Weingart on Pelvic Trauma
LITFL turns to EMCrit’s Scott Weingart for his take on the approach to the hemodynamically unstable pelvic trauma patient.
- Is FAST negative enough? Or do we need to do a diagnostic peritoneal aspirate (DPA) to rule out an intra-abdominal injury?
- Where to next to stem the flow of pelvic blood? The OR or the angiography suite?
Let’s hear what Scott has to say (5 min 35 sec):
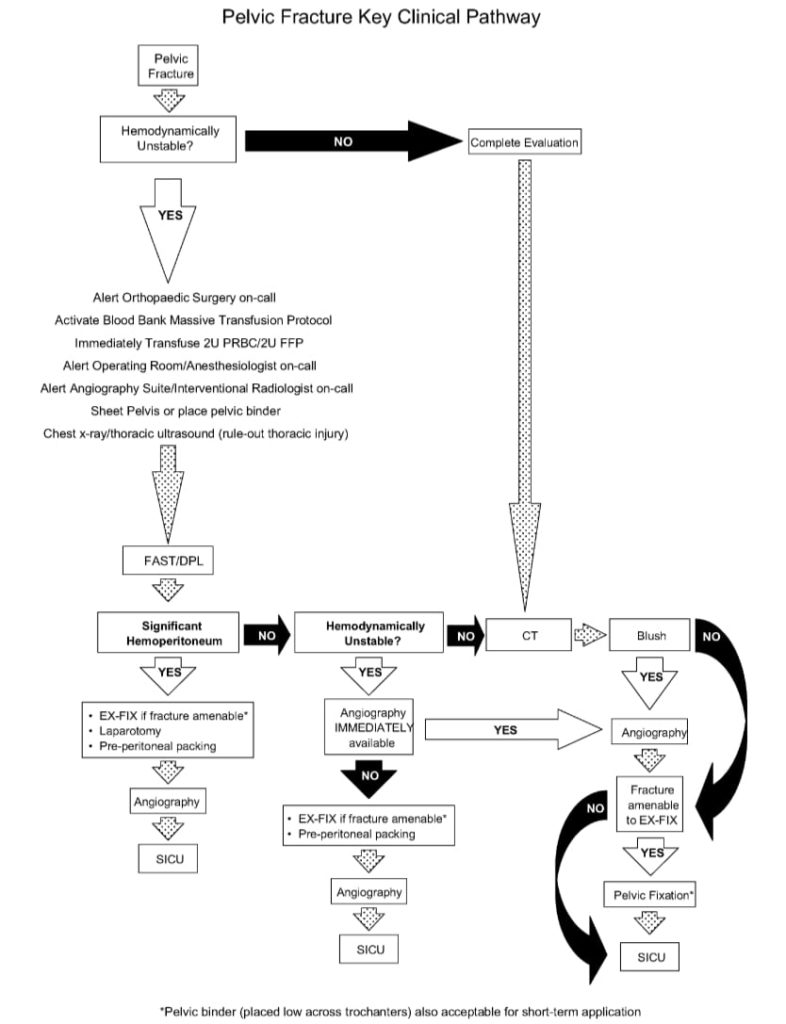
Here is a suggested pathway for the approach to the major trauma patient with pelvic fractures from White et al (2009):
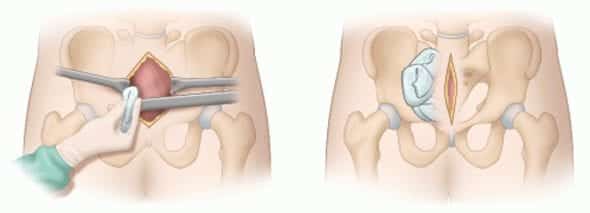
Preperitoneal packing: “Preperitoneal pelvic packing (PPP) is performed through a 6 to 8 cm midline incision made from the pubic symphysis cephalad, with division of the midline fascia. The pelvic hematoma often disscts the preperitoneal and paravesical space down to the presacral region, facilitating PPP; alternatively, blunt digital dissection opens the preperitoneal space for packing. Three standard surgical laparotomy pads are placed on each side of the bladder, deep within the preperitoneal space, and the fascia is closed with O-PDS suture and the skin with staples.”
Finally, here is Scott’s summary of the recommendations from the 2011 EAST guidelines for hemorrhage in pelvic fracture from crashingpatient.com:
- external fixation doesn’t limit blood loss, but reduces fracture displacement (III)
- unstable patients should get angio (I)
- pts with blush may require angio even if stable (I)
- ongoing bleeding after angio should get repeat angio (II)
- >60 y/o with major fracture should get angio even if stable (II)
- anterior fractures assoc with ant vessel injury and posterior = posterior (III)
- Bilateral non-selective angiographic embolisation is safe, gluteal ischemia is more likely from injury not angio (III)
- … And doesn’t affect male potency (III)
- FAST is insensitive in pelvic trauma (I) – Scott doesn’t agree with this one!
- … but FAST has adequate specificity (I)
- DPA is test of choice (II)
- Use CT if stable (II)
- Fracture pattern doesn’t predict need for angio (II)
- Nor hematoma location (II)
- Absence of ICE doesn’t exclude active hemorrhage (II)
- Volume > 500 cm3 predicts need for angio (III)
- Isolated acetabular fx may still need angio (III)
- Perform cystogram after ct (III)
- Binders reduce fx as well as definitive stabilization and decrease pelvic volume (III)
- And they limit hemorrhage (III)
- They work as well or better than external fixation in controlling hemorrhage (III)
- RetroP can be used to salvage after failed angio (III)
- Can be used as primary in an integrated protocol (III)
References and further learning
Journal articles
- Cullinane DC, Schiller HJ, Zielinski MD, Bilaniuk JW, Collier BR, Como J, Holevar M, Sabater EA, Sems SA, Vassy WM, Wynne JL. Eastern Association for the Surgery of Trauma practice management guidelines for hemorrhage in pelvic fracture–update and systematic review. J Trauma. 2011 Dec;71(6):1850-68. Review. PubMed PMID: 22182895.
- Suzuki T, Smith WR, Moore EE. Pelvic packing or angiography: competitive or complementary? Injury. 2009 Apr;40(4):343-53. Epub 2009 Mar 17. Review. PubMed PMID: 19278678.
- White CE, Hsu JR, Holcomb JB. Haemodynamically unstable pelvic fractures. Injury. 2009 Oct;40(10):1023-30. Epub 2009 Apr 16. Review. PubMed PMID: 19371871.
Social media and other web resources
- EMCrit — Severe Pelvic Trauma
- The Trauma Professional’s blog — Bleeding and pelvic trauma
- The Trauma Professional’s blog — Compression of pelvic fractures with a sheet
- Western Trauma Association — Pelvic Trauma Algorithm
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC