Autonomic Dysreflexia
Autonomic Dysreflexia (or autonomic hyperreflexia) is a condition of acute, uncontrolled reflex sympathetic output that may occur in patients with spinal cord injury, generally at or above the level of the major splanchnic outflow—i.e., above the level of T6.
The condition leads to episodes of severe hypertension, which may occasionally have lethal consequences.
Awareness and a high index of suspicion for the condition is crucial in any patient with spinal cord injury, particularly those with lesions at or above T6.
Outcome is good if the condition is recognised and managed promptly.
Treatment is directed at controlling the hypertensive response and correcting the underlying precipitating cause.
Pathophysiology
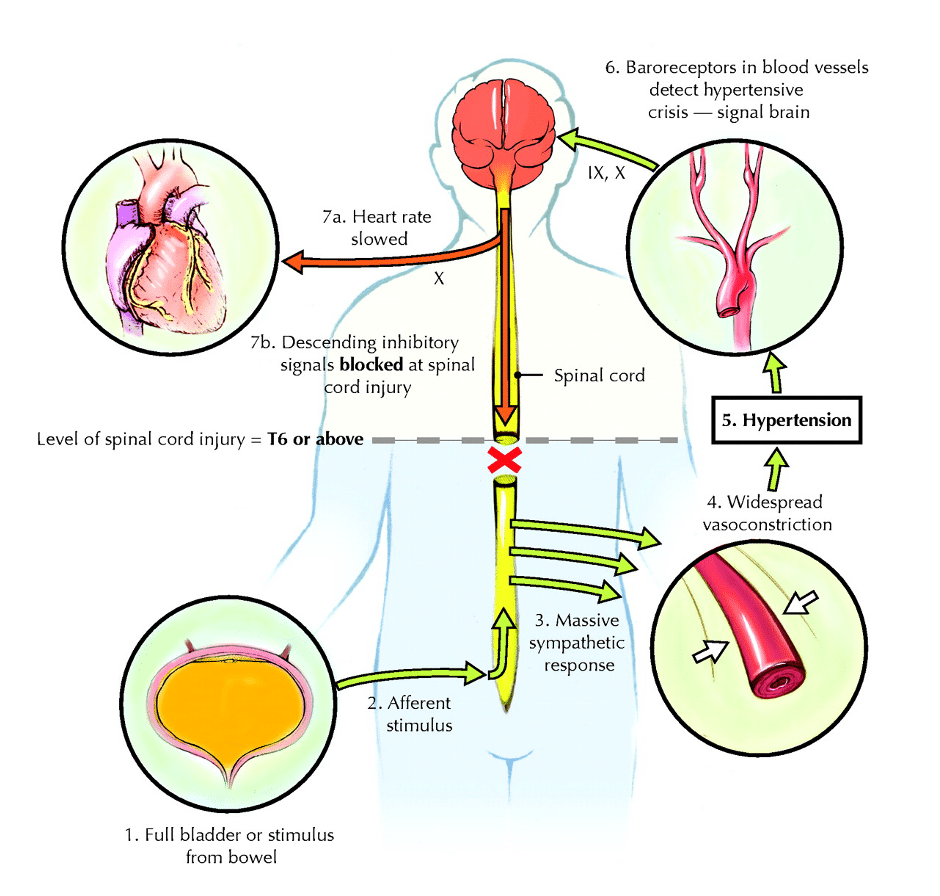
Autonomic dysreflexia results from local spinal reflex mechanisms that remain intact despite the injury, leading to unmodulated sympathetic responses—most importantly in the form of acute hypertension.
It is more common in patients with complete lesions than in those with incomplete lesions, and the reaction tends to be less severe in the latter group.
Mechanism
- A noxious stimulus below the level of the lesion produces afferent nerve impulses, triggering a generalised local spinal sympathetic reflex.
- This results in strong and widespread vasoconstriction below the level of the neurologic lesion.
- In lesions at or above T6, the splanchnic vascular bed becomes involved, providing a critical mass of blood vessels capable of producing a significant systemic elevation in blood pressure.
- The elevated blood pressure is detected by carotid and aortic baroreceptors. However, in a patient with spinal cord injury, descending inhibitory pathways are blocked, preventing modulation of the sympathetic response.
- The result is unrestricted peripheral and splanchnic vasoconstriction and generalised systemic hypertension.
- Reflex parasympathetic output (via an intact vagus nerve) causes peripheral vasodilation above the lesion, contributing to headache, flushing, sweating in the head and neck, nasal congestion, and bradycardia. However, this parasympathetic response is insufficient to counteract the hypertension.
- On rare occasions, autonomic dysreflexia may occur in patients with lesions below T6, but reactions tend to be milder.
Complications
The most serious complications arise from sustained, severe peripheral hypertension, and include:
- Retinal haemorrhages
- Hypertensive encephalopathies:
- Confusion
- Seizures
- Coma
- Cerebral haemorrhages
- Acute coronary syndromes
- Neurogenic pulmonary oedema
Fortunately, mortality is rare.
Precipitating Factors
Any noxious stimulus below the level of injury can trigger autonomic dysreflexia. The most common trigger is lower urinary tract stimulation.
Urinary tract causes
- Bladder distension (most common cause):
- Blocked IDC
- Insufficient frequency of intermittent catheterisation
- Bladder infection
- Instrumentation (e.g., catheterisation)
- Kidney stones
Gastrointestinal (GIT)
- Constipation (second most common cause)
- Distension from any cause
- Painful perianal conditions
- Acute intra-abdominal inflammatory conditions
Skin
- Cellulitis
- Infected pressure sores
- Skin infections (e.g., ingrown toenails)
Trauma
- Fractures
- Dislocations
Reproductive
- Labour and delivery
- Testicular pathology (epididymo-orchitis, torsion)
- Sexual activity
Vascular
- Deep vein thrombosis (DVT)
- Pulmonary embolism (PE)
Medications
- Sympathomimetic agents
Clinical Assessment
Features of the reaction
- Headache
- Blurred vision
- Anxiety
- Hypertension (hallmark feature):
- Normal BP in these patients is typically 90/60–100/60 mmHg lying (lower when sitting).
- 130/90 mmHg is considered abnormal.
- Untreated BP can rise rapidly to levels like 220/140 mmHg.
- Reflex vagal effects:
- Bradycardia (sometimes tachycardia if sympathetic effects predominate)
- Flushed, sweaty skin above the lesion
- Cool, pale skin below the lesion (due to sympathetic vasoconstriction)
Note: Patients may not feel the noxious stimulus but can often identify the cause based on prior experience.
Investigations
Autonomic dysreflexia is a clinical diagnosis; investigations focus on identifying the precipitating cause.
Blood tests
- FBE
- CRP
- U&Es / glucose
- LFTs
- Lipase
Urine
- Microscopy and culture
Imaging
- CXR / AXR (for faecal impaction, obstruction, perforation)
- X-rays (if trauma suspected)
- Bladder scan (to check for urinary retention)
- CT abdomen/pelvis (for unsuspected intra-abdominal pathology)
Management
Early recognition is key to avoiding life-threatening hypertension.
Goals
- Control hypertension
- Correct the precipitating cause
Management of Hypertension
First aid
- Sit the patient as upright as possible (orthostatic BP drop)
- Remove compression stockings
- Loosen tight clothing
Monitor BP closely.
Pharmacologic treatment (for systolic BP > 170 mmHg)
- GTN (glyceryl trinitrate):
- Sublingual GTN, repeat after 5 min if needed
- Onset: 2–3 min; duration: up to 30 min
- Transdermal GTN 5 mg patch for prolonged response
- In refractory cases: GTN or nitroprusside infusion
- Avoid GTN if patient has used sildenafil (Viagra) or vardenafil (Levitra) in the past 24 hrs, or tadalafil (Cialis) in the past 4 days.
- Nifedipine:
- Useful alone or with GTN
- 10 mg orally, crushed, mixed with water
Avoid sildenafil, vardenafil, or tadalafil for at least 48 hrs after a severe episode.
Management of Precipitating Factors
General principles
- Check IDC for obstruction; irrigate if needed.
- If no IDC, perform intermittent catheterisation.
- Check for faecal impaction; perform gentle disimpaction with anaesthetic gel.
- If symptoms persist, search for other causes (UTI, intra-abdominal sepsis) and treat accordingly.
References
Publications
- Blackmer J. Rehabilitation medicine: 1. Autonomic dysreflexia. CMAJ. 2003 Oct 28;169(9):931-5.
FOAMed
- Nickson C. Abdominal aortic aneurysm (AAA). LITFL
- Hartung MP. Abdominal CT: aortic aneurysm. LITFL
- Lobo V. POCUS: Abdominal aorta. LITFL
- Lam L. CT Case 084. LITFL
- Nazerian P. Aortic Dissection Detection Risk Score (ADD-RS). MDCalc
Fellowship Notes
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner
Educator, magister, munus exemplar, dicata in agro subitis medicina et discrimine cura | FFS |


