Ulnar Nerve Lesions
Ulnar nerve lesions cause claw hand, sensory loss in the medial hand, and weakness of grip. Most often due to trauma, compression, or neuropathy.
Ulnar nerve lesions are characterized predominantly by:
High lesions:
- Affects flexor carpi ulnaris, flexor digitorum profundus (digits IV–V), and intrinsic hand muscles
- Functional loss includes:
- Opening of the hand
- Loss of grip strength
- Reduced pincer strength
Low lesions:
- At or near wrist/palm
- Paralysis of:
- Hypothenar muscles
- All interossei
- Adductor pollicis
- ½ of flexor pollicis brevis
- Palmaris brevis
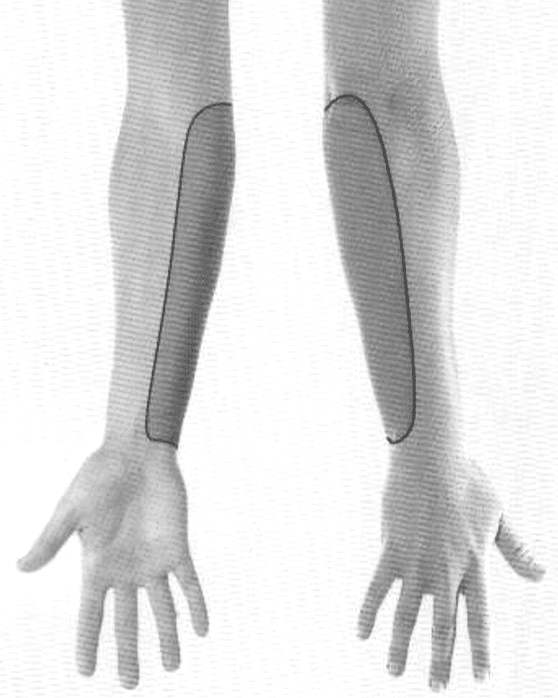
Sensory deficits may involve:
- Medial forearm
- Medial palm and dorsal hand
- Medial 1½ fingers
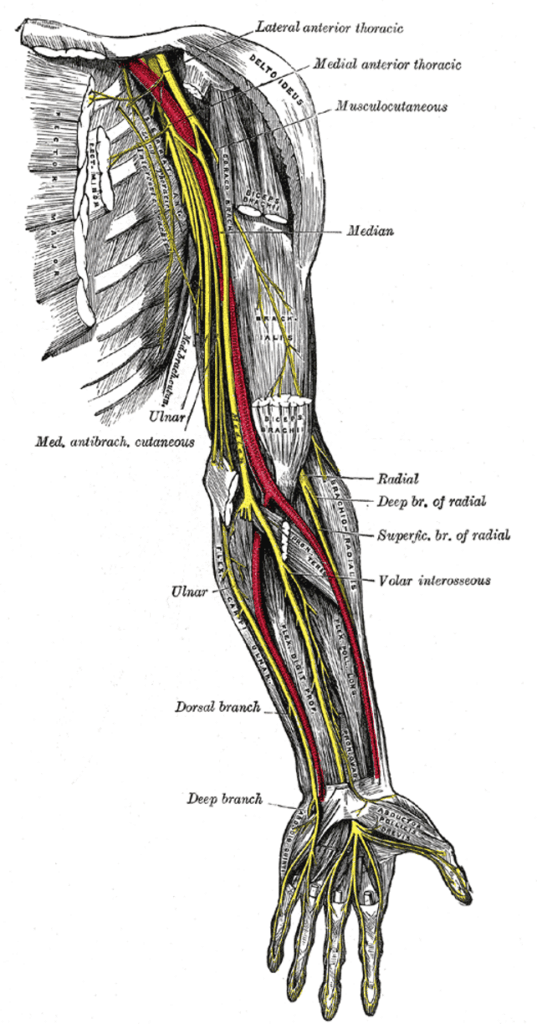
Anatomy
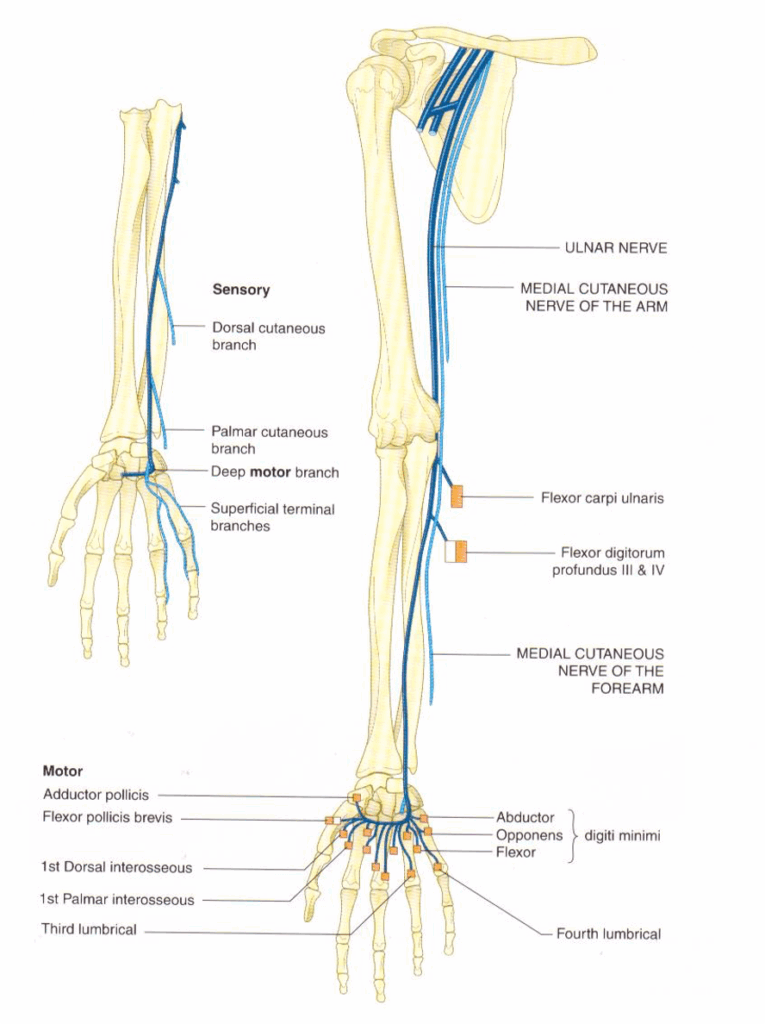
