Bouveret Syndrome
Bouveret syndrome is a rare variant of gallstone ileus, presenting as gastric outlet obstruction due to a large gallstone that has migrated through a biliogastric or bilioduodenal fistula, becoming lodged in the pylorus or proximal duodenum.
Epidemiology: Bouveret Syndrome primarily affects elderly females (F:M ~6:1) and accounts for 1–3% of gallstone ileus cases, which itself represents <0.5% of mechanical bowel obstructions. A preceding history of symptomatic gallstones is often absent, complicating diagnosis.
Pathogenesis: A cholecystoenteric fistula forms from chronic inflammation and erosion, allowing a large gallstone to pass into the duodenum or stomach. This may lodge at the pylorus or first part of the duodenum, leading to acute obstructive symptoms.
Clinical Features
- Nonspecific symptoms: Nausea, vomiting, epigastric pain, anorexia, and weight loss. May mimic peptic ulcer disease or malignancy.
- Features of gastric outlet obstruction
- Often preceded by a history of biliary colic or chronic cholelithiasis
Imaging
- CT scan is the modality of choice: visualizes gallstone, fistula, and signs of obstruction.
- Ultrasound and MRI may help identify the fistula and residual gallstones.
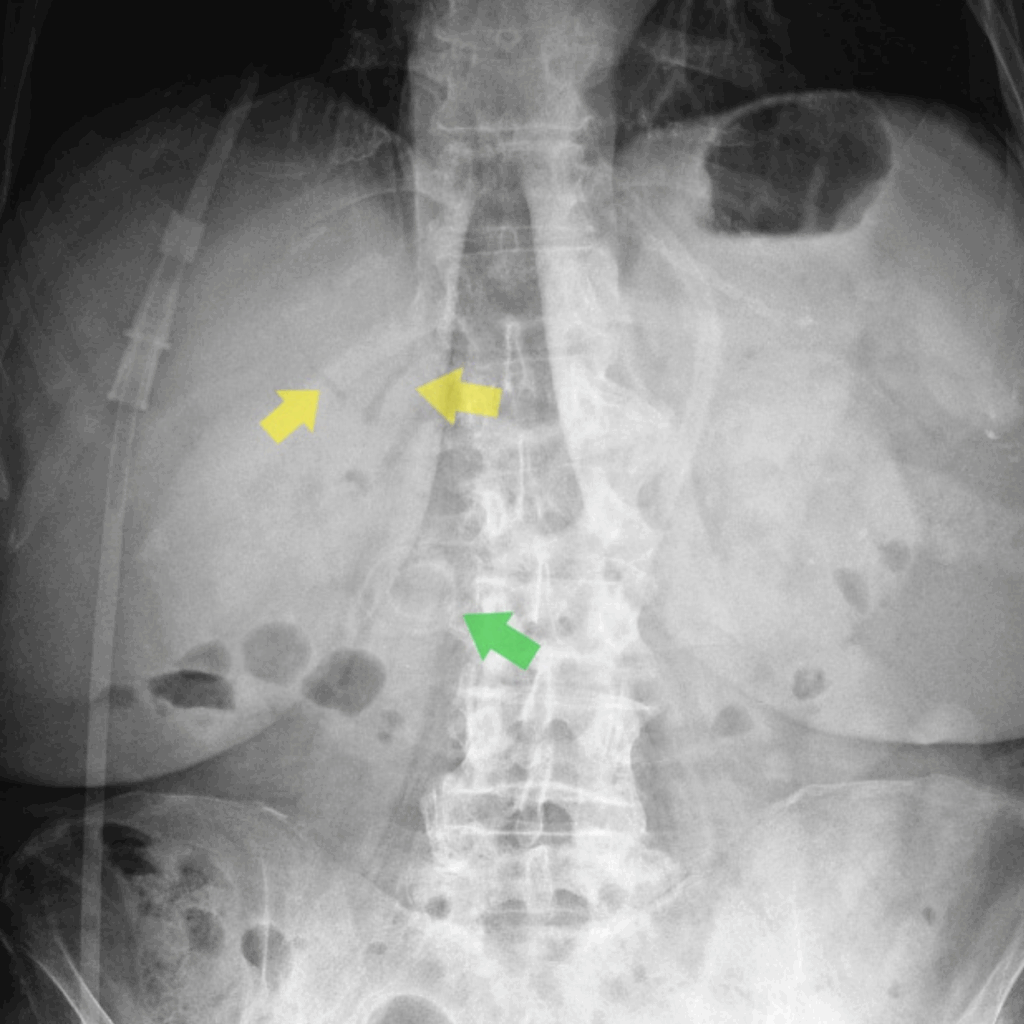
- Rigler’s Triad of pneumobilia, ectopic gallstone, and bowel obstruction) may be present (20-30%) though less commonly than in classic gallstone ileus
Management
- Endoscopic removal (mechanical, laser, or electrohydraulic lithotripsy) is first-line, especially in poor surgical candidates.
