Acute Coronary Syndromes Literature Summaries
THROMBOLYSIS
Fibrinolytic Therapy Trialists Group. Indications for fibrinolytic therapy in suspected AMI: collaborative overview of early mortality and major morbidity results from all randomised trials of more than 1000 patients. Lancet 1994; 343:311-322
- meta-analysis
- n = 58600 -> thrombolysis associated with excess deaths on day 0-1 -> survival benefit during days 2-35 -> give as soon as possble -> stroke risk = 4/1000 in first 24 hrs
Second International Study of Infarct Survival Collaborative Group. Randomised trial of intravenous streptokinase, oral aspirin, both or neither among 17,187 cases of suspected AMI: ISIS-2. Lancet 1998;2:349-360.
-> streptokinase & aspirin was additive in terms of reducing death and this benefit persisted with 10 yr follow up.
THROMBOLYSIS VS PCI
Andersen et al, A comparision of coronary angioplasty with fibrinolytic therapy in AMI, N Engl J Med 2003;349:733-742
- RCT
- n = 1572
- STEMI’s
- ateplase or angioplasty -> PCI superior to thrombolysis in terms of reinfarction but not mortality -> must transfer to cathlab within 2 hrs
Keeley EC, et al. Primary angioplasty vs IV thrombolytic therapy for AMI: a quantitative review of 23 randomised trials. Lancet 2003;361:13-20.
- n = 7739
- STEMI’s
- PTCA vs thromolysis -> PTCA associated with a significant reduction in short-term mortality, non-fatal reinfarction and combinded end point of death, non-fatal reinfarction and stroke.
PCI
Morce MC, et al. A randomised comparison of a sirolimus-eluting stent with a standard stent for coronary revascularization. N Engl J Med 2002;346:1773-1780.
- RCT
- n = 238
- uncoated vs sirolimus-eluting stents
- single, primary lesions in native coronaries -> at 6 months significant reduction in neo-intimal proliferation and degree of stent stenosis -> at 1 yr there is a significant reduction in major cardiac events