Course of the ulnar nerve
- Origin: C7–T1, from the medial cord of the brachial plexus
- Travels medial to the brachial artery, pierces the medial fascial septum
- Behind medial epicondyle, enters forearm between flexor carpi ulnaris heads
- Descends with ulnar artery, superficial at the wrist
- Divides into deep and superficial branches at the palm
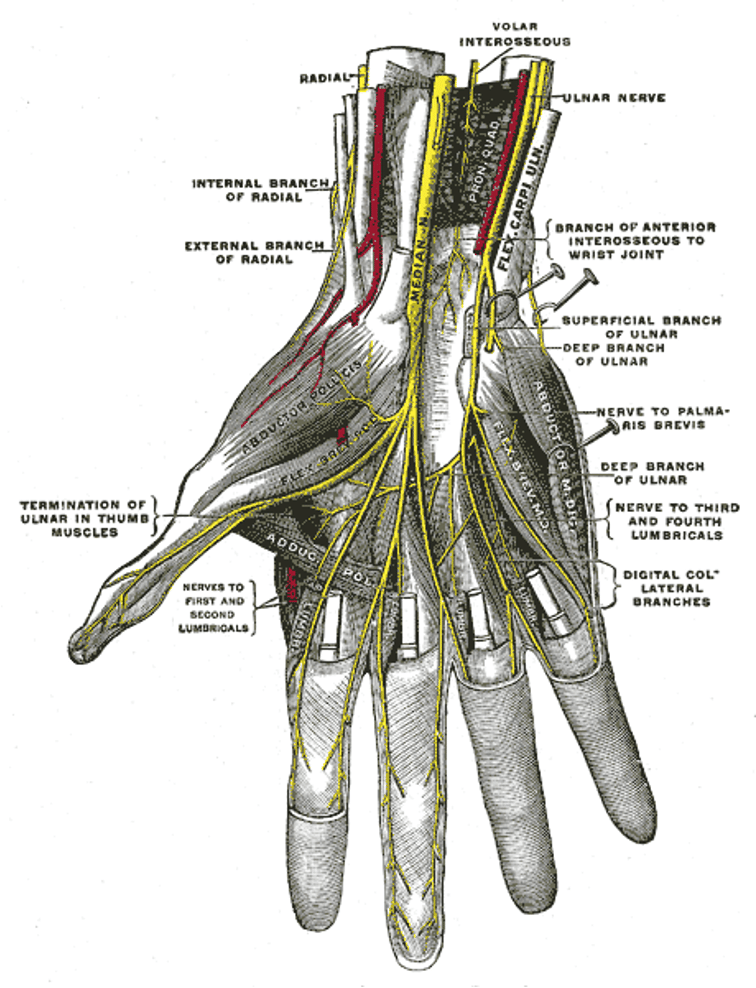
Ulnar Nerve Innervations
Proximal forearm:
- Flexor carpi ulnaris
- Flexor digitorum profundus (digits III & IV)
Distal forearm:
- Dorsal cutaneous branch: medial hand and 1½ fingers
- Palmar cutaneous branch
Hand (deep branch):
- Hypothenar muscles
- Adductor pollicis
- ½ of flexor pollicis brevis
- All interossei
- 3rd & 4th lumbricals
Hand (superficial branch):
- Palmaris brevis
- Sensory to medial 1½ fingers