- Surgical options include enterolithotomy, cholecystectomy, and fistula repair, though often avoided in frail patients.
Prognosis: Mortality rates remain high (12–33%) due to advanced age and comorbidities. Prompt diagnosis and tailored intervention significantly influence outcomes.
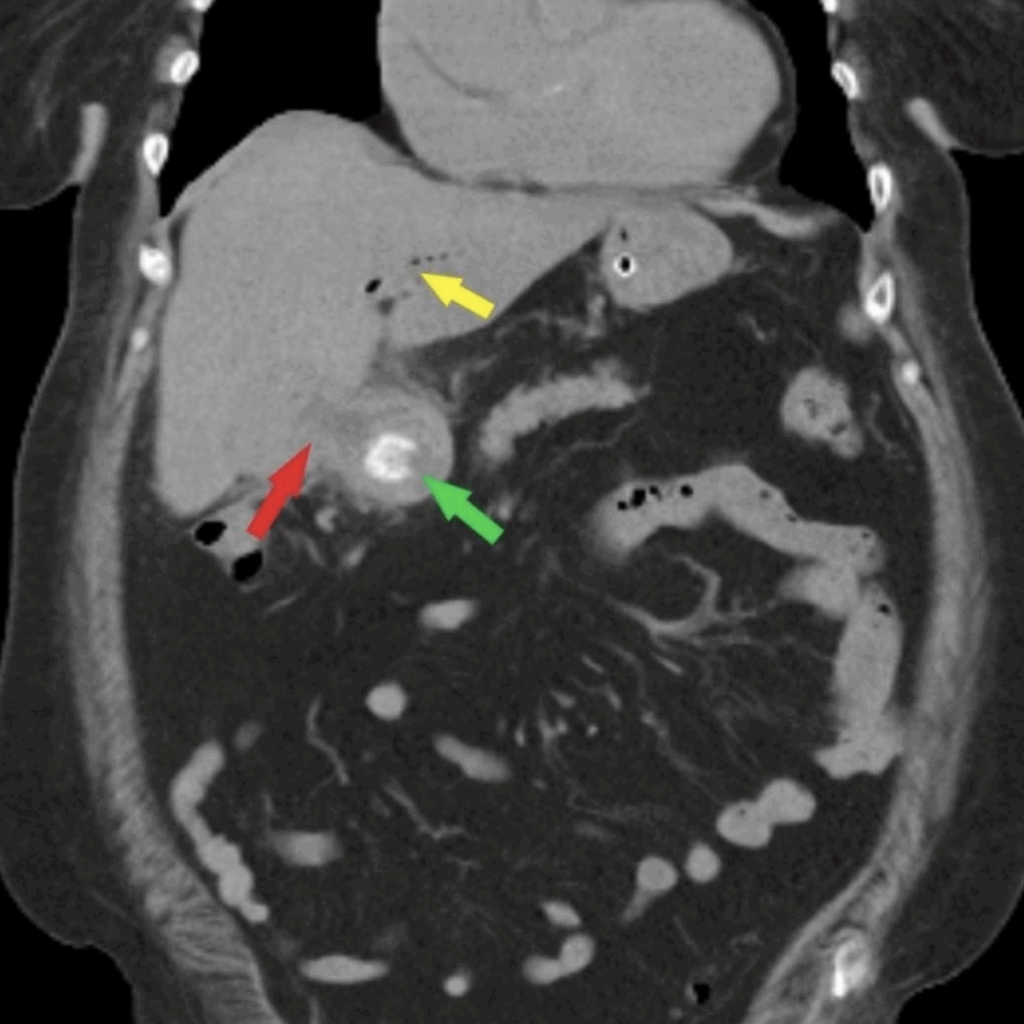
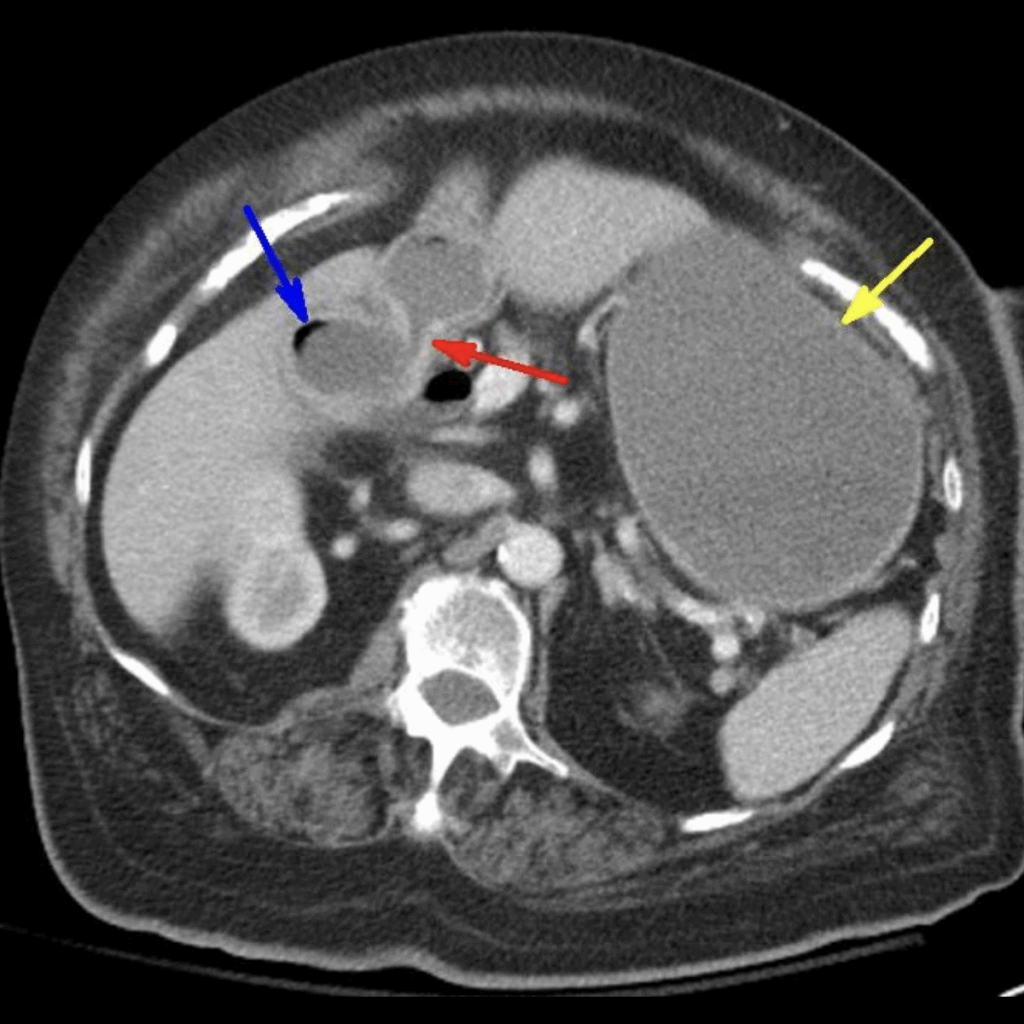
Case 2: Bouveret syndrome with Rigler’s triad: air within the gallbladder (blue arrow), cholecystoenteric fistula (red arrow) with ectopic gallstone in proximal duodenum, and gastric distention (yellow arrow). Radiopaedia
History of Bouveret Syndrome
1770 – M. Beaussier (France) documented a pathological fistulous communication between the gallbladder and the stomach with distal biliary obstruction. Although not described in modern clinical terms, this may represent the first anatomical description consistent with a biliogastric fistula. He observed this in a 60-year-old with no prior gastrointestinal symptoms, highlighting the silent evolution of the fistula.
La vésicule du fiel communique par son corps, avec l’orifice inférieur de l’estomac… Le canal cholédoque est plus long & plus épais qu’il ne doit être ; il se trouve obstrué vers l’extrémité où il entre dans le duodenum…
Il reste à savoir si l’oblitération de ce canal est naturelle, ou si quelque maladie n’a point ouvert la vésicule, peut-être déjà attachée à l’estomac ; c’est ce qu’aucune maladie ni aucun accident n’ont annoncé pendant le cours d’une vie de soixante ans. – Beaussier 1770
The gallbladder communicates directly with the lower orifice of the stomach… The common bile duct is longer and thicker than usual; it is obstructed near the point it enters the duodenum.
