Common Peroneal Nerve Lesions
Common peroneal nerve injury causes foot drop and sensory loss over the lateral leg and foot. Often due to trauma or compression near the fibular neck.
The common peroneal nerve provides:
- Motor innervation to the lateral compartment of the leg
- Sensory innervation to the lateral leg and dorsum of the foot
Injury typically results in foot drop due to loss of dorsiflexion.
Most vulnerable at the neck of the fibula, especially with tight plaster casts in this region — a common cause of neuropraxia.
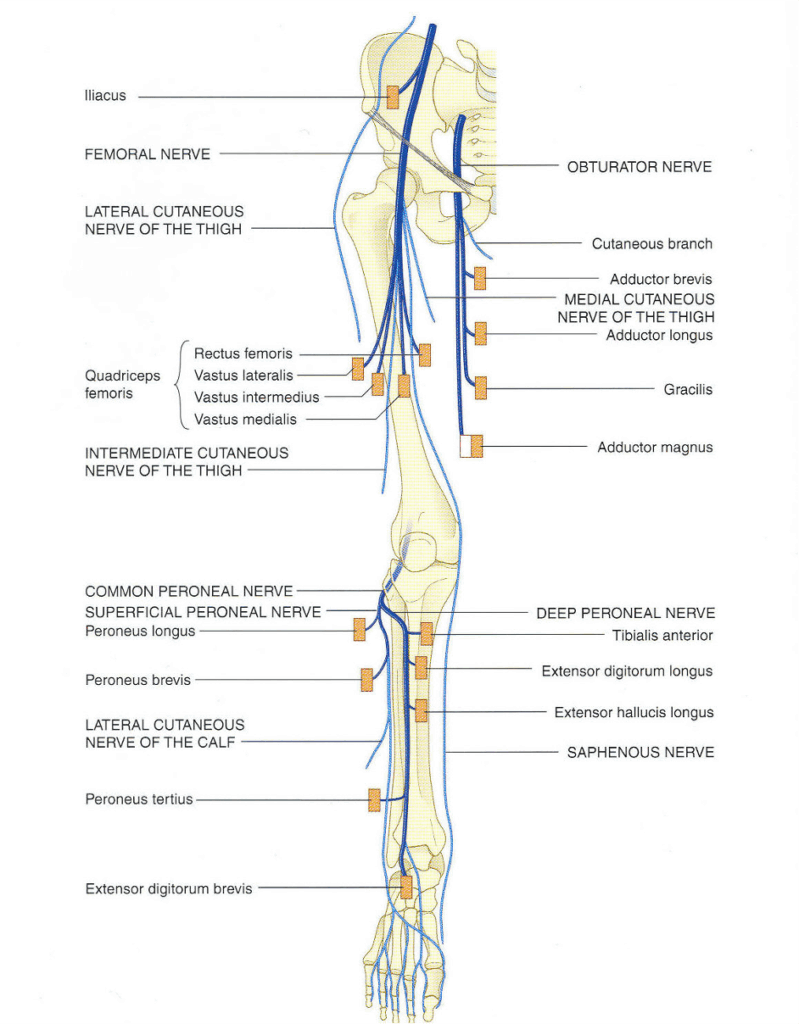
Anatomy
Course of the common peroneal nerve
- Originates with the tibial nerve from the sciatic nerve in the lower posterior thigh
- Runs along biceps femoris, wraps around the neck of the fibula
- Pierces peroneus longus and divides into:
- Superficial peroneal nerve
- Deep peroneal nerve
Superficial Peroneal Nerve
- Passes between peroneus longus and brevis, becomes superficial
- Crosses extensor retinaculum to the dorsum of the foot
Deep Peroneal Nerve
- Pierces anterior fascial septum, enters anterior compartment
- Descends deep to extensor digitorum longus
- Accompanies anterior tibial artery, enters foot deep to extensor retinacula
Innervations
Before division:
- Peroneal communicating nerve → joins medial sural cutaneous → sural nerve
- Lateral sural cutaneous nerve → skin of lateral leg
- Nerve to short head of biceps
- Articular branch to knee joint
Superficial Peroneal Nerve:
- Motor: Peroneus longus, Peroneus brevis
- Sensory: Dorsum/lateral foot, lateral 3½ toes
Deep Peroneal Nerve:
- Motor:
- Tibialis anterior
- Extensor digitorum longus
- Peroneus tertius
- Extensor hallucis longus
- Extensor digitorum brevis
- Sensory: Adjacent sides of first and second toes, branch to ankle joint
Pathology
Causes of Common Peroneal Nerve Lesions
- Trauma:
- Especially at fibular neck
- Risk with tight plaster casts
- Neuropraxia:
- Compartment syndrome of lateral compartment
- Mass lesions:
- Tumours
- Abscesses
- Neuropathies:
- Diabetes mellitus (ischemia)
- Malignancy (compression/paraneoplastic)
- Infective: Leprosy, HIV
- CTDs: RA, SLE, PAN, scleroderma, sarcoidosis
- Rare: Amyloidosis, Lyme disease, heavy metal poisoning
Clinical Assessment
Common finding is foot drop with weak eversion. Sensory loss may affect the dorsum of the foot and lateral leg depending on lesion location and severity.
