Trauma Under Pressure
aka Trauma Tribulation 034
A young man was riding his motorcycle in a country town when he hit a car bonnet at 60-90 km/hr and was thrown a long distance through the air. He presents by ambulance to your regional ED, 200km from the city, with a sore chest, a scrape on his helmet. There was an obvious right pneumothorax on arrival and you sensibly inserted an ICC while waiting for Xray. His vitals after the ICC insertion were: GCS 15. HR 98. BP 150/80, RR 18, SpO2 100% on oxygen.
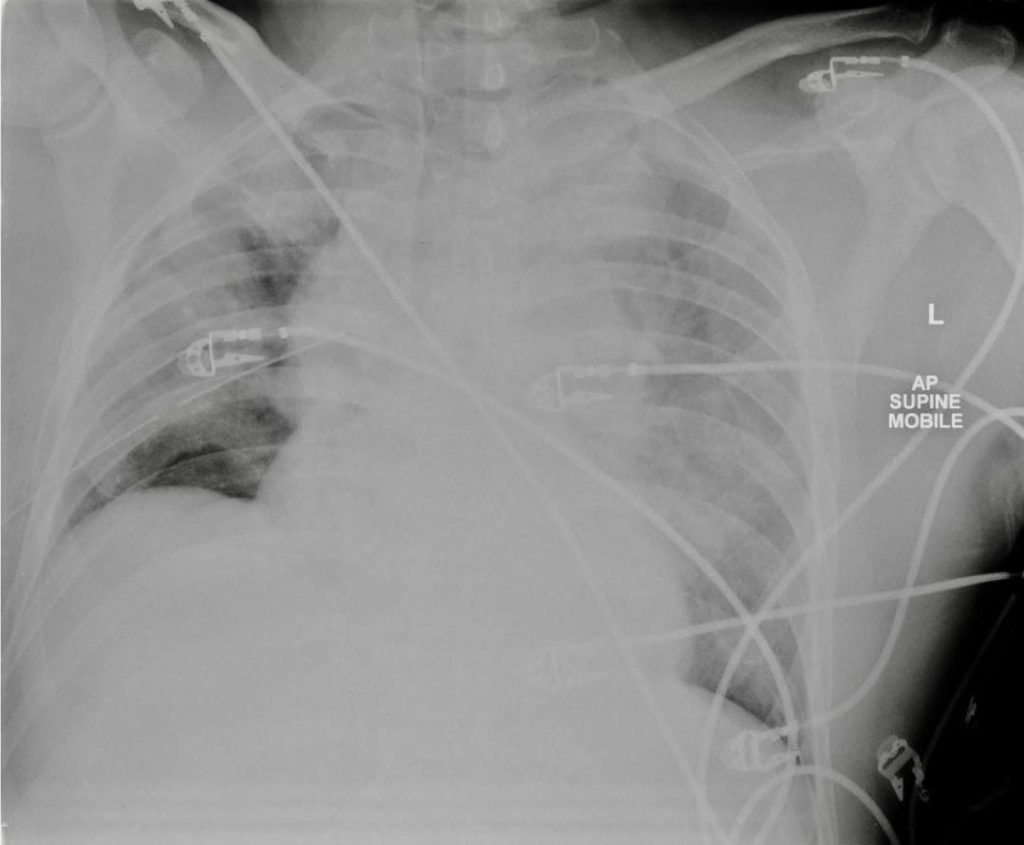
You now obtain the following CXR:
Questions
Q1. Describe and interpret the CXR
Answer and interpretation
This is not a happy CXR.
While there is debate about exactly what constitutes a widened mediastinum, there are times when it is just wide.
This is a traumatic aortic injury until proven otherwise.
It is tempting to ‘gild the lilly’ and say that the trachea is deviated to the right and that the left main bronchus is depressed however the film is rotated to the right which throws the trachea across and we have always found depression of the left main bronchus a dubious sign.
While we are on the topic, how wide is wide?
- Searching the literature on this returns a collection of fairly small retrospective case-control studies only and all disagree with each other.
- Our favourite is Burney et al (1983) which showed that subjective impression was better than measurement.
- Others have suggested a mediastinal width of 8cm in adults or various ratios of mediastinum (Wong et al, 2004) to chest or claimed that they are all useless (Marnocha et al, 2004).