It remains to be determined whether the obliteration of this duct is natural, or whether some disease opened the gallbladder, perhaps already attached to the stomach. This is uncertain, as no illness or accident indicated such a condition during a 60-year lifetime. – Beaussier 1770
1841 – Auguste Bernard Bonnet (1791-1873) presented Observation No. 63 in Traité complet théorique et pratique des maladies du foie. A 60-year-old man with persistent vomiting, obstinate constipation, and cachexia, who died after a week of progressive gastric dysfunction.
At autopsy, a large biliary calculus (1 pouce 3 lignes × 1 pouce 2 lignes ≈ 3.6 × 3.3 cm) was discovered firmly impacted in the digestive tract, most likely the duodenum or pyloric region. The gallbladder was described as squirrheuse (fibrosed) with chronic suppuration of adjacent tissues, suggesting long-standing inflammation and a probable (though not explicitly visualized) spontaneous cholecystoenteric fistula.
A l’autopsie, on trouva les marques d’une violente gastro-entérite, et de plus un calcul biliaire, ayant un pouce trois lignes de hauteur et un pouce deux lignes de largeur. Ce calcul, engagé dans le tégument, l’oblitérait entièrement. La vésicule biliaire était squirrheuse ; le tissu cellulaire qui l’unissait au foie était le siège d’une suppuration chronique. Le malade dépérit rapidement avec vomissements fréquents… Bonnet 1841
At autopsy, we found intestinal inflammation and a large gallstone. This stone lodged in the passage, completely obliterated it. The gallbladder was squirrhous; the cellular tissue which united it to the liver was the site of chronic suppuration. The patient rapidly deteriorated with frequent vomiting… Bonnet 1841
1893 – In his textbook Traité des maladies de l’estomac, Léon Bouveret (1850-1929) described a case of pyloric obstruction secondary to a gallstone eroding through the gallbladder into the stomach.
1896 – Bouveret published a more detailed account of two personal cases, including clinical features, surgical findings, and pathological correlations. He linked the syndrome to earlier fistula-related complications of gallstones
❝La vésicule biliaire était fortement adhérente au pylore; le calcul, en traversant la paroi commune, avait pénétré dans le canal digestif et obstruait complètement la lumière duodénale.❞
Bouveret 1896
The gallbladder was firmly adherent to the pylorus; the stone, having passed through the shared wall, had entered the digestive tract and completely obstructed the duodenal lumen.
Associated Persons
- Auguste Bernard Bonnet (1791-1873)
- Léon Bouveret (1850-1929)
Controversies
The Identity and Priority of M. Beaussier (1770)
Beaussier is frequently cited as providing the earliest known account of gastric outlet obstruction due to a gallstone, reportedly in 1770. However, the figure remains historically obscure.
- Name Ambiguity: The prefix “M.” in his 1770 paper almost certainly refers to “Monsieur,” the customary title of respect at the time, rather than a first initial. His full name is not provided in the publication, nor is it currently known from biographical sources.
- Professional Background: In his introduction, Beaussier is identified as: “docteur en médecine et ancien chirurgien des camps et armées du roi” (Doctor of Medicine and former surgeon of the king’s camps and armies).
- Legacy Confusion: Beaussier is perhaps more widely known for a preceding article in the same journal volume on splenic artery aneurysm (SAA), frequently cited in vascular surgery literature as the first anatomical description of SAA on cadaveric dissection: Beaussier M. Sur une anévrisme de l’artère splénique dont les parois se sont ossifiées. Journal de médecine, chirurgie, pharmacie, &c. 1770; 32: 157-162.
- Obscure Contribution to Bouveret Syndrome: His case of gastric obstruction from a gallstone appears later in the same volume but lacks modern clinical terminology. It is mentioned in contemporary reviews but without direct textual citations or quotes, contributing to the confusion.
A. Bonnet Misattribution
The 1841 case often cited as the first clear medical description of what would become known as Bouveret syndrome is attributed to “Bonnet, A” though confusion persists over which Bonnet this refers to.
- Correct Author: The source is Auguste Bernard Bonnet (1791-1873), a surgeon based in Lyon, who included a case report in his treatise on liver diseases, Traité complet théorique et pratique des maladies du foie (1841).
- Incorrect Attribution: Many secondary sources have incorrectly credited the case to Amédée Bonnet (1809-1858), a better-known surgeon who was also based in Lyon and published widely on orthopedic and surgical topics. The similarity in name, profession, and location has led to frequent confusion.