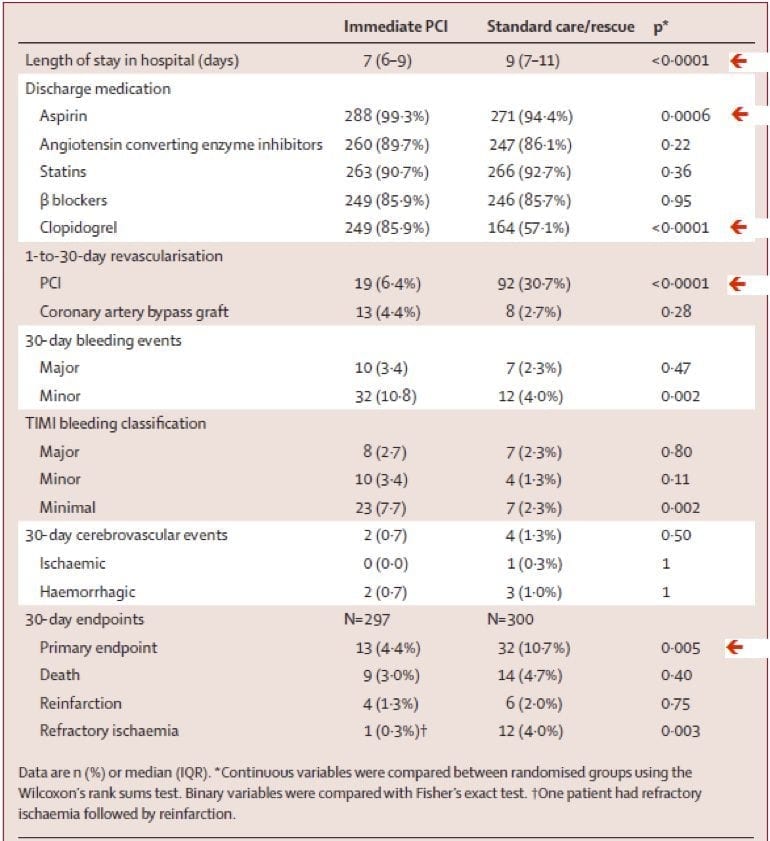
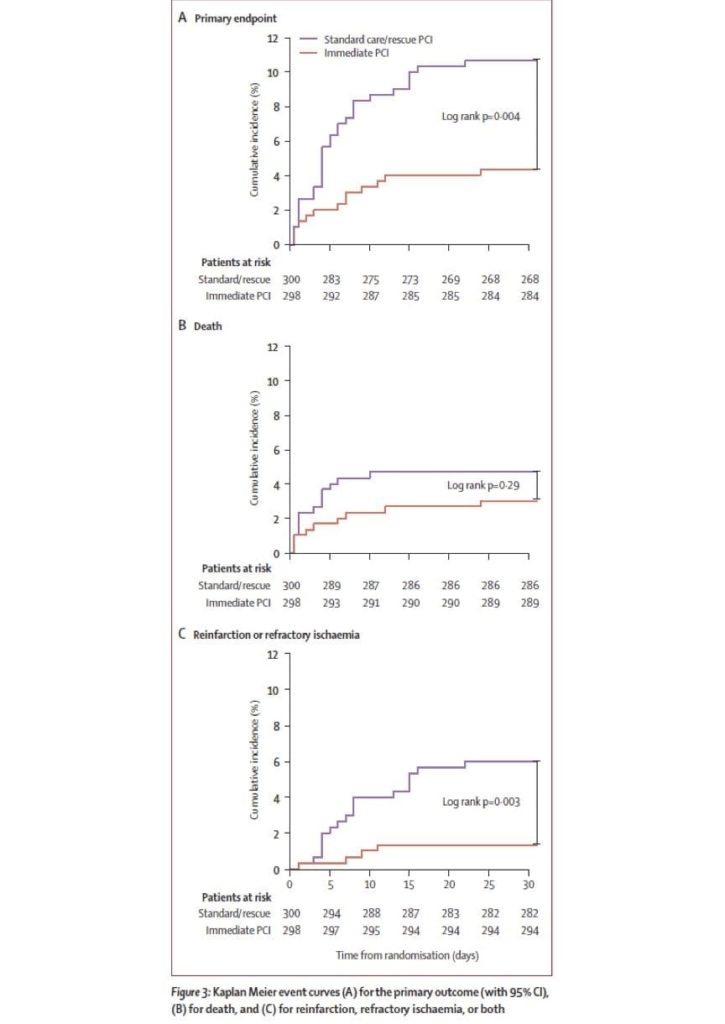
Di Mario, C. et al (2008) “Immediate angioplasty versus standard therapy with rescue angioplasty after thrombolysis in the Combined Abciximab REtetplase Stent Study in Acute Myocardial Infarction (CARESS-in-AMI): an open, prospective, randomized, multicentre trial” Lancet 371:559-68
- MRCT
- open
- n = 600
- inclusion criteria: 90min or clinical deterioration
- primary end points = death, reinfarction or refractory ischaemia @ 30 days -> immediate transfer for PCI improves outcome in high risk patients with STEMI -> no significant increase in major bleeding or strokes -> criticism: generalizability to our situation -> these patients are an incredibly few and high risk, primary outcome only significant when sub-groups combined not individually.
MEDICAL MANAGEMENT
The Epic Investigators. Use of a monoclonal antibody directed against the platelet glycoprotein IIb/IIIa receptor in high-risk coronary angioplasty. N Engl J Med 1994; 330:956-961
- RCT
- n = 2099
- abcixmab vs placebo
- severe unstable angia, evolving acute MI or high risk plaque morphology -> significant reduction in death, non-fatal MI, unplanned repeat PCI & surgical revascularisation
First International Study of Infarct Survival Collarborative Group. Randomised trial of Intravenous atenolol 16, 027 cases of suspected AMI: ISIS-1. Lancet 1986; 2:57-66
- RCT
- n = 16,027
- atenolol vs placebo -> atenolol group had significant reduction in mortality @ 1 yr
Magnesium in Coronaries (MAGIC) Trial Investigators. Early administration of IV Magnesium to high risk patients with AMI in the Magnesium in Coronaries Trial. Lancet 2002;360:1189-1196.
