Weil disease
Description
Weil disease refers to the severe icteric form of Leptospirosis. Bacterial infection with worldwide distribution. Multiple Leptospira serotypes know, including L. icterohaemorrhagica, L. interrogans, L. pomina, L. canicola, and L. automnalis.
Human infection secondary to contact with fresh water, wet soil or vegetation contaminated by the urine of infected animals, especially rodents (for example rats and mice) but also skunks, foxes, cattle and dogs. Bacteria enters body through broken skin, water-softened skin, mucous membranes or by or by swallowing/inhaling contaminated water.
Leptospirosis is typically biphasic, with long incubation period 10 days (2-26 days). Severe illness (Weil disease) typically occurs in the second phase of the disease.
Phase 1 – The Septicaemic or Leptospiraemic phase.
- Timing: 5-7 days
- Features: Bacteria found in blood and CSF of patients.
- Symptoms: Fever, vomiting, diarrhoea, myalgia, and headache. Symptoms are often mild and can represent influenza. Patients are typically anicteric. It is believed that many cases of mild leptospirosis are undiagnosed.
Phase 2 – The Immune phase.
- Timing: 7-14 days later
- Features: IgM antibodies produced. Spirochetes excreted in urine.
- Symptoms: Characterized by conjunctival congestion, jaundice, fever, renal failure, hepatosplenomegaly, and haemorrhagic purpura/petechiae. Any organ system can be affected.
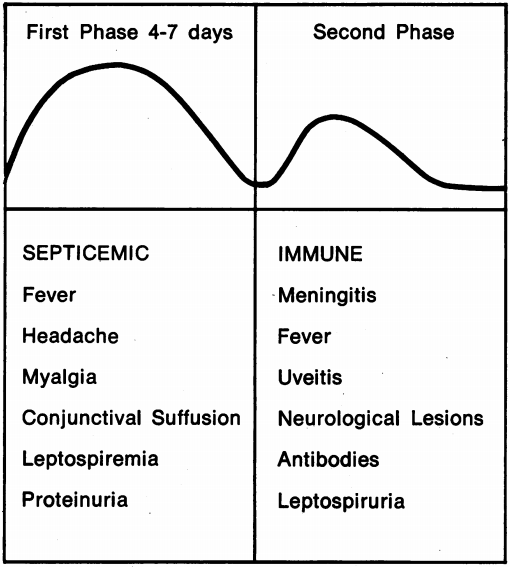
It is worth noting that it is common for there to be an asymptomatic phase 1-3 days after symptoms start, before a later recurrence of symptoms. This was also noted by Weil’s in his original paper.
History of Weil disease
Multiple recorded outbreaks of infectious jaundice (most probably severe icteric Leptospirosis) prior to it’s first medical publication in 1886.
1883 – Early description by Louis Landouzy (1845 – 1917) as Typhus hépatique
Je constatai également une fièvre très vive, une dyspnée intense, une teinte sale, ictérique, de la peau et des conjonctives; les urines contenaient de l’albumine ainsi qu’une,certaine quantité de bile…Le foie était un peu augmenté de volume, il était douloureux à la pression…La température centrale, le matin, de 38°.8. En un mot, il présentait les signes d’une adultération de la plèvre et du poumon, soit une pleuro-broncho-pneumpnie droite, ainsi que de la congestion du foie.
Landouzy L. Typhus hépatique. Gazette des hôpitaux civils et militaires, 1883; 56: 913-914
I also noticed a very high fever, intense dyspnea, a dirty tinge, jaundice, of the skin and conjunctiva; the urine contained albumin as well as some bile…The liver was slightly enlarged, it was painful to pressure…The core temperature, in the morning, 38.8. In short, he presented the signs of an adulteration of the pleura and lung, i.e. a right bronchopneumonia, as well as congestion of the liver.
Landouzy L. Typhus hépatique. Gazette des hôpitaux civils et militaires, 1883; 56: 913-914
1886 – Adolf Weil (1848-1916) published an ‘acute infectious disease with enlargement of spleen, jaundice, and nephritis‘. In this, Weil observed two patients in 1882 that presented to his clinic presenting with near identical symptoms to two patients he had observed earlier in 1870.
Die 4 bescbriebenen Fälle bieten so viel Uebereinstimmendes, dass sie wohl gemeinsam besprochen werden können. In allen vier Fällen handelte es sich am acut fieberhafte, mit schweren nervösen Erscheinungen, ausserdem mit Schwellung der Milz und Leber, Jcterus, nephritischen Symptomen einhergehende Erkrankungen, die aber nach verhältnissmässig kurzer Dauer des schweren Krankheitsbildes einen raschen gflnstigen Verlauf nahmen.
Weil A. Ueber einer eigenhuemliche, mit Milztumor, Icterus un Nephritis einhergehende, acute Infektionskrankheit. Deutsches Archiv für klinische Medizin. 1886; 39: 209-232
The four cases described offer so much in common that that they can probably be discussed together. In all four cases were acute fevers, with severe nervous symptoms, also with swelling of the spleen and liver, icterus, diseases associated with nephritic symptoms, but which, after a relatively short duration of the severe clinical picture, took a rapid and favorable course.
Weil A. Ueber einer eigenhuemliche, mit Milztumor, Icterus un Nephritis einhergehende, acute Infektionskrankheit. Deutsches Archiv für klinische Medizin. 1886; 39: 209-232
Weil carefully documented the timing and symptoms of all four patient’s, documenting the similarities and considering possible diagnoses.
Weil decided on clinical grounds that these cases represented a new entity.