- Lack of Journal Record: Some sources claim that Bonnet’s case appeared in the Archives générales de médecine, 1841, Tome 2, page 372 as Observation d’un calcul biliaire volumineux, adhérent à la portion pylorique de l’estomac et engagé dans l’intestin grêle. However, this appears to be bibliographically incorrect; no such article by either Bonnet appears in that volume or issue.
References
Historical references
- Beaussier. Autre observation. Journal de médecine, chirurgie, pharmacie, &c. 1770; 32: 163-165
- Bonnet A. Traité complet théorique et pratique des maladies du foie. 1841: 312-316
- Bouveret L. Traité des maladies de l’estomac, Paris: J.-B. Baillière 1893
- Bouveret L. Sténose du pylore adhérent à la vésicule calculeuse, Revue de médecine, Paris 1896; 16: 1-16
Eponymous term review
- Velasco Suarez C, Bazterrica E. Sindrome de Bouveret; a propésito de una nueva observacién. Archivos españoles de enfermedades del aparato digestivo y de la nutrición 1937; 13: 55-62
- Kosorok P. Bouveret’s syndrome (gallstone ileus)–a minefield. Br J Clin Pract. 1996 Jan-Feb;50(1):59-60
- Ariche A, Czeiger D, Gortzak Y, Shaked G, Shelef I, Levy I. Gastric outlet obstruction by gallstone: Bouveret syndrome. Scand J Gastroenterol. 2000 Jul;35(7):781-3.
- Cappell MS, Davis M. Characterization of Bouveret’s syndrome: a comprehensive review of 128 cases. Am J Gastroenterol. 2006 Sep;101(9):2139-46.
- Doycheva I, Limaye A, Suman A, Forsmark CE, Sultan S. Bouveret’s syndrome: case report and review of the literature. Gastroenterol Res Pract. 2009;2009:914951.
- Beuran M, Ivanov I, Venter MD. Gallstone ileus–clinical and therapeutic aspects. J Med Life. 2010 Oct-Dec;3(4):365-71
- Bruni SG, Pickup M, Thorpe D. Bouveret’s syndrome-a rare form of gallstone ileus causing death: appearance on post-mortem CT and MRI. BJR Case Rep. 2017 May 20;3(3):20170032.
- Caldwell KM, Lee SJ, Leggett PL, Bajwa KS, Mehta SS, Shah SK. Bouveret syndrome: current management strategies. Clin Exp Gastroenterol. 2018 Feb 15;11:69-75.
- Philipose J, Khan HM, Ahmed M, Idiculla PS, Andrawes S. Bouveret’s Syndrome. Cureus. 2019 Apr 9;11(4):e4414.
- Osman KT, Wahba A, Farhoud A, Abdelfattah AM, Maselli DB. Bouveret’s Syndrome: An Extensive Summary of the Literature. Arch Gastroenterol Res. 2020; 1(2): 40-46.
- Zheng B, Li C, Wang S. Cholecystogastric fistula presenting as pyloric obstruction: A rare case of Bouveret syndrome. Asian J Surg. 2022 Jan;45(1):635-636.
- Jin L, Naidu K. Bouveret syndrome-a rare form of gastric outlet obstruction. J Surg Case Rep. 2021 May 19;2021(5):rjab183
- Nasser HA, Ibrahim N, Nasser AA, Mendes VM, Zein M. Gastric outlet obstruction – looking for a syndrome: Bouveret or Mirizzi? Int J Surg Case Rep. 2021 Jul;84:106098.
- Turner AR, Kudaravalli P, Ahmad H. Bouveret Syndrome. 2021
- Bhandari TR, Wong JLH, Ahmad J, Akbari K, Menon V. Bouveret’s syndrome: An old diagnosis. A modern multimodality approach (endoscopic and robotic surgical) of gastric outlet obstruction: Report of two cases. Int J Surg Case Rep. 2024 Jan;114:109134.
- Greif EF. Bouveret syndrome. Radiopaedia
- Vaskov I. Bouveret syndrome. Radiopaedia
eponymictionary
the names behind the name
MbChB University of Bristol, UK. Currently working at Sir Charles Gairdner Hospital, Perth, Australia in emergency medicine.
BA MA (Oxon) MBChB (Edin) FACEM FFSEM. Emergency physician, Sir Charles Gairdner Hospital. Passion for rugby; medical history; medical education; and asynchronous learning #FOAMed evangelist. Co-founder and CTO of Life in the Fast lane | On Call: Principles and Protocol 4e| Eponyms | Books |