- RCT
- n = 6213
- STEMI given Mg2+ or placebo -> no change in 30-day mortality
The Platelet Receptor Inhibition in Ischemic Syndrome Management in Patients Limited by Unstable Signs & Symptoms (PRISM-PLUS) Study Investigators. Inhibition of the platelet glycoprotein IIb/IIIa receptor with tirofiban in unstable angina and non-Q wave MI. N Engl J Med 1998;338:1488-1497
- RCT
- n = 1915
- groups aspirin + (1) tirofiban, (2) unfractionated heparin, (3) tirofiban + heparin -> tirofiban + heparin experienced lower incidence of death, MI or refractory ischaemia within 7 days -> no significant increase in bleeding compared to those receiving heparin
Petersen JL, et al. Efficacy and bleeding complications among patients randomized to enoxaparin or UFH for antithrombin therapy in non-ST segment elevation acute coronary syndromes: a systematic review. JAMA 2004; 294:89-96.
- systematic review -> enoxaparin is better than UFH in preventing combined end point of death or MI without an increase in bleeding.
Yusuf S, et al. The Clopidogrel in Unstable Angina to Prevent Recurrent Events Trial Investigators. Effects of clopidogrel in addition to aspirin in patients with ACS without ST-segment elevation. N Engl J Med 2001; 345:494-502.
- RCT
- n = 12,562
- patients presenting with 12hr from onset of symptoms -> 20% relative reduction death, MI & stroke. -> significant increase in bleeding
References
- Indications for fibrinolytic therapy in suspected acute myocardial infarction: collaborative overview of early mortality and major morbidity results from all randomised trials of more than 1000 patients. Fibrinolytic Therapy Trialists’ (FTT) Collaborative Group. Lancet. 1994 Feb 5;343(8893):311-22. [PMID 7905143]
- Randomised trial of intravenous streptokinase, oral aspirin, both, or neither among 17,187 cases of suspected acute myocardial infarction: ISIS-2. ISIS-2 (Second International Study of Infarct Survival) Collaborative Group. Lancet. 1988 Aug 13;2(8607):349-60. [PMID 2899772]
- Andersen HR et al. A comparison of coronary angioplasty with fibrinolytic therapy in acute myocardial infarction. N Engl J Med. 2003 Aug 21;349(8):733-42. [PMID 12930925]
- Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003 Jan 4;361(9351):13-20. [PMID 12517460]
- Morice MC et al. A randomized comparison of a sirolimus-eluting stent with a standard stent for coronaryrevascularization. N Engl J Med. 2002 Jun 6;346(23):1773-80. [PMID 12050336]
- Di Mario C et al. Immediate angioplasty versus standard therapy with rescue angioplasty after thrombolysis in the Combined Abciximab REteplase Stent Study in Acute Myocardial Infarction (CARESS-in-AMI): an open, prospective, randomised, multicentre trial. Lancet. 2008 Feb 16;371(9612):559-68. [PMID 18280326]
- EPIC Investigators. Use of a monoclonal antibody directed against the platelet glycoprotein IIb/IIIa receptor in high-risk coronary angioplasty. N Engl J Med. 1994 Apr 7;330(14):956-61. [PMID 8121459]
- Randomised trial of intravenous atenolol among 16 027 cases of suspected acute myocardial infarction: ISIS-1. First International Study of Infarct Survival Collaborative Group. Lancet. 1986 Jul 12;2(8498):57-66. [PMID 2873379]
- Magnesium in Coronaries (MAGIC) Trial Investigators. Early administration of intravenous magnesium to high-risk patients with acute myocardial infarction in the Magnesium in Coronaries (MAGIC) Trial: a randomised controlled trial. Lancet. 2002 Oct 19;360(9341):1189-96. [PMID 12401244]
- (PRISM-PLUS) Study Investigators. Inhibition of the platelet glycoprotein IIb/IIIa receptor with tirofiban in unstable angina and non-Q-wave myocardial infarction. N Engl J Med. 1998 May 21;338(21):1488-97. [PMID 9599103]
- Petersen JL et al. Efficacy and bleeding complications among patients randomized to enoxaparin or unfractionated heparin for antithrombin therapy in non-ST-Segment elevation acute coronary syndromes: a systematic overview. JAMA. 2004 Jul 7;292(1):89-96. [PMID 15238596]
- Yusuf S et al. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med. 2001 Aug 16;345(7):494-502. [PMID 11519503]

Critical Care
Compendium
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC