Bedside Echo in Pulmonary Embolism
aka Cardiovascular Curveball 011
A 35 year-old female is brought to the emergency department after collapsing in a shopping centre. Paramedics found her to be GCS 3 and shortly afterwards required CPR and 1mg adrenaline for profound bradycardia and no pulse. Spontaneous output returned and no further drugs have been required to support her circulation.
She remains intubated and GCS 3. There is little other history, except some information from a friend stating she had been on a trip to South America recently.
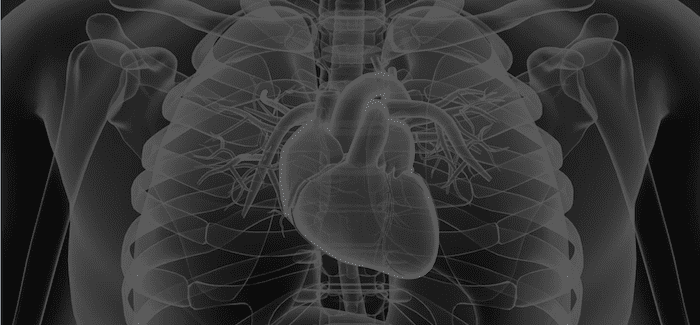
You perform a quick bedside echo while the paramedics are changing over their monitoring.
Q1. What are the obvious abnormalities on this echo?
Curveball Answer
- Small LV cavity size with normal LV systolic function
- Septal flattening consistent with RV pressure overload
- Severely dilated RV with severely reduced systolic function
Q2. What is McConnell sign?
Curveball Answer
Echocardiographic pattern of RV dysfunction consisting of akinesia of the mid free wall but normal motion at the apex
77% sensitivity and 94% specificity for diagnosis of pulmonary embolism
- Rippey J. Ultrasound Case 079. LITFL
Q3. What are the echocardiographic features of RV dysfunction in PE?
Curveball Answer
- RV wall hypokinesis
- Moderate or severe
- McConnell’s sign
- RV dilatation
- End-diastolic diameter >30 mm in parastemal view
- RV larger than LV in sobcostal or apical view
- Increased tricuspid velocity >26 m/sec
- Paradoxical RV septal systolic motion
- Pulmonary artery hypertension
- Pulmonary artery systolic pressure >30 mmHg
- Dilated IVC with lack of respiratory collapse
Other echocardiographic features associated with increased mortality include patent foramen ovale and free-floating right-heart thrombus.
Q4. What are the indications for thrombolysis in acute pulmonary embolism?
Curveball Answer
Fibrinolysis in acute pulmonary embolism remains a controversial topic.
Most agree that cardiac arrest and haemodynamic instability (SBP < 90mmHg) are indications for thrombolysis.
Controversy surrounds thrombolysis for stable patients with RV dysfunction on echocardiography.
- Treatment in this group has been shown to decrease pulmonary artery pressure and improve RV systolic function and pulmonary perfusion
- This benefit must be weighed against the risk of haemorrhage with thrombolytic therapy.
- Thrombolysis has not been shown to improve mortality
Other treatment algorithms include the use of elevated Troponin and BNP to select which patients require urgent echocardiography
In haemodynamically stable patients with RV dysfunction, thrombolysis should be considered on a case-by-case basis
Q5. What would you do next?
Curveball Answer
Administer thrombolysis
- Although stable at the moment, this patient has had a cardiac arrest from a pulmonary embolus and is potentially very unstable
- She has severe RV dysfunction on echocardiography
- There are no obvious contraindications to thrombolysis
- Alteplase 50mg IV bolus
Q6. What was the response to treatment?
Curveball Answer
This echo was performed a few hours later. Already some improvement in RV dysfunction is evident.
This case illustrates the utility of bedside echocardiography in the emergency department. Using the clinical history, a diagnosis of massive pulmonary embolism was made at the bedside and appropriate treatment could be administered almost immediately.
The pictures are from a real case, with some of the details changed. Let’s just say that thrombolysis makes failed intubation interesting
References
- Rippey J. LITFL Ultrasound Case 079.
- McConnell MV, Solomon SD, Rayan ME, Come PC, Goldhaber SZ, Lee RT. Regional right ventricular dysfunction detected by echocardiography in acute pulmonary embolism. Am J Cardiol. 1996; 78: 469–473.
- SB Oh, SJ Bang, MJ Kim. McConnell’s sign; a distinctive echocardiographic finding for diagnosing acute pulmonary embolism in emergency department. Crit Ultrasound J. 2015; 7(Suppl 1): A20.
- Fengler BT, Brady WJ (2009) Fibrinolytic Therapy in Pulmonary Embolism: an Evidence Based Algorithm. American Journal of Emergency Medicine. 27 84-89 [PMID 19041539]
- Roy P et al (2005) Systematic Review and Meta-Analysis of Strategies for the Diagnosis of Suspected Pulmonary Embolism. BMJ 331:259 [PMID 16052017]
- Goldhaber S (2002) Echocardiography in the Management of Pulmonary Embolism. Annals of Internal Medicine. 136:691-700 [PMID 11992305]
CLINICAL CASES
Cardiovascular Curveball
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
