Watery Diarrhoea
aka Tropical Travel Trouble 006
Our medical student who caught shigella on a Nepalese elective has a thirst for adventure. They plan to help at a Bangladesh refugee camp but the latest CDC report states there have been some cases of cholera. They’ve done a little bit of reading and want your help to teach them all about cholera and how they may prepare and best serve their new community.
Q1. What is cholera and how is it transmitted?
Answer and interpretation
Cholera is a gram-negative comma-shaped bacillus. Sero groups 01 and 0139 cause clinical disease.
Humans are the only animal host. Arguably it is present in some shellfish and plankton but the main transmission is contaminated food/water from infected faeces.
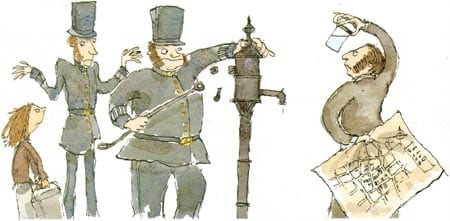
John Snow from epidemiological fame (not Game of Thrones) challenged the theory that cholera was in the air and due to “miasma“, he thought it was a contaminant in water. When cholera returned to London in 1853, Snow recognised an ideal opportunity to test his hypothesis by comparing cholera mortality rates in populations of south London supplied by water drawn from sewage-contaminated versus uncontaminated regions of the Thames.
On 30 August 1854 while involved in these studies, a dramatic cholera epidemic began near his home in Soho leading to more than 550 deaths within two weeks. Analysis of the addresses of the cholera deaths and interviews of residents of the area led him to suspect that water from a pump on Broad Street was responsible – and he prevailed upon the local council to remove the handle of the pump on 8 September 1854.
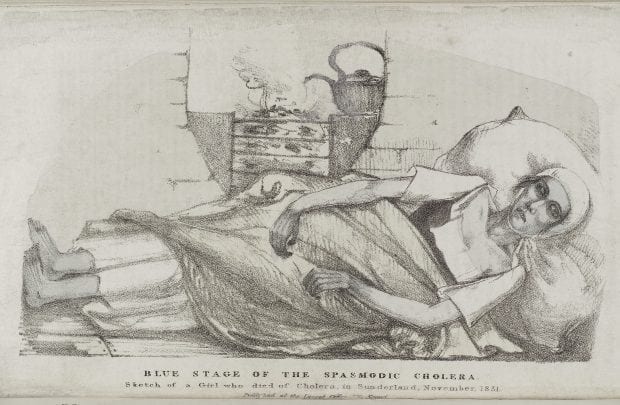
In somewhat of a loose connection to Jon Snow in Game of Thrones you can see from the image below that in the late stages of cholera, patients develop cyanosis, a bit like a white walker!
Q2. How much V. cholerae do you need to consume to develop infection?
Answer and interpretation
The infectious dose of V. cholerae is relatively high; an inoculum of 108 V. cholerae or higher generally results in severe infection in healthy North American volunteers. [Reference]
Q3. Why does Cholera typically cause a painless watery diarrhoea?
Answer and interpretation
- V. cholerae forms colonies of bacteria on the surface of the small intestine.
- Organisms attached to the small intestine produce cholera toxin (CT), which then undergoes endocytosis and travels to the endoplasmic reticulum through pathways to eventually increase concentrations of intracellular cyclic AMP
- Increased cAMP results in secretion of chloride via apical cystic fibrosis transmembrane conductance regulator (CFTR) channels and inhibition of sodium chloride absorption.
- The ultimate result is large amounts of sodium, chloride, bicarbonate and potassium in the small intestinal lumen which results in large fluid shifts.
Q4. What is the incubation time and how soon could you die from cholera once symptoms develop?
Answer and interpretation
- On average 1-2 days but depending on the amount ingested it can range from just a few hours to 5 days.
- Once symptoms develop, death can occur within 12 hours although there are multiple case reports of people dying within 4 hours with profound fluid shift into dilated bowel loops without the classic features of cholera (Cholera sicca).
- Untreated, cholera kills 50% but with correct treatment the mortality is less than 1%.
Q5. What risk factors are there for contracting cholera and what might be protective?
Answer and interpretation
Risk factors:
- Blood group O (associated with more severe cholera).
- Hypochlorhydria (lowers the dose needed to cause infection).
- Retinol deficiency.
Protective:
- Previous infection (bowel immunity).
- Breastfeeding has been consistently shown to be protective against cholera.
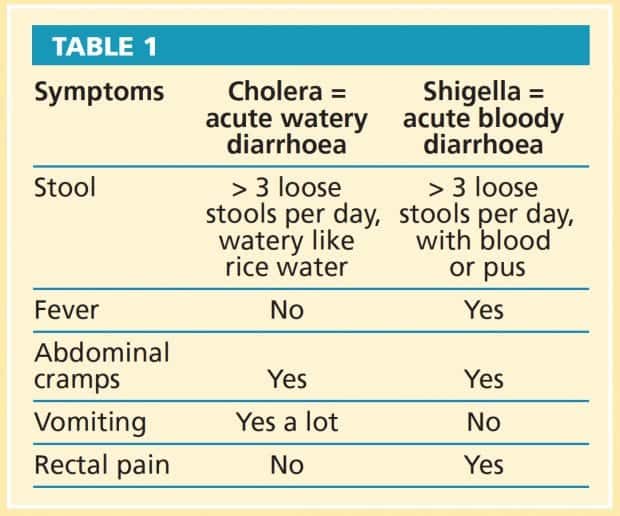
Q6. What are the classic symptoms I should be looking for?
