Pyelonephritis
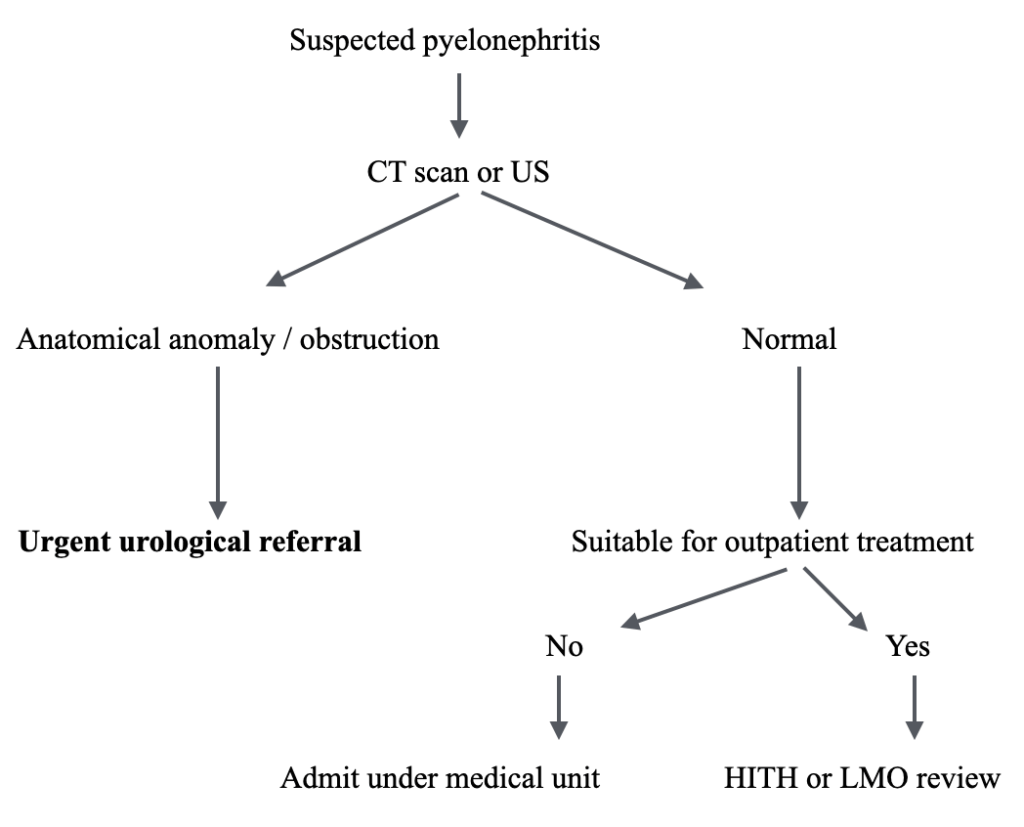
Pyelonephritis is a common presentation to the Emergency Department. The most important consideration is renal tract imaging to rule out an obstructive cause, which can rapidly lead to severe sepsis.
Urgent urological consultation is required in such cases. Patients with red flags for serious illness must be identified and treated urgently.
Epidemiology
- Occurs in any age group, peak incidence in females aged 15 to 30 years.
Pathophysiology
- Infection of the renal parenchyma and pelvic-calyceal system.
- Typically from bacterial ascent from the bladder or, less commonly, haematogenous spread.