1886 – In the same year Albert Mathieu published a similar condition as Typhus hépatique benin; rechute, guérison [Benign Liver Typhus; relapse, healing]
1907 – First identification of Leptospira by Arthur Stimson, whilst working on yellow fever, in post-mortem kidney specimens. Originally named Spirochaeta interrogans. No link was made at this time between Leptospira and Weil’s disease.
I would suggest that the organism be called Spirochaeta interrogans, the specific name being suggested by the form, somewhat resembling a question mark, which the organism frequently assumed in my preparations.
Stimson AM. Note on an organism found in yellow-fever tissue. Public Health Reports. 1907; 22(18): 541.
1913 – Inada and Ido showed for the first time that inoculation of a guinea pig with blood of a patient known to be infected with Weil’s disease, produced symptoms reminiscent of Weil’s disease in the guinea pig.
1914 – Inada and Ido detected spirochetes in liver tissue of a guinea pig injected with the blood of a patient suffering from Weil’s disease.
1915 – Based on the above finding, and the finding of spirochetes in the blood of patient’s with Weil’s disease, Inada and Ido were able to conclude that Spirochetes are the causative agent of Weil’s disease. The causative agent was originally named “spirochaeta icterohaemorrhagiae japonica”, although the “japonica” was later dropped following the finding of Weil’s disease in patients in Europe.
We came to the conclusion, in January, 1915, that this spirocheta is the pathogenic cause of Weil’s disease, and we named it Spirocheta icterohaemorrhagiae
Inada R et al. J Exp Med. 1916

Inada 1916, Plate 56 Fig 1-4

Inada 1916, Plate 57 Fig 11
1915 – Two german groups published independent discoveries of Leptospira as the causative agent. These works were published after Inada and Ido’s discoveries.
Hübener and Reiter: (published in 1915)
Our investigations extend beyond the eight patients which we have reported and in which our transmission experiments produced positive results. Weil’s disease is an acute, noncontagious, infectious disease whose causative agent belongs to the group of spirochaetae which can be transmitted to man through the bite of insects. Introduced into the blood stream, the spirochete affects internal organs and tissues simultaneously and produces specific toxic substances which cause systemic disease with typical fever and with predilection for the kidneys and the liver.
[Hübener, Reiter 1916]
Associated Persons
- Louis Landouzy (1845 – 1917)
- Adolf Weil (1848 – 1916)
- Albert Mathieu (1855 – 1917)
- Louis Théophile Joseph Landouzy (1845 – 1917)
- Hans Reiter (1881 – 1969)
- Ryukichi Inada (1874-1950)
Alternative names
- Infectious jaundice; Infectious icterus
- Mathieu disease, Mathieu’s disease (France)
Infection with Leptospirosis also termed:
- Pseudo-dengue of Java; seven-day fever, autumn fever, Akiyama disease; marsh/swamp fever; 7-day fever; black jaundice; harvest fever; canefield fever; rat catcher’s yellows; Fort Bragg fever; pretibial fever [QJM 2012]
References
Historical references
- Landouzy L. Typhus hépatique. Gazette des hôpitaux civils et militaires, 1883; 56: 913-914
- Mathieu A. Typhus hépatique benin; rechute, guérison. Revue de médecine. 1886; 6: 633-639.
- Weil A. Ueber einer eigenhuemliche, mit Milztumor, Icterus un Nephritis einhergehende, acute Infektionskrankheit. Deutsches Archiv für klinische Medizin. 1886; 39: 209-232
- Stimson AM. Note on an organism found in yellow-fever tissue. Public Health Reports. 1907; 22(18): 541.
- Uhlenhuth P, Fromme W. Experimentelle Untersuchungen über die sogenannte Weilsche Krankheit (ansteckende Gelbsucht). Medizinische Klinik 1915; 11(44): 1202–1203
- Inada R, Ito Y. A report of the discovery of the causal organism (a new species of spirocheta) of Weil’s disease. Tokyo Ijishinshi. 1915: 351-360.
- Hübener, Reiter H. Beiträge zur Aetiologie der Weilschen Krankheit. I. Deutsche Medizinische Wochenschrift. 1915; 41(43): 1275-1277
- Hübener, Reiter H. Beiträge zur Aetiologie der Weilschen Krankheit. II. Deutsche Medizinische Wochenschrift. 1916; 42(1): 1-2
- Hübener, Reiter H. Zur Aetiologie der Weilschen Krankheit. III. Deutsche Medizinische Wochenschrift. 1916; 42(5): 131-133
- Reiter H. Beiträge zur Aetiologie der Weilschen Krankheit. IV. Deutsche Medizinische Wochenschrift. 1916; 42(42): 1282-1284
- Inada R, Ido Y, Hoke R, Kaneko R, Ito H. The etiology, mode of infection and specific therapy of Weil’s disease. The Journal of Experimental Medicine. 1916; 23(3): 377–402
Review references
- Alston JM, Brown HC. The Epidemiology of Weil’s Disease: (Section of Epidemiology and State Medicine). Proc R Soc Med. 1937; 30(6): 741-756.
- Edwards GA, Domm BM. Human leptospirosis. Medicine (Baltimore). 1960; 39: 117-156.
- Lawrence S. Leptospirosis. West J Med. 1980; 132(5): 440-450.
- Kobayashi Y. Discovery of the causative organism of Weil’s disease: historical view. J Infect Chemother. 2001; 7(1): 10-15
- Forbes AE, Zochowski WJ, Dubrey SW, Sivaprakasam V. Leptospirosis and Weil’s disease in the UK. QJM 2012; 105(12): 1151–1162
- Nickson C. Leptospirosis. LITFL CCC
eponymictionary
the names behind the name
Studied Physiological Sciences BA (Hons), followed by Medicine at the University of Oxford BM BCh. British doctor currently working in emergency medicine in Perth, Australia. Special interests include acute internal medicine and emergency medicine.

