Trauma! Initial Assessment and Management
aka Trauma Tribulation 014
Your trauma patient from Trauma Tribulation 013 has arrived… A trauma call was activated and the team assembled. The patient was transferred onto a bed in the trauma bay, and removed from a spinal board used fro transfer. Handover and vital signs are being obtained as the trauma team get to work.
As the Trauma Team Leader, you’re going to need to know your stuff to be able to coordinate the team’s initial assessment and management of this trauma patient.
Questions
Q1. What are the 5 key components of the primary survey in major trauma?
Answer and interpretation
ATLS (8th edition) emphasizes the ABCDE approach:
- Airway maintenance with cervical spine protection
- Breathing and ventilation
- Circulation with hemorrhage control
- Disability (neurological status)
- Exposure and environmental control (completely undress the patient but avoid hypothermia)
This assessment can usually be performed in less than 10 seconds.
Handy tips:
- Talk to the patient. Any verbal response strongly suggests that for the moment at least their ABCDE’s are okay!
- Once identified, deal with a problem BEFORE moving on in your assessment (this is encapsulated by the mantra “FIND the bleeding, STOP the bleeding”).
- After any intervention, return to the start of the primary survey.
Q2. What does airway maintenance with cervical spine control involve?
Answer and interpretation
Airway assessment and maintenance:
- Ensure patency and consider if airway protection is required.
- Escalate from simple to advanced techniques as required.
- Suction and Magill’s forceps should be immediately available.
- Employ simple airway maneuvers – jaw thrust and chin lift. Head tilt inappropriate with cervical spine control.
- Use airway adjuncts – oropharyngeal airway usually only a temporizing measure if tolerated as usually requires definitive airway. Nasopharyngeal airways are inappropriate in head and facial trauma due to risk of intracranial passage.
Consider the need for a definitive airway, which may be required for A, B C or D reasons:
- A – eg: impending airway obstruction (burns, penetrating or blunt neck injury) or injury that may distort airway anatomy (e.g. neck hematoma)
- B – eg: Respiratory insufficiency due to a large pulmonary contusion, flail chest, or other thoracic injury.
- C – eg: multisystem trauma with shock
- D – eg: Reduced GCS (especially <8), penetrating cranial vault injury
Intubation may also be advisable prior to invasive procedures (e.g. chest tube insertion) or patient transfer.
All ED intubations should be regarded as difficult airways and every operator should have a ‘plan B’ prior to commencing. Surgical airways (e.g. cricothyrotmy) are required in the ‘can’t intubate, can’t ventilate scenario’. Patients that require urgent, but not emergent intubation (e.g. facial burns) may be best intubated by awake fiberoptic intubation with anesthesia and ENT in attendance.To learn more about airway management, check out the videos at Own the Airway!
Major trauma patients should be suspected of having cervical spine injuries. Until the cervical spine is cleared, spinal precautions should be employed.
- Control cervical spine with a hard collar, sandbags and tape
- Easy access to airway may mandate manual cervical spine immobilization by a third party until airway control is achieved
Appropriate cervical spine precautions is an evolving area of controversy…
- Resus.ME — Another reason to be skeptical about collars
- Resus.ME — Cervical spine guideline
- Resus.ME — Neck movement in spite of collar
Q3. What does assessment and management of breathing and ventilation involve?
Answer and interpretation
Assessment
- Respiratory rate and SpO2
- Exposure and inspection essential: external signs of trauma, asymmetrical chest movements
- Careful palpation over entire chest wall may reveal unsuspected injury e.g. crepitus / surgical emphysema.
- Percussion – often difficult in a noisy trauma bay
- Auscultation – listening for air entry bilaterally, gauge adequacy and assess for added sounds
- Trachea – palpate to see if deviated, although true tracheal deviation due to a tension pneumothorax is pre-terminal and it is unlikely to be the only sign
- May be appropriate to log roll at this stage if concerned about a posterior chest injury.
Management
- High flow oxygen 15L/min via non-rebreather mask on arrival
- Non-invasive ventilation is rarely indicated in trauma patients
- Patients requiring respiratory support are usually intubated and mechanically ventilated
- Needle thoracotomy, finger thoracotomy or intercostal catheter insertion may be required urgently
Handy tip
- Be prepared for a tension pneumothorax to raise it’s ugly head following commencement of positive pressure ventilation in a trauma patient (if small pneumothoraces are present they will expand).
Q4. What does assessment and management of circulation with haemorrhage control involve?
Answer and interpretation
Assessment
- Pulse rate, blood pressure, capillary refill and the warmth of peripheries
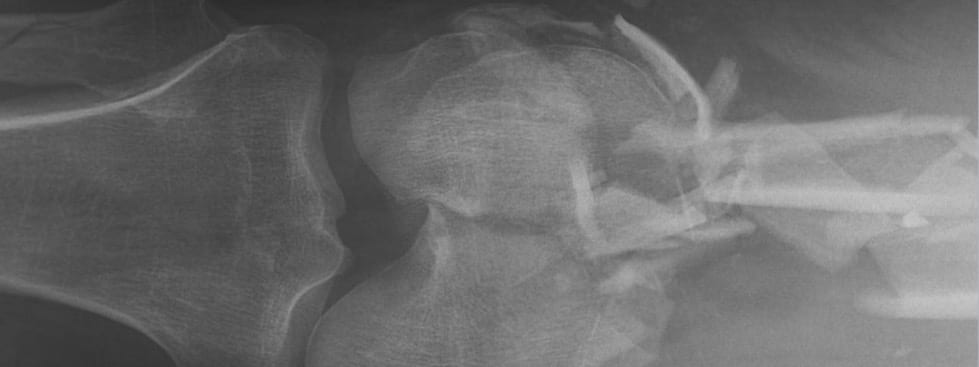
- Systematically look for evidence of bleeding. The 6 key areas are: chest, abdomen, retroperitoneum, pelvis, long bones and externally.
- Removal of all prehospital bandaging is vital – a poorly applied ‘turban’ can mask major scalp haemorrhage.
Management
- Insert 2 large bore (at least 16 gauge) intravenous cannulae, ideally in the antecubital fossae. If this cannot be rapidly achieved obtain intraosseous access (see intraosseous access).
- Send off ‘trauma bloods’ emergently, most importantly crossmatch blood.
- Venous blood gas is useful for rapid determination of lactate and initial hemoglobin.
- Others tests include full blood count, urea and electrolytes, creatinine, glucose, coagulation profile and lipase. These rarely alter initial management.
- Traditional ATLS teaching is to commence IV fluids — usually Normal Saline or Hartman’s Solution — 1-2 L STAT. Change to blood if remains haemodynamically unstable after 2 L of crystalloid, or earlier if obvious signs of major bleeding.
This approach is being superseded by the concept of damage control resuscitation. - Haemorrhage control:
— Most external bleeding can be at least temporarily controlled with direct pressure, tourniquets or by tying off vessels.
— Other measures are considered in ‘major haemorrhage’, and ultimately damage control surgery may be needed.
To learn about the cutting edge approach to damage control resuscitation list to EMCrit Podcast 12 — Trauma Resus Part 1 and EMCrit Podcast 13 — Trauma Resus Part II: Massive Transfusion.
Q5. What does disability (neurological evaluation) involve?
Answer and interpretation
Assessment
- Assess GCS and document it’s components (e.g. E4, V5, M6 = GCS 15)
- Assess pupillary size and responsiveness (if you can open the eyelids due to swelling, consider using ocular ultrasound)
- Assess gross motor and sensory function in all 4 limbs
- If you suspect a spinal injury is present a full neurological assessment is vital at the earliest opportunity — check for priapism, loss of anal sphincter tone and the bulbocavernosus reflex
- Check glucose
Management
- Airway maintenance (see above)
- Seizure control — midazolam 5-10mg IV, followed by phenytoin 18mg/kg IV over 30 minutes
- Treat hypoglycemia (glucose <3 mmol/L) with 50 mL 50% glucose
- Anxiety or agitation — treat pain, shock and search for underlying cause
- Treat raised intracranial pressure — 30 degree head up positioning, analgesia and sedation, neuromuscular blockade, manitol or hypertonic saline, arrange for urgent surgical decompression
Q6. What does exposure and environmental control involve?
Answer and interpretation
Exposure and environmental control:
- While maintaining thermostasis, completely expose the patient
- If not yet done, consider log-rolling the patient now
- Areas where potentially life threating injuries can be missed are:
— Back of head
— Back
— Buttocks
— Perineum
— Axillae
— Skin folds
Think before cutting of the patient’s clothes — it is not mandatory!
Q7. What should be examined for in the neck of a trauma patient?