Answer and interpretation
Classic symptoms:
- Abdominal discomfort and borborygmi.
- Vomiting (typically watery).
- Profuse diarrhoea: typically “rice-water” stool, with a fishy odor. The diarrhoea is usually painless, without tenesmus. In adults, stool output can reach as high as 1 liter per hour and in children, 10 and 20 ml/kg/hour. This rate of fluid loss is not typically observed in other causes of diarrhoeal illness.
- Fever is uncommon.
Q7. If I have someone with rice water stool is that enough to make the diagnosis? What about if you were in the UK or Australia, how would you make the diagnosis?
Answer and interpretation
Most cases of cholera are presumptively diagnosed based on clinical suspicion.
This is typical in resource-poor settings and due to the high mortality if left untreated (0.5% if treated), management if often started empirically. Although the following differentials produce watery diarrhoea, it is less profuse than cholera:
- Rotavirus and cryptosporidium among infants and young children.
- Escherichia coli predominates among older children and adults.
Cholera can be presumed on clinical grounds via the following definitions:
- MSF: any patient developing rapid onset severe watery diarrhoea (usually with vomiting), resulting in severe dehydration.
- WHO:
- (a) in area in which cholera is not known to be present, patient > 5yr develops severe dehydration or dies from acute watery diarrhoea;
- (b) area in which there is a cholera outbreak, any patient > 5yr who develops acute watery diarrhoea, with or without vomiting.
Stool culture (gold standard, done on thiosulfate citrate bile sucrose agar or taurocholate tellurite gelatin agar) should be performed if an outbreak is suspected to assist with diagnosis and antibiotic sensitivities.
Transport the specimen in Cary-Blair media or alkaline peptone water to a central laboratory from field settings. If suspecting cholera it is best to inform the laboratory so they can place the stool on specific media.
The vibes can be seen darting on dark field microscopy and the movement can be inhibited by using various antisera (antibodies) to help confirm the serotype.
Rapid tests may be performed to make a presumptive diagnosis of cholera.These include commercially available immunochromatographic lateral flow devices (dipsticks), the sensitivity of which can be over 95 percent, but the specificity of the test has ranged between 65 to 85 percent in field settings. The low specificity of dipstick tests can limit their diagnostic utility in endemic areas, but a preponderance of positive tests in a small cohort of patients with diarrhoea (3 out of 10) is useful in confirming a suspected outbreak. Any suspected cholera specimen screened by the rapid test should be confirmed by lab culture.
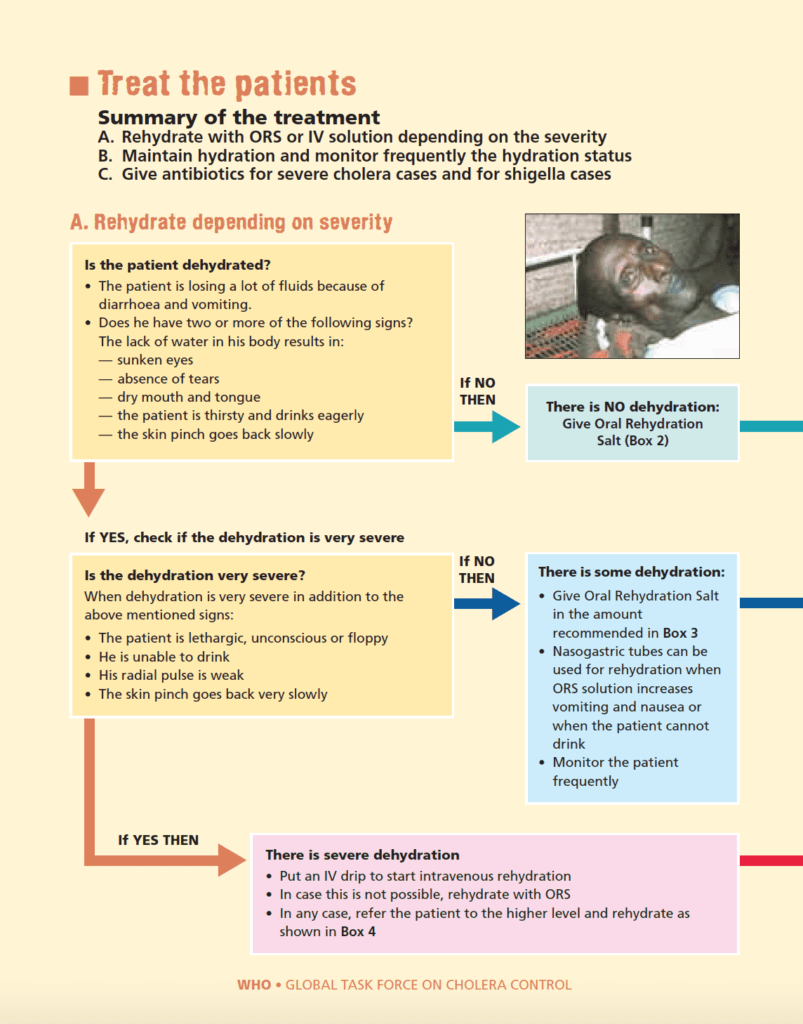
Q8. What is the empiric management?
Answer and interpretation
Fluids, fluids and fluids.
Probably one of the few diseases in which giving a patient 4L in one hour would not be considered negligent. Titrate fluids closely to your patient’s response, where possible convert to oral once initial resuscitation is completed.
The antibiotic options for cholera include macrolides, fluoroquinolones and tetracyclines. The choice between them should be based on availability and local resistance patterns.
- Tetracyclines (doxycycline) are the antibiotic class for which there is greatest clinical experience. However, resistance to tetracycline is common, so empiric use of these agents should be limited to outbreak settings in which the causative isolate has documented susceptibility. They should also be avoided in pregnancy and lactation.
- Fluoroquinolones and macrolides are reasonable alternative agents, although resistance to fluoroquinolones is also growing in endemic areas.
- Fluoroquinolones at varying doses, including a single dose, have had at least comparable efficacy as tetracyclines against both V. cholerae O1 and O139 in several trials (ciprofloxacin 1g as a stat dose).
- Macrolides are also effective in adults and children. In a trial of 128 children with cholera, erythromycin (12.5mg/kg every six hours for three days) and azithromycin (20mg/kg single dose) had similar clinical and bacteriologic efficacy, although azithromycin was associated with less vomiting.
WHO management guidelines for interest:
Q9. How do you make ORS?
Answer and interpretation
- 1L of water, 2.6 g sodium chloride, 2.9 g trisodium citrate, 1.5 g potassium chloride and 13.5 g glucose. Usually it is provided in ready made sachets, if not you can make it with:
- 1L of water, 1/2 teaspoon of salt and 6 teaspoons of sugar.
- ORS was first used on a large scale in a cholera epidemic in the 1970’s, see FFFF 213 Q3 for more details.
Q10. How would you manage an outbreak?
Answer and interpretation
Preparedness: see WHO cholera kits and stock lists to manage an outbreak. It includes an excel calculator to make an estimate of patients, IV fluids and antibiotics required.
Interrupt transmission:
- Drink and use safe water. Bottled water, boiled or chlorinated water. If chlorine is not available then add 8 drops of household bleach for every 1 gallon of water (2 drops for every 1 litre) and wait 30 minutes before drinking.
- Wash hands with safe water and soap.
- Use latrines to bury faeces, avoid contamination with water.
- Cook the food well. Fruit and veg must be washed in safe water and peeled.
- Washing must be done at least 30 meters away from drinking water sources.
- Vaccination is controversial. The WHO currently does not recommend vaccination in an outbreak as dosing is usually 7 days apart and is therefore potentially impractical. Aid workers coming to an outbreak should ideally be vaccinated and at risk populations that are on the periphery of your outbreak should also be considered for vaccination. Two internationally-licensed oral cholera vaccines are available, administered as two or three doses depending on age. See our vaccination page.
Control and management of cases and contacts: isolate cholera patients, use cholera cots, clean and use separate latrines, clear all infected materials in chlorine. Wash hands.
Surveillance and reporting: You will be in a privileged position to report what is clinically happening on the ground. Efficient reporting allows organisations to monitor and plan for the provisions you may require on the ground, and also help you visualise whether you are controlling the outbreak.
Corpse management:
- Disinfect corpses with chlorine solution (2%).
- Fill mouth and anus with cotton wool soaked with chlorine solution.
- Wash hands with soap after touching the corpse.
- Disinfect the clothing and bedding of the deceased by stirring them in boiling water or by drying them thoroughly in the sun.
References
- Beeching N and Gill G. Lecture Notes – Tropical Medicine. 7e Wiley Blackwell 2014.
- CDC – cholera prevention
- Eddleston, Davidson, Brent, Wilkinson. Oxford Handbook of Tropical Medicine. Oxford Medical Handbooks. 4e 2014
- Green Book – Cholera
- Matthews PC. Tropical Medicine Notebook. Oxford University Press, 2017
- Rothe C. Clinical Cases in Tropical Medicine. Elsevier 2015. ISBN 9780702058240
- Uptodate – Cholera
- WHO – Cholera kit education module
- WHO – First steps on managing a diarrhoea outbreak
CLINICAL CASES
Tropical Travel Trouble
Dr Neil Long BMBS FACEM FRCEM FRCPC. Emergency Physician at Kelowna hospital, British Columbia. Loves the misery of alpine climbing and working in austere environments (namely tertiary trauma centres). Supporter of FOAMed, lifelong education and trying to find that elusive peak performance.