What Weingart would do II
aka Trauma Tribulation 033
Pull the knife or don’t pull the knife?
Thank you for all your responses. Here is the followup post to Trauma Tribulation 32.
First of all a quick recap: 16 year old male, multiple stab wounds to his back, knife still in-situ. Obs stable BUT he is 90 minutes from the nearest trauma centre. You have no other docs to help you. The only things you have is a CXR. 2 units of O-neg blood and basic labs…
How do you manage this tricky situation?
We asked Scott Weingart (from EMCrit.org) to look at the scenario and tell us what he would do. It was a bit mean of us, as as we drip-fed the information in the previous post, so we gave him right of reply after seeing the story unfold.
What would Weingart do?
Well you folks will hear my reply based only on the original case shortly. Gerard has supplied all sorts of juicy tidbits in these comments that I didn’t hear until now, so some thoughts.
Retrieval in your neck of the woods is very different than in the States. You folks get trained docs with a bevy of interventions at their disposal, so I would leave the knife in situ. What do I gain by yanking it in a stable patient? If need be, pull it if the patient decompensates in the air. If Minh tells me he wants the airway controlled before the pt flies, then let’s do that in the ED as a team. Lateral intubation is not hard you just turn your body to match the patient’s orientation. Minh will probably show up with video which makes it even easier. If you fail your first pass and the pt’s sats are not being maintained, pull the blade, put him on his back, re-oxygenate and intubate normally.
If you folks did decide to pull the knife, put the chest tube in first, just as they did.
Thoractomy will be something of a shitshow in this case. You would definitely want to do it as the BP is going way south but before arrest. Clamshell is not doing you any favors, this is a posterior wound and your visibility is going to be poor with the patient supine. Probably better off going in with the patient propped up on some sheets, extend the L incision toward posterior and pray it is an intercostal that you can put pressure on with some sponges at both ends of the cut vessel, while your nurse pours in whatever blood and products this center has and hope the BP recovers. If it does, then some poor soul is going to sit there holding pressure until you can fly in a surgeon.
If it is not an intercostal, then it is lung. If you know how to find the inferior pulmonary ligament and cut it, then you can clamp the hilum or do a pulmonary twist. Both of these maneuvers are hard and the pt will prob die before definitive management can get there.
Every ED doc should know how to perform a thoracotomy with the sole goal of opening pericardium and putting a finger on a hole. This can be life saving anywhere regardless of the time for surgeons to arrive and is well within the skillset of the specialty. If you can’t do this, come to SMACC and I will take you through it.
…and here is his initial response via podcast (2 min 52 sec) – recorded prior to the first post going live:
We would like to thank Scott for those comments, and for agreeing to be put on the spot. He made some great points, and his approach to this situation makes a lot of sense. And thanks to all our readers for their contributions and debate.
Lets play the scenario out, and see what happens…
Q1. What things about this situation are concerning?
Answer and interpretation
This patient has several problems that are immediately apparent, and several more potential problems.
- He is prone.
- The knife is still in, and the handle has broken off.
- The knife is angled towards the midline – isn’t the IVC around there somewhere?
- There are 4 other puncture wounds lower down bilaterally on his back.
- He doesn’t have IV access yet!
Ok. In this situation one might feel a wee bit annoyed. No one said he was prone, no one said the knife was still in his back, and no one said that YOU ARE THE ONLY DOC in the hospital!
Q2. What are your immediate priorities?
Answer and interpretation
As per any trauma scenario, follow the ATLS mantra.
- A – airway
- B – breathing
- C – circulation
Whilst the MICA paramedic gained IV access, you assess his airway. He’s talking, mainly swear words, but he’s conspicuously vague about who the perpertrator was. This is a good sign. Vitals: Sats 99% (non-rebreather), RR 20, SBP 130, PR 100.
You are feeling a little better about things. However you are anxious to get him supine, but you can’t with that knife still in his back!
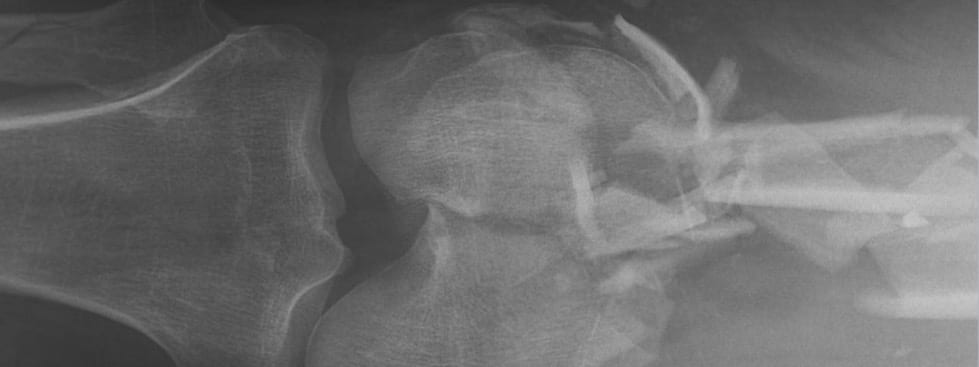
The CXR shows the following:
- The knife is within the hemithorax
- It does not appear to involve the IVC
- There is a small pneumothorax
- There is no evidence of haemothorax
At this point, you place an intercostal tube on the right side. Although the landmarks are difficult on a prone patient, a conveniently positioned piercing helps guide you. Once connected to the underwater sealed drain, it bubbles and there is no blood in the chamber. The patients’ vitals remain stable.
Q3. But what do you do now? Do you pull the knife?
Answer and interpretation
Arguments FOR pulling the knife:
- To get him supine and hence much easier to control the airway should he deteriorate.
- The knife is not likely to be in a major vessel.
- Removing the knife is unlikely cause more damage than has already been done.
- He needs to be transported to a major centre: which will involve a helicopter or road ambulance. This would be easiest with the patient supine.
Arguments AGAINST pulling the knife:
- The knife MAY may be tamponading a vessel (e.g IVC or intercostal) and there are no surgeons available to do a thoracotomy.
- He is stable and does not currently need to be supine for any medical reason.
- You have limited blood available.
Q4. So – what happened?
Answer and interpretation
Lots of things are going through your mind…
- You need to get him supine, but can’t do this with the knife still in situ.
- You wonder whether he actually needs to go supine to get him to another hospital?
- You wonder whether by removing the blade you will cause a potentially life threatening bleed?
Times like this it is easy to feel confused, alone, and quite a bit scared.
One approach is to think like a surgeon and start spreading the blame… sorry, anxiety. So, you call the nearest retrieval service – and speak to the retrieval physician. They arrange to send a helicopter out. By your description of the knife, the patient and the CXR, the physician is pretty happy that the knife is not in the IVC, so he tells you to pull the knife (out the same way it went in), and get him supine.
His argument is that they will transport him supine, and the knife needs to be out for that. By pulling the knife, he has a chance to prove stability or otherwise, which can be dealt with easier on the ground (in the ED) than in the air. They are also bringing 6 units of O-negative blood.
So, you pull the knife…
When the retrieval team arrives, the patient is supine and comfortable thanks to the morphine. His vitals remained stable and he is transferred to a major centre.
As he leaves, you regret not counting his teeth — maybe you would have felt better about pulling the knife if you knew what his tattoo-to-tooth ratio was …
Oh well.
CLINICAL CASES
Trauma Tribulation
Specialist Intensive Care Physician working at the Austin Hospital, Melbourne. Interests: Shoulder Dislocations, Pain Management, End-of-life care, Organ Donation and ECGs | Linkedin |

