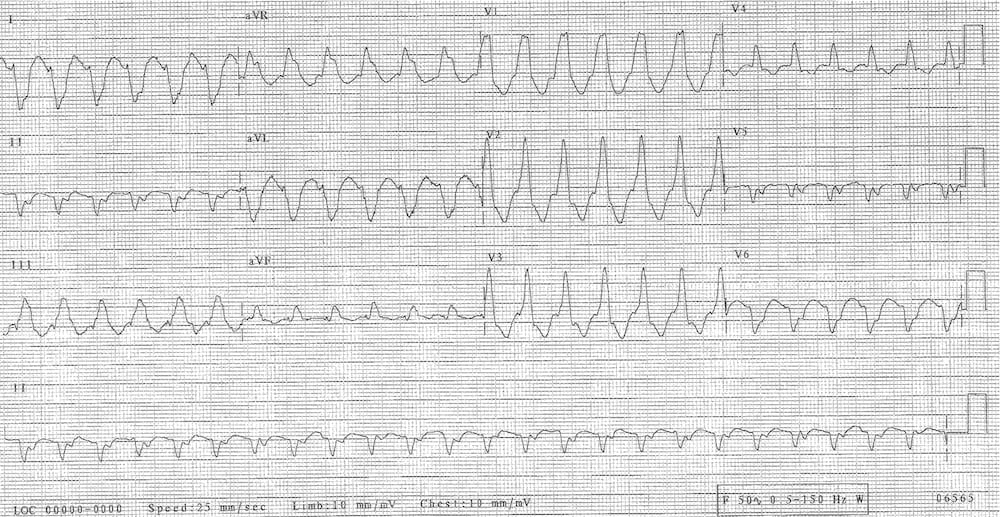
VT or not VT
aka ECG Exigency 013
One fine day, (or was it a midsummer night), in a hospital not far from here, a strange looking patient is brought into the ED. His name is William, but he says “Call me Bill!“. Strangely his last name is Shakespeare. You giggle. What a funny name, you think. So familiar…
Before you can wonder any longer whether this Midsummer Night’s Dream, a Friday night in ED, is about to become a Tempest, the nurse pokes his ECG in front of you.
You feel pretty smart because you have just read up about Super Axis Man (SAM). So you say (insert posh voice here): “Is this an ECG I see before me? The axis towards my hand? Come, let me touch thee. I feel thee not, yet I see thee still.”
You get strange looks from the nurse, so you confidently tell him, “The axis is abnormal — at 130 degrees. Now get thee to a nunnery!”
The nurse, still bewildered about your comments on touching an ECG, and wondering about the method in your madness, says “No! I don’t think the axis is the problem. Look — this ECG is completely abnormal.”
Bah you think — the nurse doth protest too much. But you humor him. “Ah,” you say. “You are correct! The patient has a wide complex tachycardia (WCT). But is it VT?”
Barely conscious, the patient, gasping, looks at you and says…
“VT or not VT? That is the question…”
What is the definition of wide complex tachycadia?
Answer and Interpretation
Wide complex tachycardia has these features:
- The QRS-complex needs to be wide. Wide is >120ms (or >3 small squares).
- The patient needs to be tachycardic, >100/min.
The differential diagnosis in WCT includes ventricular tachycardia (VT), supraventricular tachycardia (SVT) with aberrancy and pacemaker rhythms.
What clinical features help differentiate VT from SVT?
Answer and Interpretation
Although there are no features that reliably distinguish SVT from VT, there are features that make one more or less likely.
History
- If the patient has no prior history of tachycardia, or they have a history of structural cardiac disease, a known pacemaker or ICD this makes VT more likely. A history of AVNRT or other previous SVT makes SVT more likely.
Examination
- The patient who is unstable, has cardiac failure, a midline sternotomy scar, a pacemaker or ICD, cannon a-waves or heart sound fluctuations (esp S1) make VT more likely.
ECG findings
- VT is more common generally (80%, but up to 95% in IHD). VT is more likely with extreme right axis, minor rate variation and chest lead concordance. SVT is more likely with a rate that is exactly 150/min and a narrower QRS-complex width (120-140ms).
Bill looks at you, and whispers longingly:
“O Brugada, Brugada, wherefore art thou Brugada?”
Which algorithms can help differentiate SVT/aberrant conduction from VT?
Answer and Interpretation
There are many different algorithms that may help to distinguish SVT from VT. My favourite ones are the simple four-step ones, either the Vereckei criteria or Brugada criteria. Vereckei criteria were developed as an attempt to simplify the Brugada criteria (specifically step 4) but to retain the test accuracy.
The Vereckei Criteria
The self reported test characteristics were:
- sensitivity: 95.7%
- specificity: 73.4%
- test accuracy: 90%.
These are remarkably similar to the above values for the Brugada Criteria.
Interestingly, in the same paper Vereckei evaluated the same 453 ECGs used to develop his criteria, using Brugada criteria — with a test accuracy of 85%. Furthermore, 18 WCTs were incorrectly diagnosed by both criteria.

Things I like about these criteria…
- They involve a simple four step process.
- Most steps in both the Brugada and Vereckei are simple to remember, and easy to rapidly apply.
Things I don’t like about these criteria…
- Step 4 in the Brugada criteria and step 3 in the Vereckei criteria are complicated.
- VT is a medical emergency. Both criteria get it wrong about 10% of the time…
- 10% is too high for my liking.
So, is all this Vereckei and Brugada business Much Ado About Nothing? Are they Measure For Measure the same thing?
- A more pragmatic way of looking at the algorithm is that yes, both may help you equally in making the diagnosis in a stable patient. But in the unstable patient, the distinction between SVT and VT is academic, because you have a 10% chance of getting it wrong. I think that is too high.
- If someone has a WCT and they are haemodynamically compromised, they need urgent action — a DC shock would be my preference, or a very quick acting antiarrhythmic.
Or, as Bill was saying to me by this stage —
“A shock, a shock, my kingdom for a shock“
References
- Brugada P, Brugada J, Mont L, Smeets J, Andries EW. A new approach to the differential diagnosis of a regular tachycardia with a wide QRS complex. Circulation. 1991 May;83(5):1649-59.
- Vereckei A, Duray G, Szénási G, Altemose GT, Miller JM. Application of a new algorithm in the differential diagnosis of wide QRS complex tachycardia. Eur Heart J. 2007 Mar;28(5):589-600
Further Reading
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog.
- Wiesbauer F. Little Black Book of ECG Secrets. Medmastery PDF
- Hampton, JR. The ECG In Practice, 6e
- Mattu A, Brady W. ECG’s for the Emergency Physician 1
- Mattu A, Brady W. ECGs for the Emergency Physician 2
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric, 6e
- Wagner, GS. Marriott’s Practical Electrocardiography 12e
CLINICAL CASES
ECG EXIGENCY
Specialist Intensive Care Physician working at the Austin Hospital, Melbourne. Interests: Shoulder Dislocations, Pain Management, End-of-life care, Organ Donation and ECGs | Linkedin |


But, is this VT or not?