Blunt Abdominal Trauma: Decision Making
aka Trauma Tribulation 023
You can only stomach so much. Whether it’s a kick, punch, baseball bat, cricket bat, hammer, fall or car crash, there are big decisions to make in the emergency management of blunt trauma. Here are 3 scenarios designed to find out whether you know when to send your patient straight to the OT, to the scanner or to hold FAST and watch and wait…
Patient 1 — Isolated blunt abdominal trauma
A rugby league player is brought in by ambulance. He was the minced meat in a wholemeal sandwich when he was crash tackled by two opposing players as he dived for the try line. He’s in a lot of pain and points at his abdomen. To make matters worse, he fumbled over the line and his team lost. Ouch.
Questions
Q1. What are the indications for emergency laparotomy in blunt abdominal trauma?
Answer and interpretation
These:
- Peritonism
- Free air under the diaphragm
- Significant gastrointestinal hemorrhage
- Hypotension with positive FAST scan or positive DPL
FAST = Focused Assessment with Sonography in Trauma
DPL = Diagnostic Peritoneal Lavage
Your league playing patient doesn’t have any of these indications at present… Mind you he hasn’t had any investigations yet. Your next decision depends on whether he is haemodynamically stable or not.
Q2. What is your approach if he is haemodynamically unstable?
Answer and interpretation
Commence hemostatic resuscitation and look for causes of hemorrhage and shock, starting with intraperitoneal haemorrhage.
Perform FAST scan (or DPL if ultrasound is not available)
If positive the patient needs an emergency laparotomy. If negative… see Q3!
Q3. What is your approach if the patient is haemodynamically unstable but the FAST scan is negative?
Answer and interpretation
Continue haemostatic resuscitation while seeking and treating other causes of hemorrhage and shock.
Diagnostic peritoneal aspiration (DPA) can be performed following a negative FAST scan in the setting of blunt abdominal trauma. A positive DPA is suggested by the aspiration of frank blood — lavage is not performed.
If the DPA is positive the patient needs:
- emergency laparotomy
If the DPA is negative then:
- Other causes of hemorrhage are likely (i.e. extra-abdominal), or non-hemorrhagic causes of hypotension.
- The six sites of bleeding to consider are: scalp and external, chest, abdomen, long bones, pelvis and retroperitoneal (SCALPeR)
However, patients who are FAST negative DPA negative following blunt abdominal trauma may still have a significant intraperitoneal injury.
- Serial examination of the abdomen and serial FAST scans should be performed in case of an evolving injury.
- If the patient stabilizes a CT abdomen with IV contrast will help determine the presence of a significant intraperitioneal organ injury retroperitoneal injury, which may also necessitate operative intervention or interventional radiology.
Q4. What is your approach if he is haemodynamically stable?
Answer and interpretation
Options include:
- Serial physical examinations +/- FAST scans and observation
- CT abdomen with IV contrast (DPL is an alternative if CT abdomen is not available)
The choice depends on various factors:
- Availability of imaging
- Availability of experienced staff to perform serial examinations
- Patient preference following informed consent
- Presence of other indications for definitive imaging e.g. seat belt sign, suspected retroperitoneal injury, etc.
Q5. Why is diagnostic peritoneal lavage (DPL) suggested as an alternative to CT abdomen rather than ultrasound, if CT is unavailable?
Answer and interpretation
The CT abdomen is primarily used in a haemodynamically stable to identify intraperitoneal injuries in the absence of significant hemorrhage. FAST scan can detect 250 mL of intraperitoneal free fluid, depending on the operator. As such it is useful for identifying significant intraperitoneal hemorrhage. However, ultrasound is not reliable for identifying specific organ injuries or minor hemorrhage.
DPL, although it cannot identify specific organ injuries, can detect:
- minor intraperitoneal hemorrhage
- ruptured viscus (e.g. intraperitoneal contamination with gastrointestinal contents)
Things can be trickier in the real world of course, as patients may inconveniently have major injuries at other sites in addition to blunt abdominal trauma…
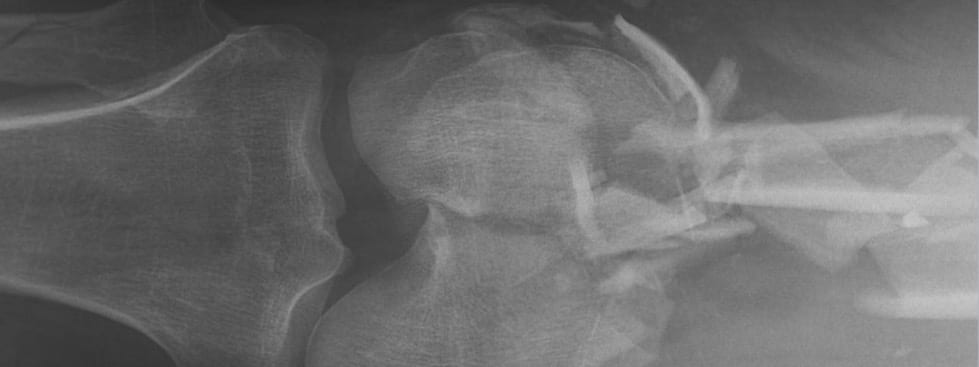
Patient 2 — Blunt abdominal trauma and pelvic fracture
A bull rider got bucked off and stomped on at the local rodeo. In addition to a suspected intrabdominal injury from blunt abdominal trauma, his pelvic bones felt wobbly on palpation suggesting that he has a pelvic fracture.