Answer and interpretation
Look for TWELVE things (OK, there’s only six, so check them twice…):
- Tracheal deviation
- Wounds
- External markings
- Laryngeal disruption
- Venous distention
- Emphysema (surgical)
These findings suggest life-threatening injuries to the neck or thorax (e.g. tension pneumothorax, cardiac tamponade). I like to look for these when I’m the airway doctor as part of an assessment of A and B. I’ve specifically stressed the importance of examining the neck because it is easily forgotten when hidden by a hard collar…Also, don’t forget to check for a Horner syndrome in possible neck trauma!
Q8. What does the secondary survey involve?
Answer and interpretation
The secondary survey is carried out after the primary survey and immediate management of potential life threats in a stable patient to identify the presence of other injuries missed in the focused primary survey.
It involves a systematic ‘top-to-toe’ examination, including:
- Head, face, eyes, ears, nose and throat — carefully check the scalp and the oral cavity
- Neck
- Chest
- Abdomen
- Pelvis
- The back
- Extremities
- All wounds
Q9. What are the key aspects of history required for assessment of trauma patients and how can they be obtained?
Answer and interpretation
Around the time of the secondary survey clarification of the history is important to ensure that no injuries, or relevant comorbidities, are missed.
More details can be obtained by
- searching for witnesses or telephoning relatives
- search the patient’s wallet or mobile phone for contact details
- autopsy the patient’s clinical records
- contact the patient’s GP
A useful mnemonic to guide information is the ‘AMPLE’ history:
- Allergies and ADT status
- Medications
- Past Medical History
- Last ate and drank; LMP (check for pregnancy in females of child bearing age)
- Events / environment related to injury (i.e. a detailed account of the mechanism of injury)
Q10. What is the tertiary survey and what does it involve?
Answer and interpretation
The tertiary survey is a repetition of the secondary survey that again aims to pick up ‘missed’ injuries. This may occur on multiple occasions over the days following injury.
The multiply injured motorcyclist’s broken pinkie can be easy to miss during initial assessment!
Q11. What is the appropriate disposition of a major trauma patient?
Answer and interpretation
It depends on your location and the nature of the patient’s injuries.
In a trauma center, major trauma patients are usually admitted under the Trauma Surgery team. The patient may go straight to the operating theatre for surgical management, or be conservatively managed in an ICU/HDU setting or be observed on the ward pending a tertiary survey.
Major trauma patients, particularly in a country as large as Australia, are often first assessed and managed in smaller centres. As a result disposition can be a critical aspect of the patient’s care as delays to definitive care are associated with increased mortality. The transfer process should be commenced as soon as it becomes clear that injuries are beyond facilities capabilities.Efforts to further assess or stabilise the patient should not delay transfer.
To optimize the care of major trauma patients in non-trauma centers systems should be in place locally to make the transfer process as quick and easy for the referring hospital. A dedicated member of staff may need to concentrate on the transfer process while others continue to assess and manage the patient.
Teaching VIDEO from OME
This teaching video shows the stages of initial trauma assessment in an OSCE style format. The video is useful for demonstrating a traditional, comprehensive systematic approach. Note that in reality, many of the steps will occur simultaneously and be performed by multiple different team members. Some of the examinations performed (such as chest percussion) are not particularly useful are are rarely performed in practice.
References
- EMBasic Podcast — Trauma Resuscitation: Part 1 – Evaluation and Part 2 – Interventions
CLINICAL CASES
Trauma Tribulation
Chris is an Intensivist and ECMO specialist at the Alfred ICU in Melbourne. He is also a Clinical Adjunct Associate Professor at Monash University. He is a co-founder of the Australia and New Zealand Clinician Educator Network (ANZCEN) and is the Lead for the ANZCEN Clinician Educator Incubator programme. He is on the Board of Directors for the Intensive Care Foundation and is a First Part Examiner for the College of Intensive Care Medicine. He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives.
After finishing his medical degree at the University of Auckland, he continued post-graduate training in New Zealand as well as Australia’s Northern Territory, Perth and Melbourne. He has completed fellowship training in both intensive care medicine and emergency medicine, as well as post-graduate training in biochemistry, clinical toxicology, clinical epidemiology, and health professional education.
He is actively involved in in using translational simulation to improve patient care and the design of processes and systems at Alfred Health. He coordinates the Alfred ICU’s education and simulation programmes and runs the unit’s education website, INTENSIVE. He created the ‘Critically Ill Airway’ course and teaches on numerous courses around the world. He is one of the founders of the FOAM movement (Free Open-Access Medical education) and is co-creator of litfl.com, the RAGE podcast, the Resuscitology course, and the SMACC conference.
His one great achievement is being the father of three amazing children.
On Twitter, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
