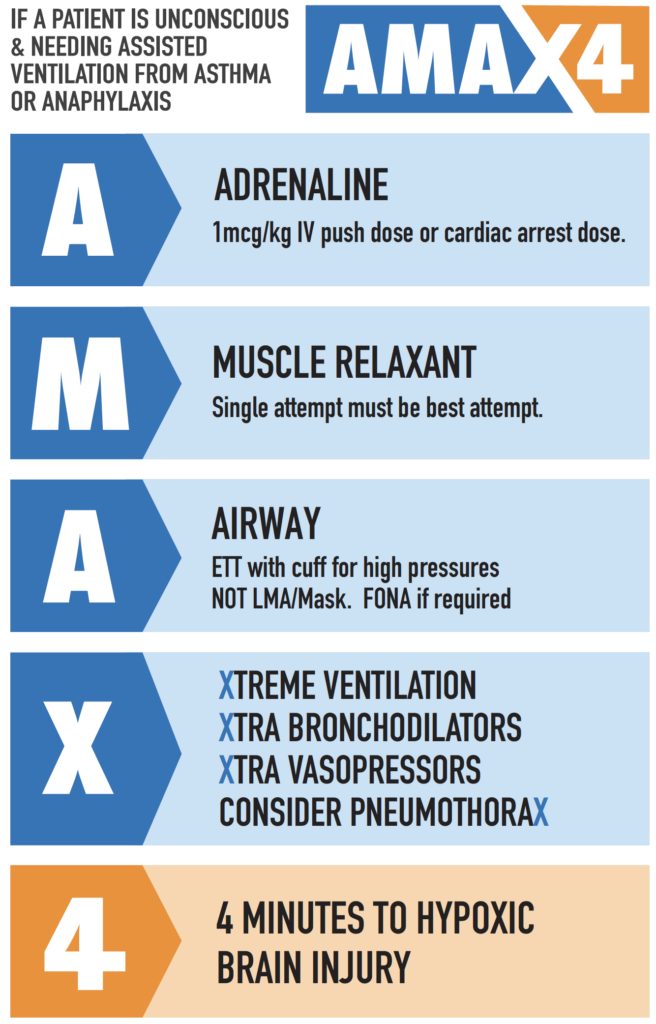
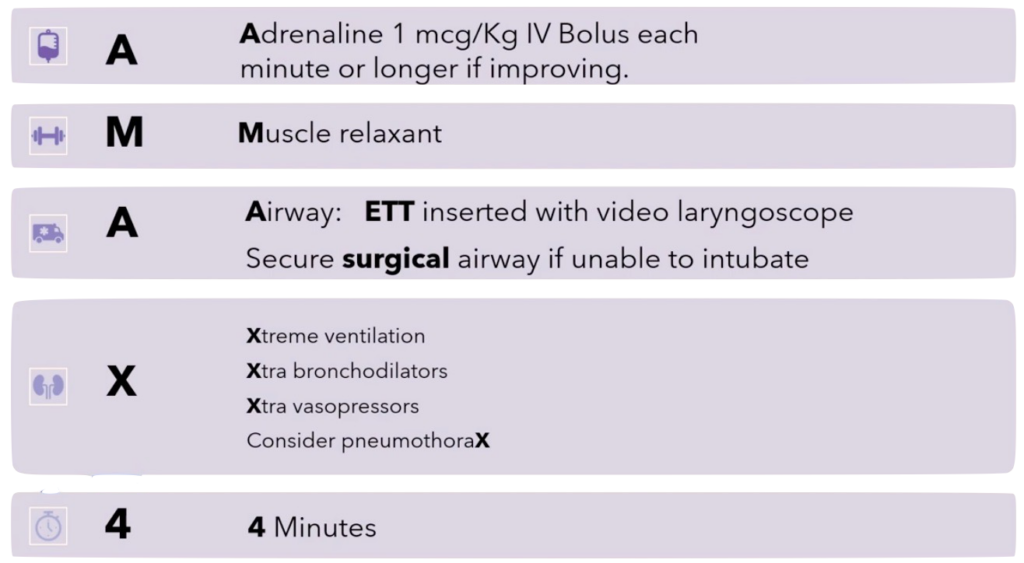
AMAX4 Algorithm
AMAX4 is an algorithm for critical care clinicians in anaphylaxis and asthma resuscitation.
The aim of this didactic approach is to reduce deaths from anaphylaxis and asthma by maintaining standards in emergency medicine and prehospital care.
What is anaphylaxis?