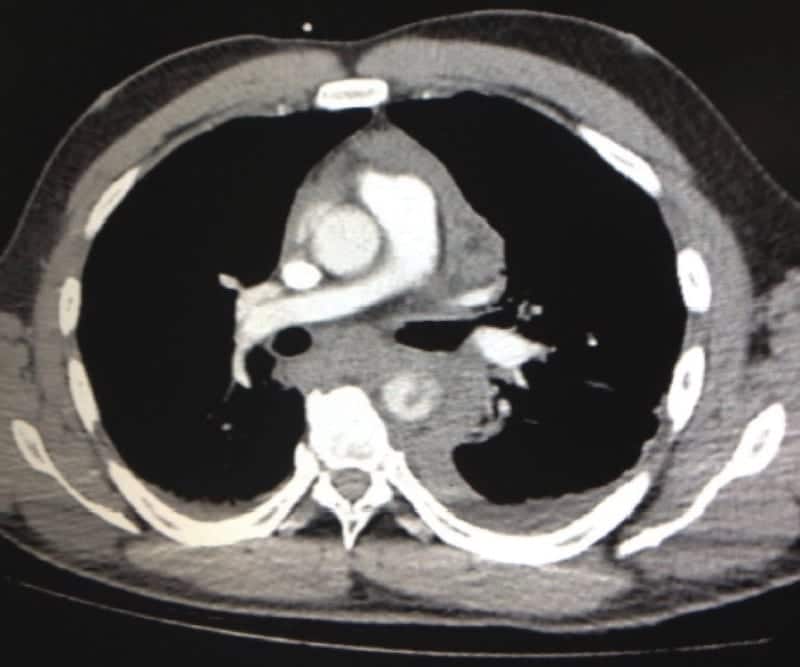
Wisely, you go on to organise further imaging. This is a slice of your subsequent CT:
Q2. What does the CT image show?
Answer and interpretation
Of course, it isn’t fair to be shown only one slide of a CT… after all, when does that ever happen in real life..?. Oh yeah, in Fellowship exams.
This is a single transverse slice of a contrast CT scan of the chest at the level of the pulmonary trunk demonstrating a rupture of the thoracic aorta.
Contrast is seen filling the ascending aorta and pulmonary trunk but there is either delayed opacification or a filling defect of the descending aorta (more slices are needed to tell which – in fact it was filling defect from dissection flaps). The descending aorta is shrouded in haematoma and there is a hint of fresh contrast settling posteriorly in that haematoma. There is a pleural effusion on the left which does not contain contrast but which is probably blood from the same injury that has spilt into the pleural space earlier. The oesophagus and trachea are deviated to the right, pushed aside by the haematoma.
Suspect traumatic aortic injury if deceleration injury, side impact motor vehicle crash, fall >10 metres, or if there is steering column or wheel damage in a motor vehicle crash.
Q3. What is the best way to measure this man’s blood pressure?
Answer and interpretation
Intra-arterial blood pressure monitoring
The aorta is currently held together by a fragile gel of clotted blood. The non-invasive BP may not be trustworthy in this circumstance. As in the case of aortic dissection, there is considerable baroreceptor dysfunction in these cases leading to maladaptive reflex hypertension and tachycardia.
In this case an arterial line was inserted and demonstrated a radial artery BP of 195/90 mmHg when the NIBP was reading 150/90 mmHg.
Q4. Can we draw on the small amount of useful literature addressing hypotensive resuscitation in trauma to guide the management of this patient?
Answer and interpretation
No
These patients aren’t often hypotensive as a result of their aortic injury (unless they’re going to be dead from aortic exsanguination in a few minutes) – they may often be hypotensive for other reasons though.
Q5. Can we draw on animal literature in this setting?
Answer and interpretation
Maybe.
There are always small animal models of aortic injury that demonstrate you will rebleed if you crank the BP up high enough. Sondeen et al (2005) suggests it doesn’t matter when or how you give the fluid, you will bleed like a stuck pig if the BP gets high enough. However, extrapolating from pigs to humans may not be wise.
Q6. What does the aortic dissection literature tell us?
Answer and interpretation
We know that not only blood pressure but also left ventricular ejection velocity determines the stresses in the aortic wall and subsequent extension.
That’s why B blockers are preferred – they decrease blood pressure, decrease the number of heart beats causing stress, decrease ejection velocity, and counter the tachycardia that may be induced while using vasodilators (Marik and Varon, 2007).
Vasodilators are added on top of this. There is no data to validate one blood pressure target over another, usual protocols to target 120 systolic or MAP <80 mmHg (Estera et al, 2006). We know that some blood pressures are difficult to treat and some people progress their aortic catastrophe despite medical therapy (Marik and Varon, 2007).
Q7. What is a good common sense approach to blood pressure management in this case?
Answer and interpretation
Using the principles of decreasing aortic wall stress mentioned above, we can tailor our BP target to something sensibly low such as:
SBP 100 to 120 mmHg and MAP 60 to 80mmHg
However, you might want more generous targets if there is a concomitant head injury. In this setting if you lower the BP too much you might contribute to the secondary injury to the patient’s brain by dangerously decreasing cerebral perfusion pressure.
We can also be modest in our blood pressure resuscitative efforts of other injuries.
Q8. What drugs will you use to lower the blood pressure and what order?
