Ultrasound Case 053
Presentation
A 23 year old surfer presents several weeks after sustaining a foot injury with some mild swelling and pain in his mid plantar arch.
2 weeks previously he had been running along the rocks when he stood on something sharp. A small wound was present however his surfing desire proved stronger than his nociceptive instinct and he returned to the waves.
View 2
Describe and interpret these scans
IMAGE INTERPRETATION
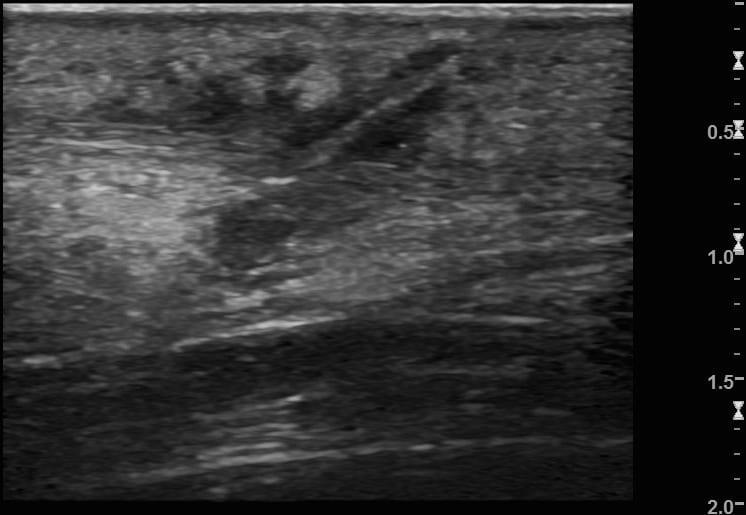
Image 1: Transverse foot, plantar surface, slowly sliding the probe along the medial longitudinal arch from the proximal (heel end) distally (toward the toes) where a small wound lay.
A small hypoechoic collection is seen (note the scale). Within this lie two echogenic spines. They are imaged in transverse section appear only as bright dots that become more superficial as they are scanned toward the entry point. One of the foreign bodies ends 2-3mm deep to the skin, the other ends at the skin surface.
Image 2: Image 1 with FB marked.
Image 3: Longitudinal image of the FB and associated collection.

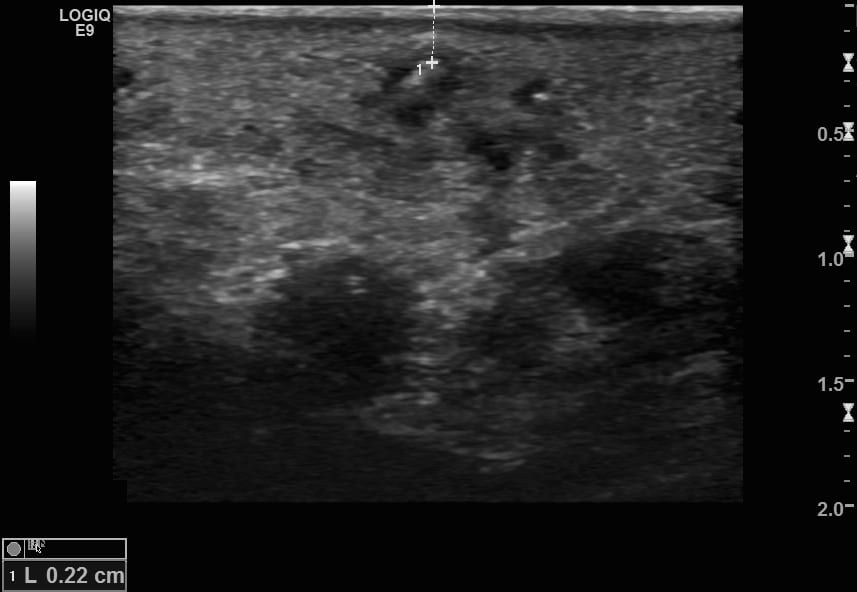
Image 4: Transverse view of the superficial end of the deeper FB – 2.2mm below the skin surface.
Image 5: Longitudinal image of the more superficial FB which measured 7mm in length.
Image 6: Transverse view of the shallow end of the superficial FB – at the skin surface.
CLINICAL CORRELATION
Sea urchin spines in plantar surface of foot.
Foreign body removal is difficult. The echogenicity, size, direction of penetration and patient cooperation vary greatly and present the clinician with a considerable challenge.
Success involves a number of key steps.
- Find the foreign body – explore with a high frequency transducer in many different directions and tangents. Look for the FB with may be echogenic – or may only cause posterior acoustic shadowing. A penetrating FB will usually be splinter like in shape.
- Measure the FB’s length. Also measure the depth of the most superfical part of the FB.
- Consider whether the procedure should be done in the operating theatre. Advantages include time and staff factors, patient anaethesia (general or regional), better equipment and lighting, improved exposure and ability to wash out optimally, ability to identify and preserve any important adjacent anatomical structures and use of image intensification. In this case the patient requested minimal intervention and as the foreign bodies lay within several milimeters of the skin the decision to proceed in the Emergency Department was made.
- Ensure good analgesia – a regional block is best and in this case this was achieved with an ulrasound guided posterior tibial nerve block. Never inject air superficial to the FB or imaging will be lost.
- Ensure a bloodless field – I used a Bier’s block cuff over the calf in this case.
- Use a sterile probe cover and use aseptic technique.
- Meticulously measure and mark out the FB and decide on your approach – there are several techniques. I usually make a transverse incision toward the superfical end of the FB and carefully dissect down until finding my target.
- If you fail after a couple of attempts stop. A fresh set of eyes in the completely controlled setting of an operating theatre will be better. Also remember it is far easier to remove a foreign body after a few days, when it becomes encapsulated and surrounded by a rim of inflammatory fluid.
[cite]
TOP 100 ULTRASOUND CASES
An Emergency physician based in Perth, Western Australia. Professionally my passion lies in integrating advanced diagnostic and procedural ultrasound into clinical assessment and management of the undifferentiated patient. Sharing hard fought knowledge with innovative educational techniques to ensure knowledge translation and dissemination is my goal. Family, wild coastlines, native forests, and tinkering in the shed fills the rest of my contented time. | SonoCPD | Ultrasound library | Top 100 | @thesonocave |