Third Cranial Nerve Lesions
Cranial nerve III is also known as the Oculomotor nerve.
It carries motor and autonomic nerve fibres.
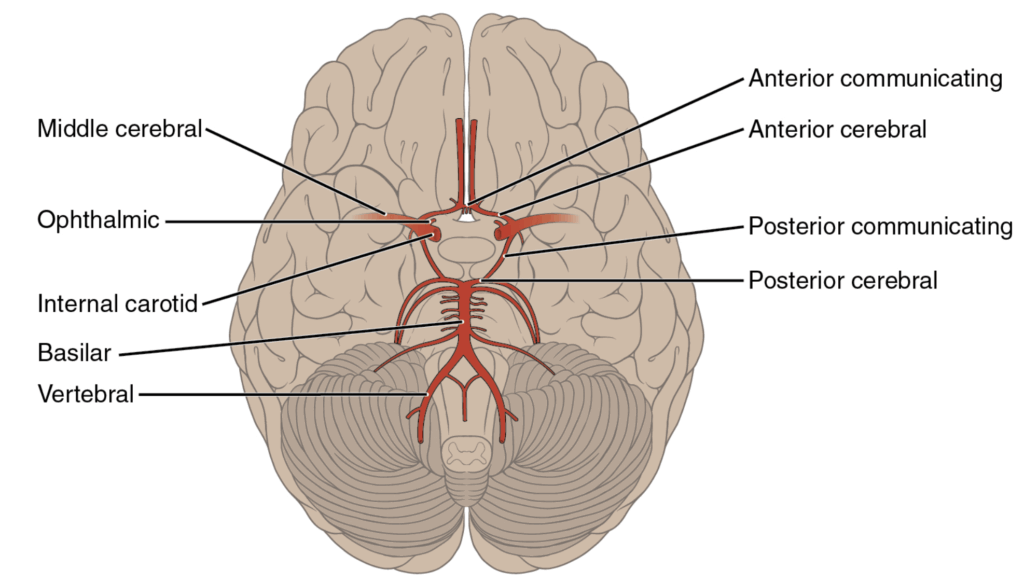
From an Emergency Department perspective, an aneurysm of the posterior communicating artery is the most serious cause in non-trauma cases and this always needs to be excluded.
Anatomy
Course of the Oculomotor Nerve
- The somatic motor nucleus of the oculomotor nerve is located in the mid region of the midbrain.
- The parasympathetic autonomic nucleus is the Edinger-Westphal nucleus, also in the midbrain.
The nerve:
- Emerges from the ventral brainstem, superior to the pons and at the medial margin of the cerebral peduncle of the midbrain.
- Runs forward within the lateral wall of the cavernous sinus, just above the trochlear nerve.
- Divides into:
- Superior ramus
- Inferior ramus
Both rami enter the orbit via the superior orbital fissure.
Mnemonic for structures passing superior to inferior:
“Lazy French Tarts Sitting Naked In Anticipation”: Lacrimal nerve, Frontal nerve, Trochlear nerve, Superior ramus of the oculomotor nerve, Nasociliary nerve, Inferior ramus of the oculomotor nerve, Abducens nerve.
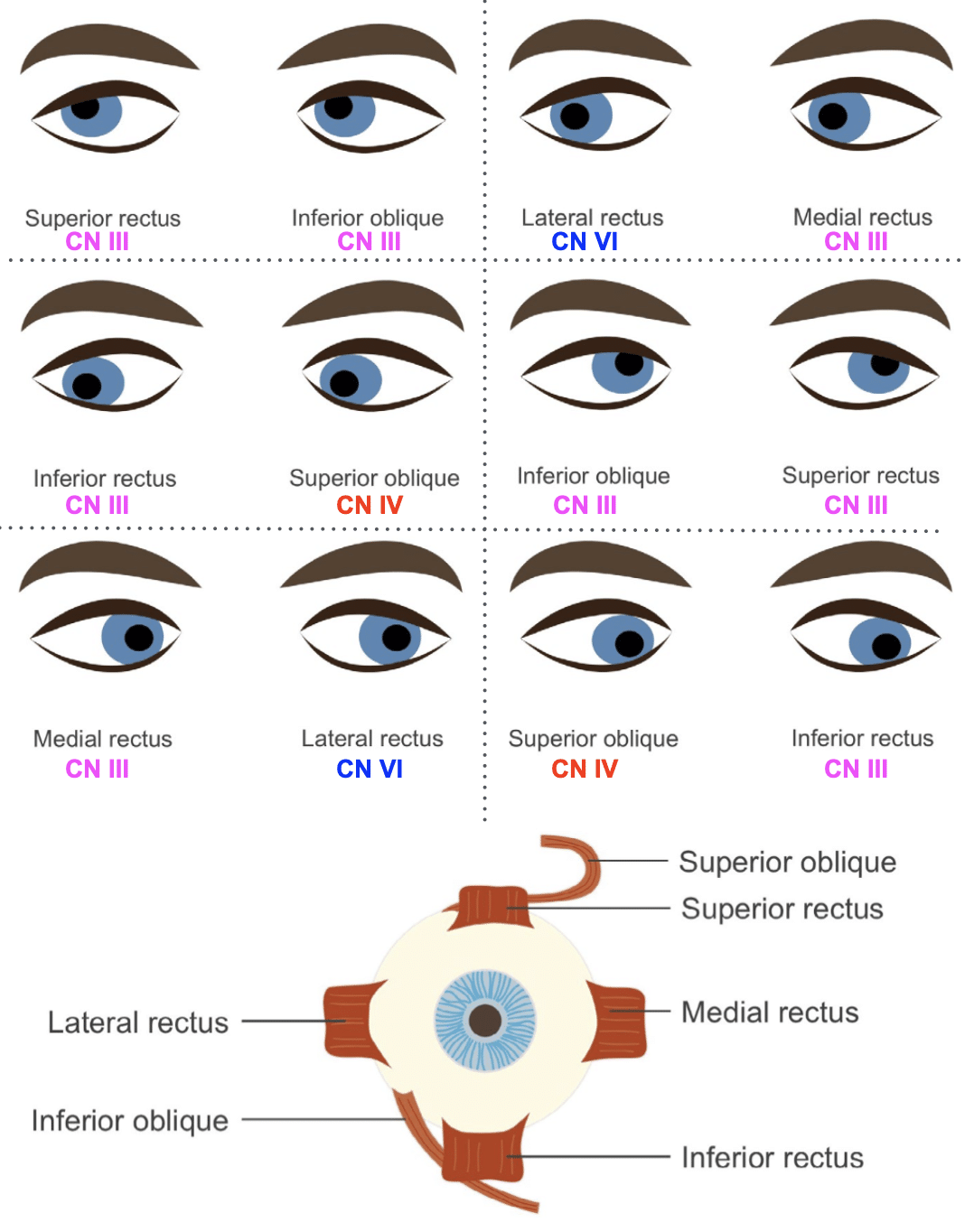
Oculomotor Nerve Innervations
| Ramus | Structures Supplied |
|---|---|
| Superior ramus | – Superior rectus (elevates eye maximally when abducted) – Levator palpebrae superioris (raises upper eyelid; also receives sympathetic fibres) |
| Inferior ramus | – Inferior rectus (depresses eye, maximally when abducted) – Medial rectus (pulls eye medially) – Inferior oblique (pulls eye up and out) – Sends branch to ciliary ganglion → parasympathetic fibres to eye via short ciliary nerves |
Pathology
Causes of a third cranial nerve lesion include:
- Demyelinating disease
- Multiple sclerosis
- Vascular disease
- Brainstem microvascular strokes
- Space-occupying lesions
- Tumours
- Aneurysm of the posterior communicating artery (must be excluded)
- Abscesses
- Raised intracranial pressure
- Venoms
- Snakebite
- Thiamine deficiency
- Seen in Wernicke’s encephalopathy (as one manifestation of ophthalmoplegia)
- Trauma
- Skull base trauma
- Unilaterally dilated pupil ± ipsilateral third nerve palsy may indicate impending cerebral herniation
- Mononeuritis
- Diabetes
- Toxins
- Microvascular disease
- Paraneoplastic disease
- Connective tissue disease
- Infections (HIV, Lyme disease, syphilis)
- Idiopathic
- No clear cause found in some cases
- Rarely
Clinical Assessment