Anaphylaxis Definition (World Allergy Organisation 2020)
Either 1 or 2:
- Acute onset laryngeal involvement, bronchospasm or hypotension after exposure to a known or highly probable allergen for that patient (minutes to several hours) even in the absence of skin symptoms.
- Acute onset of an illness (minutes to several hours) with simultaneous involvement of skin, mucosal tissue, or both
AND at least one of the following
- Respiratory compromise (dyspnoea, wheeze-bronchospasm, stridor, hypoaxemia
- Reduced BP or associated symptoms of end organ hypoperfusion (eg hypotonia, syncope, incontinence)
- Severe GI symptoms (e.g. severe crampy abdominal pain, repetitive vomiting, especially after exposure to non-food allergens
Most young people with anaphylaxis die from bronchospasm – especially food allergy which is the most common trigger presenting to emergency departments. Bronchospasm also occurs in drug and venom allergy and causes death in young people.
Australia has the highest rates of documented food allergy and hospital anaphylaxis admissions in the developed world.
Severe anaphylaxis is an extremely challenging clinical scenario for even the most skilled clinicians and requires rapid escalation of potentially life-saving measures.
What is the AMAX4 algorithm?
AMAX4 is the initiative of emergency physician Dr Ben McKenzie and his wife Tamara McKenzie following the tragic death of their 15-year-old son Max McKenzie. Max sustained an hypoxic brain injury secondary to food anaphylaxis related bronchospasm/asthma.
The promotion of the AMAX4 algorithm aims to raise awareness and reform treatment through a didactic protocol to reduce deaths from anaphylaxis and asthma in young people to zero.
- Every emergency department should have programs where brief in situ practice of time critical team based procedures are practiced.
- Every ambulance service should have mechanisms in place to manage hypoxic asthma arrests and respond to potential rapid deterioration of acute asthma/ anaphylaxis.
The AMAX4 Algorithm
The AMAX4 algorithm applies to all clinicians who are capable of endotracheal intubation or are part of an intubating team. Non intubating clinicians need to understand that it is unknown how long bag valve mask ventilation can oxygenate someone with critical asthma/anaphylaxis or severe airway obstruction before it fails. The most senior person needs to devote every effort to deliver oxygen – a two person technique may help.
The 10 concepts informing AMAX4
Note: The 10 concepts are presented here in brief; they are expanded upon in the AMAX4 lecture on the AMAX4 website.
- Time to hypoxic brain injury is 4 minutes. The time to hypoxic brain injury is extremely short and cannot be extended by CPR in hypoxic arrest.
- Airway pressures are HIGH (50-100 cmH20) – too high for any other device other than an endotracheal tube (ETT). BVM and LMA are unsuitable.
- Immediately securing airway with ETT has multiple other benefits. Aspiration risk is high and consequences catastrophic.
- The FIRST intubation attempt should be the BEST attempt. Muscle relaxant, video laryngoscopy, and best intubator in the room.
- Inability to intubate on first attempt (Can’t Intubate, Can’t Oxygenate (CICO)) indicates immediate surgical airway.
- Secure the airway! Prioritise oxygen delivery to prevent brain damage.
- Intubation practice. Practice. Simulation. Practice
- PneumothoraX. Pneumothorax rates are high when arrest or CPR is involved.
- Xtreme Ventilation. Initially use a bag, not a ventilator.
- Xtra medical therapy.
If unconscious needing assisted ventilation from asthma or anaphylaxis consider the following:
The AMAX4 website
Ben and Tamara have launched a website AMAX4 – Every Second Counts which includes full details of the AMAX4 algorithm.
AMAX4 lecture
The site includes a full one hour lecture presented by Dr. Ben McKenzie and has been divided into 6 easily digestible 10 minute sections.
- Paediatric anaphylaxis, diagnostic criteria, severity grading system: Acute allergy is a continuum of disease from mild skin symptoms to cardiac arrest.
- Anaphylaxis treatment from basics to critical care specialist management before arrest. Ben tells the tragic story of James Tsindos who died 8 weeks before Max suffering an almost identical series of problems in care.
- Key anaphylaxis and asthma resuscitation concepts that are a “special circumstance
- The “Maximum 4 minutes” until hypoxic ischaemic encephalopathy, the first of 10 concepts informing AMAX4. The impact of time critical care, and the concept of “Hard deck, Hard limits“.
- Discussion of the remaining 9 of 10 concepts informing AMAX4
- Ben talks about what happened to Max with a deeper understanding of the timeline of Max’s care with paramedics and the Emergency Department.
Max’s Story
Max McKenzie was an otherwise healthy teenager. He was talented, happy and loved. Max entered health care with normal oxygen levels alert and he was able to ask for help, but despite the emergency health care provided sustained an unsurvivable brain injury.