Common organisms:
- Escherichia Coli (>80%)
- Klebsiella species (5-20%)
- Proteus, Enterobacter, and Pseudomonas species (less common)
Risk Factors
- Immunocompromised states
- Pregnancy
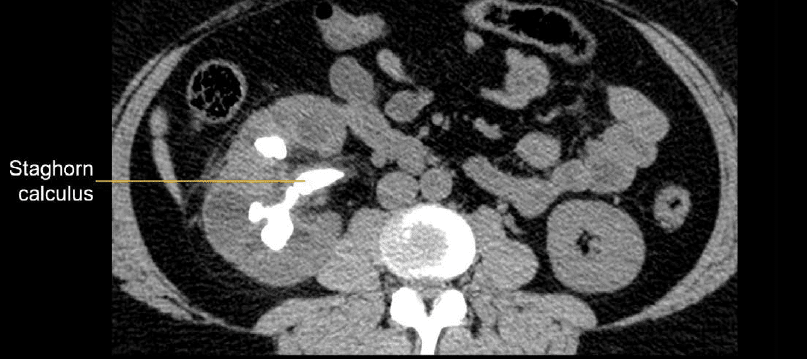
- Urinary tract obstruction (e.g., renal calculi, PUJ obstruction, prostatomegaly)
- Vesico-ureteric reflux (children)
- Anatomical urinary tract abnormalities
Complications
- Septic shock
- Renal or perinephric abscess
- Acute papillary necrosis with possible obstruction
Clinical Features
- Fever, rigors, myalgias, nausea, vomiting
- Loin pain/tenderness
- Urinary symptoms (frequency, dysuria)
- Confusion in the elderly
Features of severe pyelonephritis:
- Fever ≥38°C
- Systemic symptoms
- Sepsis or septic shock
High-risk groups:
- Elderly, immunocompromised, pregnant women
- History of recurrent UTIs
- Renal transplant, single kidney, anatomical abnormalities
- Obstructive lesions, recent instrumentation
- Chronic conditions (diabetes, renal disease, neurological disease)
Differential Diagnoses
- Acute cholecystitis, diverticulitis, appendicitis
- Renal colic, paraspinal pain or infections
- Renal vein thrombosis, lower lobe pneumonia
- Pelvic inflammatory disease
Investigations
Bloods:
- FBE: increased WCC
- CRP: elevated
- U&Es, glucose
- Blood cultures if unwell
Urine:
- FWT (leukocytes, nitrites)
- Microscopy and culture
Imaging:
Ultrasound:
- Useful screen for obstruction, not reliable for detecting stones
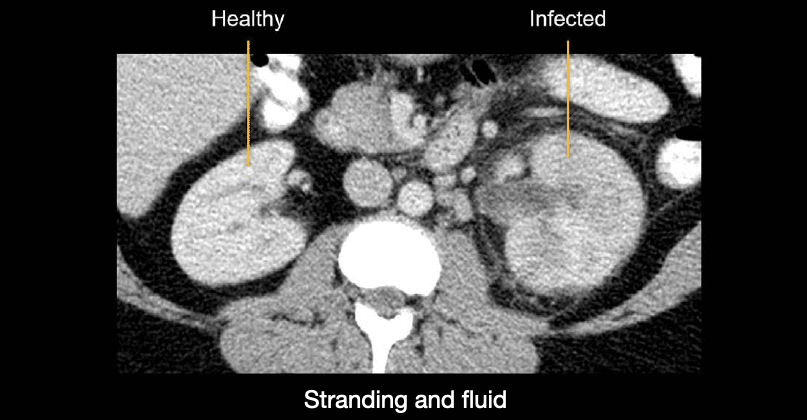
CT scan:
- Preferred if patient unwell
- Non-contrast CT to detect stones
- Contrast CT for detailed infection assessment (reduced enhancement, abscess)
MRI:
- Alternative in pregnancy
Management
- Analgesia as required
- IV fluid resuscitation
- Antibiotics:
Mild cases:
- Oral amoxycillin-clavulanate or ciprofloxacin (if no contraindications)
- Tailor to culture results (e.g., amoxycillin, cephalexin, trimethoprim)
Moderate to severe cases:
- IV ceftriaxone or cefotaxime
- Gentamicin plus ampicillin/amoxycillin
Obstructive pyelonephritis:
- Urgent Urology review
- May require nephrostomy
Duration:
- Total 10-14 days
- Ciprofloxacin for 7 days may suffice in uncomplicated cases
Disposition
Mild cases:
- Consider outpatient management if adult, no red flags, and adequate support
Moderate to severe cases:
- Admit for IV antibiotics
- Consider Short Stay Unit if appropriate
- Admit to Urology if obstructive lesion
- Refer unwell patients to HDU/ICU
Appendix 1:
Appendix 2:
References
FOAMed
- Davidson J. CT Case 014. LITFL
- Hartung MP. Abdominal CT: renal infections. LITFL
- Rippey J. Ultrasound Case 093. LITFL
- Nickson. Urosepsis. LITFL
- Cunningham K. Abdominal Imaging Cases 006. LITFL
Publications
- Kalra OP, Raizada A. Approach to a patient with urosepsis. Journal of global infectious diseases. 1(1):57-63. 2009.
- Wagenlehner FM, Lichtenstern C, Rolfes C. Diagnosis and management for urosepsis. International Journal of Urology. 20(10):963-70. 2013.
Fellowship Notes
Physician in training. German translator and lover of medical history.
Educator, magister, munus exemplar, dicata in agro subitis medicina et discrimine cura | FFS |

