – rubella
1619 – Daniel Sennert (1572-1637) of Wittenberg described the disease under the name of ritteln or rotteln as belonging to the class of measles but less dangerous
ad morbillos procul dubio pertinent Ritteln vel Rotteln, a rubore procul dubio sic dicta exanthemata…minus tamen quam vulgares morbilli periculosus.
1814 – William George Maton (1774-1835) published ‘Some Account of a Rash Liable to be Mistaken for Scarlatina‘ describing characteristic features of the disease including: contagion, lymphadenopathy, and mild symptoms.
…it seems requisite to form a new designation, which, however, I do not venture to propose at present, being satisfied with calling the attention of my colleagues to the subject, and being persuaded that the above is much too loose a sketch, from which to frame formal nosological characters.
1821 – Adolph Christian Heinrich Henke (1775-1843) summarised the German experience of Rötheln as a disease distinct from scarlet fever and measles; credited Bräuner (1713); De Bergen (1752); Ludwig and Orloff (1758); Fritsch (1786); and Selle (1789).
1840 – Robert Paterson (1809-1885), of Leith, Scotland was the first physician to publish in English on the nature of Rötheln as a distinct disease in his paper ‘An Account of the Rötheln of German Authors, together with a few Observations on the Disease as it has been seen to Prevail in Leith and its Neighbourhood‘
…the generality of continental authors in using the word Morbilli to signify the measles, Scarlatina the scarlet fever, and the intermediate disease Rubeola. German authors in general call it Rötheln or feüermasern. I fear that the adoption of the word rubeola for this disease would produce confusion in medical nomenclature. I shall therefore use the German word Rötheln.
1850s – The term ‘German measles‘ was used in common parlance to describe the condition first distinguished from scarlet fever and measles by German physicians, though not everybody agreed:
With regard to the name, ‘German measles‘ – its usual trite designation here – seems unexceptionable for common use; while, for more learned occasions, ‘rubeola‘ seems more decidedly to mark a distinct disease, than any other yet proposed.
1864 – An anomalous exanthem was epidemic in the metropolis. Benjamin Ward Richardson (1828-1896) felt the exanthem was another disease emulating scarlet fever, but distinct from it, and proposed the term Rosalia idiopathica. Benjamin Guy Babington (1794-1866) directed the attention of the Epidemiological Society of London to the outbreak:
From the general resemblance of this eruptive epidemic to rubeola I, would propose to designate it Rubeola notha, or bastard measles
1866 – Henry Richard Lobb Veale (1832-1908) proposed the term Rubella [Latin: rubellus, diminutive for red (i.e. little red)]:
Rötheln is harsh and foreign to our ears. Rubeola notha and rosalia idiopathica are too long for common use and are certainly expressive of conclusions which have yet to be proved. I therefore venture to propose Rubella as a substitute.
1881 – Rubeola, Rötheln or German Measles, formally recognised as an individual entity, at the seventh session of the International Medical Congress on diseases in children held in London. The following entries appear in the Nomenclature of the Royal College of Physicians:
- 1884 – Epidemic rose rash. Synonyms: Rötheln. German measles, Rubeola, Rubella.
- 1896 – Rubella. Synonyms: Rötheln. German measles, epidemic rose rash
- 1906 – German measles. Synonyms: Epidemic rose rash.
- 1917 – Rubella. Synonyms: German measles.
- 1931 – German measles. Synonyms: Rubella, Röteln. (the word röteln first appears without an h.)
1898 – Frederick Forchheimer (1853-1913) reviewed the world literature on enanthem (rash on the mucous membranes) to differentiate rubella from German measles and scarlet fever. He examined 22 cases during a rubella epidemic documenting a consistent enanthem appearing simultaneously with the exanthem.
…a macular, distinctly rose-red eruption upon the velum of the palate, the uvula, extending to but not on to the hard palate. These spots were arranged irregularly, not crescentically; were the size of large pin-heads, were very little elevated above the level of the mucous membrane, and did not seem to produce any reaction upon it. Six hours after this, the enanthem had become decidedly paler, the infiltration very much less, and by the next morning it had disappeared.
1938 – Hiro & Tasaka (Japan) Experimentally transmitted rubella between children via nasal filtrates, though the virus itself remained unidentified.
1941 – Congenital rubella syndrome (CRS) first described. Australian ophthalmologist Sir Norman McAlister Gregg (1892-1966) first reported the association between congenital cataracts and rubella during the first trimester of pregnancy. The earliest recognition that an environmental exposure, specifically a virus, could cause birth defects.