Simulation Training Video
Simulation Video applying the techniques in a real-time, simulation of treating hypoxic anaphylaxis and asthma.
Every emergency department should have programs where brief in situ practice of time critical team based procedures are practiced – especially if the case mix of high acuity patients is low in a particular department.
Understand the medical adjuncts, risk of obstructive hyperinflation, risk of pneumothorax and how to perform difficult ventilation in the face of high pressures and an obstructive pattern using a laerdal bag post intubation.
Drawing up push dose adrenaline (epinephrine)
How to PREPARE and LABEL adrenaline (epinephrine) for a bolus push dose of 1 mcg/kg in order to have solutions of 100mcg/mL or for smaller children 10mcg/mL
A single large 10mL vial of 1:10,000 contains 1 mg/10mL adrenaline.
- In a 10mL syringe: Each 1mL has 100 mcg of adrenaline (100 mcg/mL)
A single small 1mL vial of 1:1,000 contains 1 mg/1 mL adrenaline (1000 mcg/mL)
- This can be diluted with 9mL of normal saline or water for injection to make a solution of 1mg/10mL
- In a 10mL syringe: Each 1mL has 100 mcg of adrenaline
For smaller children it is safer to make a solution of 10 mcg/mL
- To make this solution: Take 1 mL of a 1:10,000 solution and make it up to 10mL with 9mL of water for injection or normal saline.
- 10mL syringe: Each 1 mL contains 10 mcg of adrenaline (10mcg/mL)
Additional Resources
AMAX4
- AMAX4 Lanyard card [Download PDF]
- AMAX4 Algorithm
Allergy and Anaphylaxis
- Cardona V, Ansotegui IJ, Ebisawa M, El-Gamal Y, Fernandez Rivas M, Fineman S, Geller M, Gonzalez-Estrada A, Greenberger PA, Sanchez Borges M, Senna G, Sheikh A, Tanno LK, Thong BY, Turner PJ, Worm M. World allergy organization anaphylaxis guidance 2020. World Allergy Organ J. 2020 Oct 30;13(10):100472
Max McKenzie
- Interview with Ben & Tamara McKenzie
Martin Bromiley
- Just a Routine Operation with Martin Bromiley
- Lessons from the Bromiley Case. LITFL
FOAM review
- Morgenstern J. Critical anaphylaxis and asthma: The AMAX4 algorithm. First10EM
- Carly S. Just a routine resuscitation. The AMAX4 algorithm for anaphylaxis/asthma. St Emlyn’s
- Tagg A. A routine resuscitation. DFTB
[cite]
SMILE 2
Better Healthcare
Dr Neil Long BMBS FACEM FRCEM FRCPC. Emergency Physician at Kelowna hospital, British Columbia. Loves the misery of alpine climbing and working in austere environments (namely tertiary trauma centres). Supporter of FOAMed, lifelong education and trying to find that elusive peak performance.
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC

Hi Chris and Neill.
Such a sad case and very admirable that Ben and Tamara channel from this loss such an amazing effort to make it more of a never-event than it sadly is.
A point for discussion: I don’t think every place has access to 1:10.000 of adrenaline / epi (also, pet peeve, don’t like the 1:xx naming, it invites confusion and medication error). Teaching paeds stabilisation regularly I have often found that very few frontline staff have the training in place to be able to execute adrenaline dosing correctly in a paeds HALO situation like this.
My preference for making 10mcg/mL of adr/epi is to use the standard cardiac arrest solution of 1mg/mL and put 1 mL in a 100mL bag of NS which we, at least, have ubiquitously.
It saves trying to understand “1:10.000” labelling, and having to search for or first make up this 100mcg/mL solution. As such, it is consistently achievable in little time.
We use the 10mcg/mL often as push dose pressor when intubating critically ill adults so affords some familiarity from the day-to-day. It works beautifully if you have to make up cardiac arrest dose for the smaller child (1mL per kg) or the middle ground dosing for anaphylaxis (0.1mL per kg, drawn up in 1mL or 10mL syringe depending on the size of the child).
I realise different shops may become good at different approaches and Bens version will work well if drilled. I hesitate to muddy his messaging, but I believe this might generally have some merit at least outside purely paediatric settings where 95+% of uses of adrenaline will be for adults. This standard approach will be easily transferrable to the kid in extremis where mental bandwidth is limited. Working PICU / paeds anaesthesia I can’t remember when I last used “1:10.000”.
Thank you for writing this up and keeping LITFL the live index of sanity in medicine.