Important Points of History
- Presenting problem usually one of diplopia.
- If headache present, raises suspicion for:
- Cerebral aneurysm (acute bleed or expansion)
- Intracranial tumours
- Raised intracranial pressure
Important Points of Examination
- Strabismus
- Obvious squint of the affected eye
- Eye typically lies “down and out” (inferior and lateral)
- Pupil dilation
- Pupil may or may not be dilated
- Ptosis
- Complete or partial ptosis
- Eye movement testing
- Eye is “down and out” with third nerve lesion
- To test for associated fourth nerve (trochlear) lesion:
- Ask patient to look down then across to opposite side
- Eye will intort if fourth nerve is intact

Investigations
Blood Tests
- FBC
- CRP
- ESR
- U&Es / glucose
CT Angiogram
- Urgent imaging required to rule out posterior communicating artery aneurysm.
- CT angiography reasonable option, but not as sensitive as MRI/MRA.
- Will also detect other space-occupying lesions causing third nerve palsy.
MRI
- Preferred imaging for detecting cerebral aneurysm.
- Most sensitive and specific for other intracranial or orbital space-occupying lesions.
Angiography
- Formal angiography is gold standard but invasive; rarely required.
Management
- Management directed at the underlying cause.
- If posterior communicating artery aneurysm is found:
- Patient should be kept in hospital pending neurosurgical consultation.
- Clear follow-up plan must be arranged with neurosurgery before discharge from Emergency Department.
Appendix 1

Appendix 2
References
Publications
- Golshani K, Ferrell A, Zomorodi A, Smith TP, Britz GW. A review of the management of posterior communicating artery aneurysms in the modern era. Surg Neurol Int. 2010 Dec 22;1:88.
- Zelman S, Goebel MC, Manthey DE, Hawkins S. Large Posterior Communicating Artery Aneurysm: Initial Presentation with Reproducible Facial Pain Without Cranial Nerve Deficit. West J Emerg Med. 2016 Nov;17(6):808-810.
- Brazis PW, Masdeu JC, Biller J. Localization in Clinical Neurology. 8e 2021
- Fuller G. Neurological Examination Made Easy. 6e 2019
- O’Brien M. Aids to the Examination of the Peripheral Nervous System. 6e 2023
FOAMed
- Coni R. Neuro 101: Cranial Nerves. LITFL
- Nickson C. More Befuddling Pupillary Asymmetry. LITFL
- Nickson C. Third Cranial Nerve Lesions. LITFL
- Nickson C. Cranial nerve lesions DDx. LITFL
Fellowship Notes
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner
Educator, magister, munus exemplar, dicata in agro subitis medicina et discrimine cura | FFS |