Actions of Ulnar-Innervated Muscles
| Muscle | Action |
|---|---|
| Flexor carpi ulnaris | Flexes/adducts hand |
| FDP (digits III & IV) | Flexes distal phalanges |
| Abductor digiti minimi | Abducts little finger |
| Opponens digiti minimi | Rotates 5th MC, cupping |
| Flexor digiti minimi | Flexes little finger |
| Adductor pollicis | Thumb adduction |
| ½ Flexor pollicis brevis | Flexes thumb (MCP joint) |
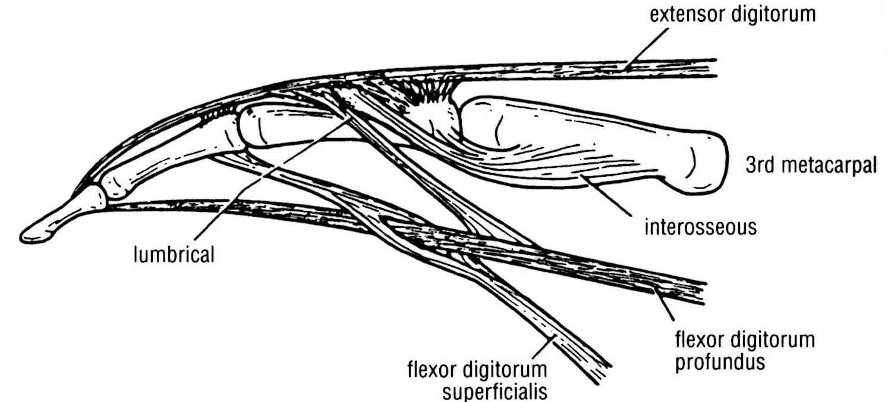
| Interossei | Finger adduction/abduction; MCP flexion, IP extension |
| Lumbricals (III & IV) | Flex MCP, extend IP (digits 3 & 4) |
Pathology
Causes of Ulnar Nerve Lesions
- Trauma:
- Penetrating or blunt trauma
- Neuropraxia:
- Compression at medial epicondyle
- Prolonged elbow pressure
- Compartment syndrome
- Mass lesions:
- Tumours
- Abscesses
- Neuropathies (mononeuritis):
- Diabetes mellitus
- Malignancy
- Infection: leprosy, HIV
- CTDs: RA, SLE, PAN, scleroderma, sarcoidosis
- Other: amyloidosis, Lyme disease, heavy metals
Clinical Assessment
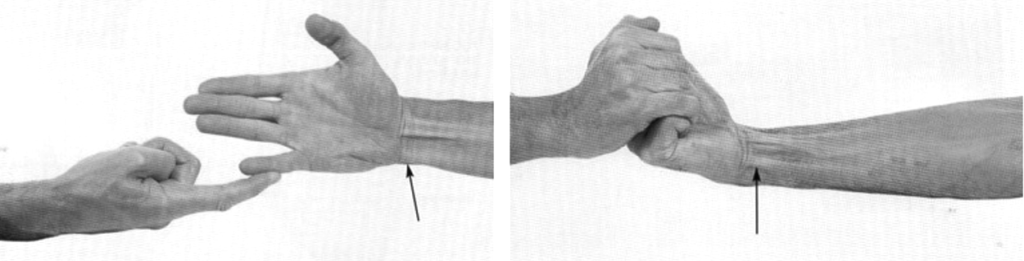
Right: Flexor carpi ulnaris (ulnar nerve C7,8 T1). The patient is flexing and adducting the hand at the wrist against resistance. Arrowed: the tendon can be seen and felt.
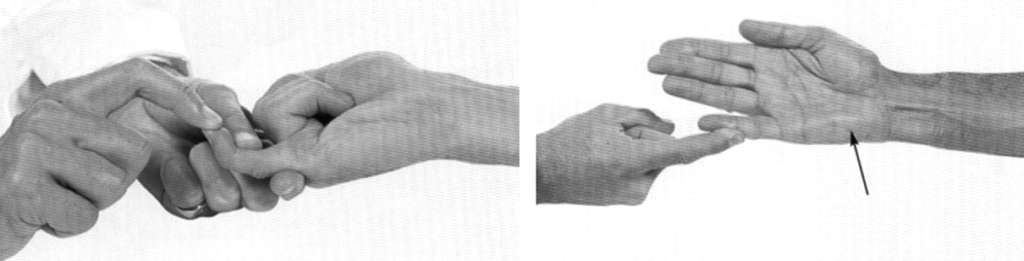
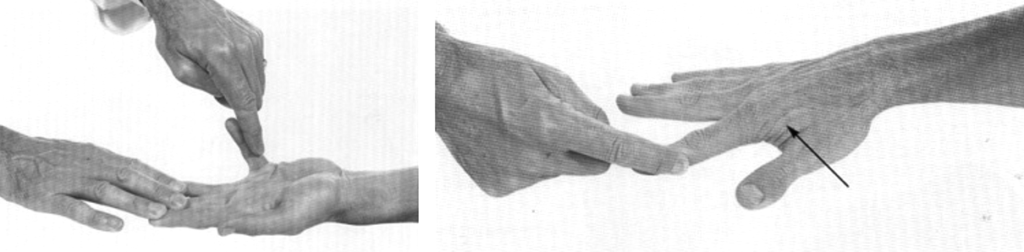
Right: First dorsal interosseous muscle, (ulnar nerve, C8, T1). The patient abducts the index finger against resistance. Arrow: the muscle belly can be felt, and often seen
Right: Adductor pollicis, (ulnar nerve C8, T1). The patient is adducting the thumb at right angles to the palm against the resistance of the examiner’s finger.