Answer and interpretation
In this case the patient was given 5mg boluses of IV metoprolol (25mg in total) followed by a GTN infusion.
A useful approach is to use beta blockers to lower the heart rate to 60 to 75/min then titrate the GTN to achieve the blood pressure target.
An alternative to metoprolol is to use esmolol which has the advantage of being an ultrashort-acting β-blocker that is easily titrated. After mixing 5 g in 500 ml 5% glucose, give an initial bolus of 500 μg/kg followed by an infusion of 50 to 200 μg/kg/min. Most ED staff are much more familiar with IV metoprolol however…
Q9. Why use GTN in preference to sodium nitroprusside?
Answer and interpretation
Ask yourself these questions:
- Where is our nitroprusside kept?
- How is it made up?
- When was the last time I used it?
- When was the last time any of our resus nurses used it?
- When was the last time any of our paramedics used it?
- Do I have to do something with alfoil? Or cyanide? Or something?
When time is really short it is not the time to be extra clever. It is time to be effective with the things that you know backwards. Now if you are using nitroprusside very day then that is the drug to use but I suspect you and your nurses and paramedics are much more familiar with GTN. More importantly, GTN seems to do the job.
Q10. What is your approach to ensuring this patient receives timely definitive care?
Answer and interpretation
Clearly this is a time critical injury.
Your choice of platform with depend on where you are and what your ambulance and retrieval service can offer, taking into account weather, other missions, staff availability and so on.
At our place there is no helipad and we are looking at around 30 minutes by ambulance out to the airport. There is however a helicopter waiting at that airport most of the time. If the weather is good the helicopter certainly beats the road for us for a trip to the trauma centre. Make sure you consider things like how the patient is to get out to the airport. If we wait for the flight intensive care paramedic to come in and collect the patient we are adding at least 30 minutes onto transfer time. If we try to put him in an ambulance with a road paramedic we may get someone who is unable to run a GTN infusion and are likely to get someone who is unable to give titrated beta-blocker. Add the intercostal catheter and you have a complex transfer.
In this case we sent an EM registrar with the patient to the airport.
The metoprolol was delivered over the course of the thirty minute trip and the patient was loaded onto the aircraft with a BP 110/60 and HR 60. This is not our standard procedure and it left us a doctor down for an hour but when there is one patient in your ED that day who stands a good chance of dying from a correctable problem that patient really needs to be your priority.
References
- Bickell WH, Wall MJ Jr, Pepe PE, Martin RR, Ginger VF, Allen MK, Mattox KL. Immediate versus delayed fluid resuscitation for hypotensive patients with penetrating torso injuries. N Engl J Med. 1994 Oct 27;331(17):1105-9. PubMed PMID: 7935634. [Free Fulltext]
- Burney RE, Gundry SR, Mackenzie JR, Wilton GP, Whitehouse WM, Wu SC. Comparison of mediastinal width, mediastinal-thoracic and -cardiac ratios, and “mediastinal widening” in detection of traumatic aortic rupture. Ann Emerg Med. 1983 Nov;12(11):668-71. PubMed PMID: 6638627.
- Estrera AL, Miller CC 3rd, Safi HJ, Goodrick JS, Keyhani A, Porat EE, Achouh PE, Meada R, Azizzadeh A, Dhareshwar J, Allaham A. Outcomes of medical management of acute type B aortic dissection. Circulation. 2006 Jul 4;114(1 Suppl):I384-9. PubMed PMID: 16820605. [Free Fulltext]
- Marik PE, Varon J. Hypertensive crises: challenges and management. Chest. 2007 Jun;131(6):1949-62. Review. Erratum in: Chest. 2007 Nov;132(5):1721. PubMed PMID: 17565029.
- Marnocha KE, Maglinte DD, Woods J, Goodman M, Peterson P. Mediastinal-width/chest-width ratio in blunt chest trauma: a reappraisal. AJR Am J Roentgenol. 1984 Feb;142(2):275-7. PubMed PMID: 6607590. [Free Fulltext]
- Sondeen JL, Coppes VG, Holcomb JB. Blood pressure at which rebleeding occurs after resuscitation in swine with aortic injury. J Trauma. 2003 May;54(5 Suppl):S110-7. PubMed PMID: 12768112.
- Wong YC, Ng CJ, Wang LJ, Hsu KH, Chen CJ. Left mediastinal width and mediastinal width ratio are better radiographic criteria than general mediastinal width for predicting blunt aortic injury. J Trauma. 2004 Jul;57(1):88-94. PubMed PMID: 15284554.
- LITFL CCC — Permissive Hypotension
- Radiopaedia — Thoracic Aortic Injury
- Resus.ME — Traumatic Aortic Injury
- Trauma.org — Traumatic Aortic Injury
Case by Dr Ben McKenzie and Dr Mark Putland of EDCentral.com.au
CLINICAL CASES
Trauma Tribulation
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC