FFS: Horner Syndrome
Horner syndrome — also known as oculosympathetic paresis — is a neurological condition caused by disruption of the sympathetic pathway to the eye and face. It is characterized by the classic triad of miosis, partial ptosis, and anhidrosis +/- enophthalmos
Horner syndrome is a neurologic syndrome that classically presents with:
- Miosis – producing an obvious anisocoria (unequal pupil sizes)
- Ptosis
- Anhidrosis
- Enophthalmos – actually a pseudoenophthalmos, where the eye appears sunken due to narrowing of the palpebral aperture from ptosis
Horner’s syndrome results from a lesion of the ipsilateral sympathetic innervation to the eye, anywhere along the neural pathway:
- Brainstem – hypothalamus, sympathetic nucleus
- Cervical and upper thoracic spinal cord
- Sympathetic chain and stellate ganglion
- Carotid sympathetic plexus
Causes range from benign to serious.
History
The syndrome is eponymously attributed to Swiss ophthalmologist Johann Friedrich Horner (1831-1886), who published a comprehensive case in 1869.
However, earlier descriptions exist, notably by François Pourfour du Petit (1664–1741), Edward Selleck Hare (1812-1838), and Silas Weir Mitchell (1829-1914), prompting historical debate over attribution. In France, the condition is known as Bernard-Horner syndrome, acknowledging Claude Bernard’s experimental work.
Anatomy
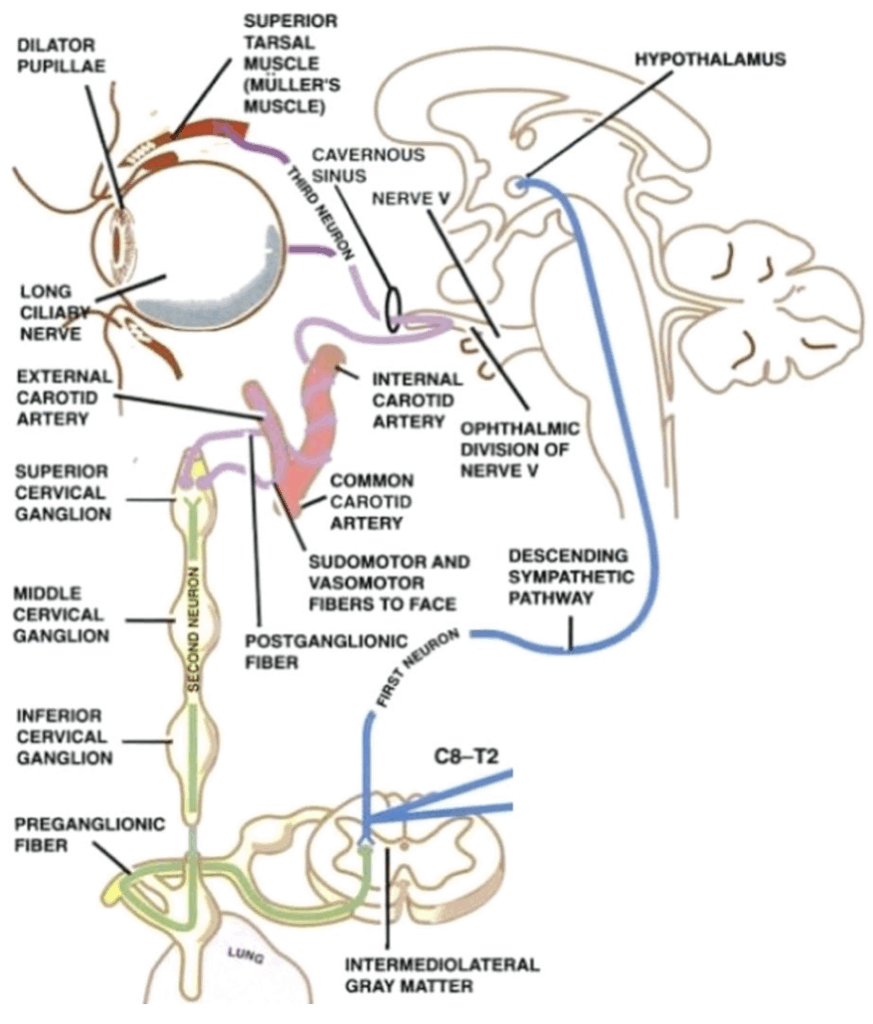
Horner’s syndrome involves a three-neuron sympathetic pathway originating in the hypothalamus:
- First-order neurons – descend to the cervical spinal cord (C8–T2)
- Second-order neurons – travel through the sympathetic trunk, brachial plexus, over the lung apex, then ascend to the superior cervical ganglion near the mandible
- Third-order neurons – ascend with the internal carotid artery, pass through the cavernous sinus (near CN VI), and join the ophthalmic division of CN V to innervate the iris dilator and Müller’s muscle
Pathophysiology
Causes
Congenital
- Can occur with birth trauma
- Associated with heterochromia (affected iris lighter)
Acquired – best classified by anatomical region:
- Brainstem / upper spinal cord
- Vascular (e.g. lateral medullary syndrome)
- Tumour
- Syringobulbia, syringomyelia
- Demyelination (e.g. MS)
- Neck
- Tumour (e.g. thyroid, lymph nodes)
- Trauma or surgery
- Vascular: carotid dissection, aneurysm, arteritis
- Chest
- Apical lung tumours (Pancoast) – look for T1 signs
- Intracranial (non-brainstem)
- Carotid aneurysms
- Cavernous sinus disease (e.g. cluster headache)
Note: In many cases, no cause is found.
Clinical features
“Everything gets smaller” in Horner’s syndrome
- Partial ptosis – mild (<2 mm), affects Müller’s muscle. May involve lower lid (upside-down ptosis).
- Miosis – small pupil with normal reflexes; anisocoria more prominent in dark.
- In congenital cases, heterochromia may be present.
- Anhidrosis – facial anhidrosis present in central/pre-ganglionic lesions, often absent in postganglionic lesions
- Enophthalmos – apparent, not true, due to ptosis

Associated neurological features
These help localise the lesion:
- Brainstem signs (e.g. diplopia, vertigo) → brainstem
- Myelopathy (weakness, long tract signs) → cervicothoracic cord
- Brachial plexus signs (arm pain/weakness) → lung apex
- Isolated CN VI palsy → cavernous sinus
- Horner’s with neck pain/mass → carotid dissection
Investigations
Tailored to suspected cause:
- CXR – apical lung mass
- Carotid Doppler ultrasound – initial screen
- CT / CT angiogram – head, neck, chest, carotids
- MRI / MRA – best for brainstem, spinal cord, carotids (avoids contrast)
Management
- Treatment is directed at the underlying cause.
Appendix 1
References
Publications
- Horner JF. Über eine Form von Ptosis. Klinische Monatsblätter für Augenheilkunde 1869;7:193-198
- Kisch B. Horner’s syndrome, an American discovery. Bull Hist Med. 1951 May-Jun;25(3):284-8.
- Onuigbo WI. John Reid (1809-49) and Horner’s syndrome. Scott Med J. 1958 May;3(5):218-20.
FOAMed
- Cadogan M. Horner Syndrome. LITFL
- Cadogan M. Johann Friedrich Horner. LITFL
- Nickson C. Horner Syndrome. LITFL
- Nickson C. Horner syndrome DDx. LITFL
Fellowship Notes
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner
Educator, magister, munus exemplar, dicata in agro subitis medicina et discrimine cura | FFS |