Again, the key issue is whether or not he is haemodynamically stable.
Q6. What is your approach if he is haemodynamically unstable?
Answer and interpretation
The key question is to determine whether there is significant intraperitoneal hemorrhage.
Again, commence haemostatic resuscitation and look for causes of hemorrhage and shock, starting with intraperitoneal hemorrhage.
- A pelvic binder should also be applied.
Perform FAST scan (or DPL if ultrasound is not available).
- If positive the patient needs an emergency laparotomy.
If the FAST scan is negative, DPA can be performed, but the site of aspiration should be above the umbilicus. A positive result is frank blood (RBCs on microscopy is not sufficient).
- If positive, this indicates a false negative FAST scan and the need for emergency laparotomy
If the FAST scan and DPA are negative then the pelvic fractures are the likely cause of hemorrhage and hemodynamic instability. As a result, the patient requires :
- angiography and pelvic stabilization
Following this, the approach is then similar to that of hemodynamically stable patient as described below.
Q7. What is your approach if he is hemodynamically stable?
Answer and interpretation
He could still have a significant intraperitoneal injury.
- A CT abdomen with IV contrast is indicated to determine the presence of intraperitioneal organ injury, which may also necessitate laparotomy. DPL is an alternative if CT abdomen is not available.
If no significant intraperitioneal organ injury is present then the patient can undergo definitive treatment of his pelvic fractures (e.g. angiography and/or pelvic stabilization).
Patient 3 — Blunt abdominal trauma and severe traumatic brain injury
A cyclist came off his bike at speed when a ‘road train’ passed him a tad too close. Apart from having handle bars rammed into his abdomen, he smacked his helmeted head hard and has a GCS of 7.
Q8. What are your immediate priorities?
Answer and interpretation
- Airway maintenance ( avoid hypoxia)
- Management of intracranial pressure
- Hemostatic resuscitation (avoid hypotension, correct coagulopathy)
- Detect correctable injuries (especially intracranial and abdominal injuries)
Q9. What is the role of permissive hypotension in this setting?
Answer and interpretation
There is no role for permissive hypotension in this setting.
Most experts advise a MAP of 70 mmHg in the presence of a severe traumatic brain injury (TBI) to maintain cerebral blood flow, given that the severely injured brain lacks cerebral autoregulation and intracranial pressure may be elevated.
Remember that cerebral perfusion pressure (CPP) = MAP – ICP)
Learn more about severe TBI in Trauma! Traumatic Brain Injury
Q11. What is your approach if the patient is hemodynamically unstable?
Answer and interpretation
There is little point resuscitating or operating on a brain dead patient.
Determine if there is significant intraperitoneal hemorrhage by performing FAST scan (or DPL if ultrasound is not available).
- If positive, the patient needs an emergency laparotomy
- If negative, the approach is similar to that of a haemodynamically stable patients (see Q12)
However, if the patient has lateralising signs then the patient either needs:
- a pre-laparotomy CT head (if CT is immediately available), or
- burr holes/ craniotomy at the same time as the laparotomy.
If lateralising signs are absent:
- the patient can go for a CT head after the emergency laparotomy.
Q12. What is your approach if the patient is haemodynamically stable?
Answer and interpretation
It depends on whether lateralising signs are present.
If lateralising signs are present then the patient needs:
- CT head and CT abdomen with IV contrast if CT is immediately available, or
- burr holes/ craniotomy prior to CT head and abdomen (if imaging is not readily available)
If lateralising signs are absent then the patient needs:
- CT head and CT abdomen with IV contrast
- ongoing management of intracranial pressure and supportive care.
Diagnostic peritoneal lavage is touted as an alternative option in settings where a CT abdomen is not available.
Q13. What are lateralising signs in severe traumatic brain injury?
Answer and interpretation
Lateralising signs in severe traumatic brain injury suggest the presence of a focal lesion (e.g. hematoma) that requires urgent decompression.They include:
- unilateral blown pupil (usually ipsilateral to the lesion)
- unilateral posturing or seizures (usually contralateral to the lesion)
References
- Fildes J, et al. Advanced Trauma Life Support Student Course Manual (8th edition), American College of Surgeons 2008.
- Legome E, Shockley LW. Trauma: A Comprehensive Emergency Medicine Approach, Cambridge University Press, 2011.
- Marx, JA. Blunt Abdominal Trauma: Priorities,Procedures, And Pragmatic Thinking. Emergency Medicine Practice; Vol 3(5) 2001. [link to fulltext pdf]
CLINICAL CASES
Trauma Tribulation
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