1962 – Thomas Weller isolated rubella virus in cell culture. Serological assays revealed CRS was due to both teratogenic and chronic foetal infection.
1964-1965 US Rubella Epidemic; 12.5 million cases, 20,000 CRS cases, and 2,000+ deaths. Identified wide CRS spectrum including deafness, cardiac lesions, and developmental delays.
1967 American physician, Stanley Alan Plotkin (1932- ) developed the RA27/3 rubella vaccine while working at Wistar Institute in Philadelphia. The most widely administered rubella-containing vaccines use the attenuated RA27/3 strain.
1971 – MMR vaccine licensed (US). Combined measles, mumps, and rubella (MMR) vaccine was licensed for use in the United States, with the current rubella vaccine component (RA27/3)
2005 – MMRV licensed. Tetravalent formulation including varicella (chickenpox) introduced in multiple countries.
2015 – Rubella elimination in the Americas. Declared free of endemic rubella and CRS transmission by the WHO — a global milestone.
2021 – Global progress. 89% of WHO member states included rubella-containing vaccines in routine immunisation schedules.
Associated Persons
- Daniel Sennert (1572-1637) – Early description of ritteln/rotteln as a mild measles-like illness
- William George Maton (1774-1835) – First to clinically differentiate rubella from scarlet fever in English literature
- Robert Paterson (1809-1885) – Clarified Rötheln as distinct from measles and scarlet fever
- Benjamin Ward Richardson (1828-1896) – Proposed the term Rosalia idiopathica
- Benjamin Guy Babington (1794-1866) – Suggested Rubeola notha (“bastard measles”)
- Henry Richard Lobb Veale (1832-1908) – Coined the term Rubella to replace Rötheln
- Clement Dukes (1845-1925) – proposed the numbered classification of paediatric exanthems
- Frederick Forchheimer (1853–1913) – Identified Forchheimer spots, aiding diagnosis of rubella
- Norman McAlister Gregg (1892-1966) – Discovered Congenital Rubella Syndrome, linking maternal rubella to birth defects
- Thomas Weller (1915–2008) – Isolated rubella virus in tissue culture, enabling vaccine development.
- Stanley Alan Plotkin (1932- ) – Developed the RA27/3 rubella vaccine, cornerstone of global immunisation
References
- Maton WG. Some Account of a Rash Liable to be Mistaken for Scarlatina. Medical transactions 1815; 5: 149-165
- Henke ACH. Die Rötheln. Handbuch zur Erkentniss und Heilung der Kinderkrankheiten
- Paterson R. An Account of the Rötheln of German Authors, Together with a Few Observations on the Disease as It Has Been Seen to Prevail in Leith and Its Neighbourhood. Edinb Med Surg J. 1840 Apr 1;53(143):381-393.
- Babington BG. Rubeola notha. Half-yearly abstract of the medical sciences. 1865; 41: 292-294
- Veale H. History of an Epidemic of Rötheln, with Observations on its Pathology. Edinburgh Medical Journal, 1866; 12: 404-414
- Diseases in children. Transactions of the international Medical Congress. 1881
- Hess AF. German measles (rubella): an experimental study. Archives of internal medicine, 1914; 13(6): 913-1916
- Rolleston JD. German measles. In: The history of the acute exanthemata: the Fitzpatrick lectures for 1935 & 1936
- Hiro Y, Tasaka S. Die Röteln sind eine Viruskrankheit. Monatsschrift für Kinderheilkunde 1938; 76: 328-332.
- Gregg NM. Congenital cataract following German measles in the mother. Transactions of the ophthalmological society of Australia. 1941; 3: 35–41
- Plotkin SA, Vaheri A. Human fibroblasts infected with rubella virus produce a growth inhibitor. Science 1967; 156: 659–661.
- Plotkin SA, Farquhar JD, Katz M, Buser F. Attenuation of RA 27–3 rubella virus in WI-38 human diploid cells. Am J Dis Child 1969; 118: 178–85.
- Winter AK, Moss WJ. Rubella. Lancet 2022; 399(10332): 1336-1346
eponymictionary
the names behind the name
BA MA (Oxon) MBChB (Edin) FACEM FFSEM. Emergency physician, Sir Charles Gairdner Hospital. Passion for rugby; medical history; medical education; and asynchronous learning #FOAMed evangelist. Co-founder and CTO of Life in the Fast lane | On Call: Principles and Protocol 4e| Eponyms | Books |