Ulnar Nerve Deficits
At the elbow:
- Motor:
- Paralysis of FCU and medial FDP
- Weak wrist flexion and deviation
- Sensory:
- Loss over medial third of hand (both surfaces), medial 1½ fingers
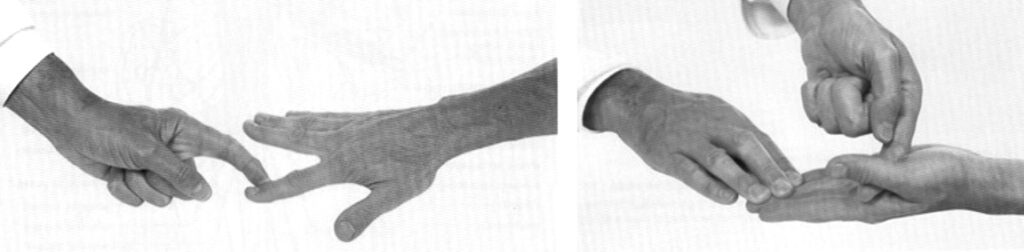
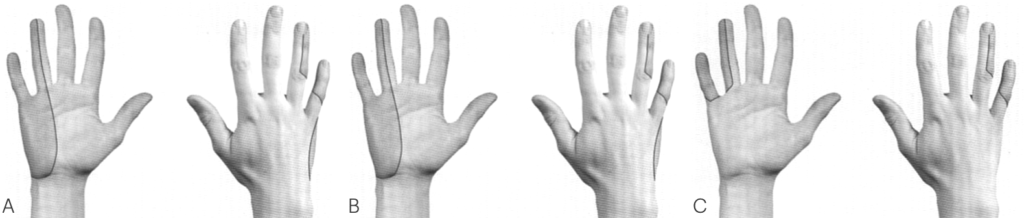
At the wrist — Claw Hand:
- Intrinsic hand muscles paralyzed
- Thenar muscles and lumbricals I–II (median nerve) spared
Motor deficits:
- Loss of finger ab/adduction
- Impaired pincer grip
- MCP hyperextension (esp. digits IV–V)
- IP flexion (digits IV–V)
- Hypothenar wasting
- Dorsal interosseous wasting
Sensory loss:
- Palmar and dorsal surfaces of medial 1½ fingers
- Palmar cutaneous and dorsal cutaneous branches often involved
Investigations
When clear-cut, investigations may not be necessary.
Consider:
- Nerve conduction studies
- Diagnostic clarification
- Rule out generalised disease
- Prognostic information
- Blood tests:
- FBC, U&Es/glucose, CRP, ESR, others (e.g. lead levels)
- CT/MRI:
- Mass lesion delineation
- Nerve visualisation
- Biopsy:
- Rarely for mononeuritis or suspected leprosy
Management
- Treat the cause
- Compartment syndrome:
- Fasciotomy if appropriate
- Occupational therapy:
- Splinting, support devices
- Physiotherapy:
- Rehab, prevention of secondary complications
Disposition
Dependent on:
- Cause
- Severity
- Onset
Appendix 1
Ulnar Nerve Anatomy
Appendix 2
Appendix 3

What is the Ulnar paradox?
An injury to the ulnar nerve will result in the classical ulnar claw. However this is mainly seen in more distal injuries. The ulnar nerve also innervates the ulnar half of the flexor digitorum profundus (FDP) muscle. If the ulnar nerve lesion occurs more proximally (closer to the elbow), the flexor digitorum profundus muscle may also be denervated. As a result, flexion of the IP joints is weakened, which reduces the claw-like appearance of the hand.
Simply put, as reinnervation occurs along the ulnar nerve after a high lesion, the deformity will get worse (FDP reinnervated) as the patient recovers – hence the use of the term “paradox”.
A simple way to remember this is: ‘the closer to the Paw, the worse the Claw’.
References
Publications
- Brazis PW, Masdeu JC, Biller J. Localization in Clinical Neurology. 8e 2021
- Fuller G. Neurological Examination Made Easy. 6e 2019
- O’Brien M. Aids to the Examination of the Peripheral Nervous System. 6e 2023
FOAMed
- Coni R. Neuro 101: Peripheral Nervous System. LITFL
- Nickson C. Myotomes and Differentiating Nerve Lesions. LITFL
Fellowship Notes
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner
Educator, magister, munus exemplar, dicata in agro subitis medicina et discrimine cura | FFS |