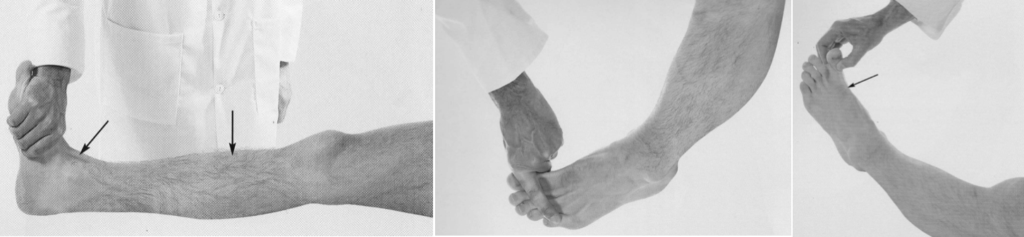
Middle: Extensor digitorum longus (Deep Peroneal Nerve, L5, S1). The patient dorsiflexes the toes against resistance. The tendons passing to the lateral four toes can be seen and felt.
Right: Extensor Hallucis Longus (Deep Peroneal Nerve). The patient dorsiflexes the distal phalanx of the big toe against resistance. The tendon (arrow) can be seen and feltdosriflexes the foot against resistance.
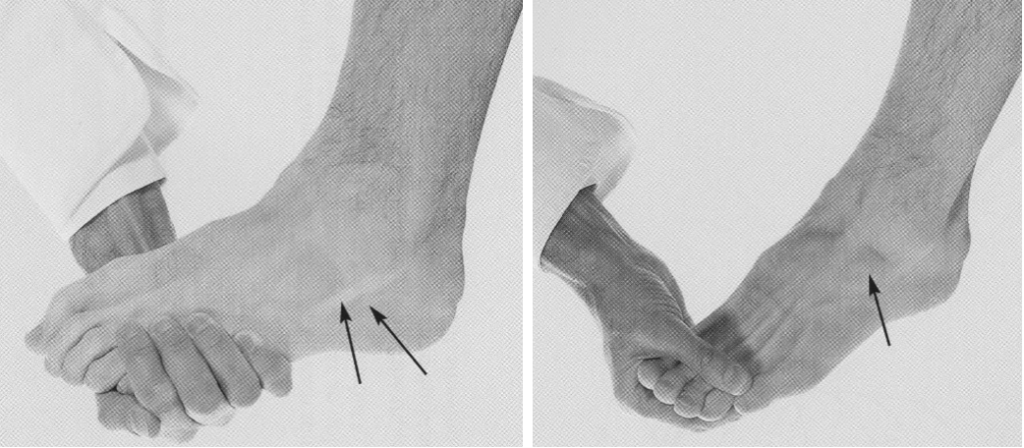
Right: Extensor digitorum Brevis (Deep Peroneal Nerve. The patient dorsiflexes the proximal phalanges against resistance. Arrow; the muscle belly can be felt and sometimes seen.
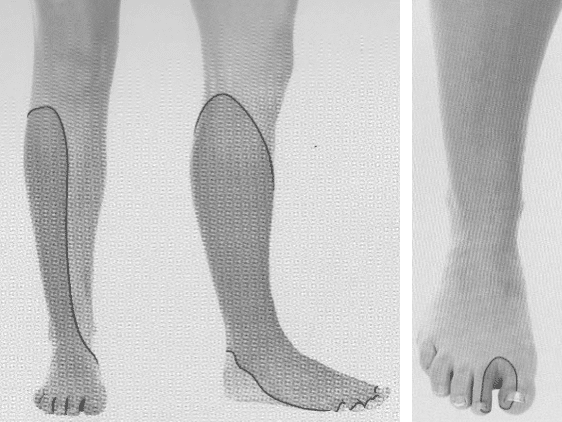
Right: The approximate area within which sensory changes may be found in lesions of the deep peroneal nerve
Investigations
Blood tests (based on clinical suspicion):
- FBC
- U&Es / Glucose
- CRP
- ESR
- Additional tests as indicated
Imaging:
- CT or MRI to evaluate mass lesions or assess nerve integrity
Management
- Treat underlying cause
- Neuropraxias:
- Fasciotomy if due to compartment syndrome
- Remove tight casts
- Occupational therapy:
- Assist with splinting, adaptive supports
- Physiotherapy:
- Promote recovery, prevent contractures or deformity
Disposition
Dependent on:
- Onset
- Cause
- Severity
Appendix 1
Common Peroneal Nerve Anatomy
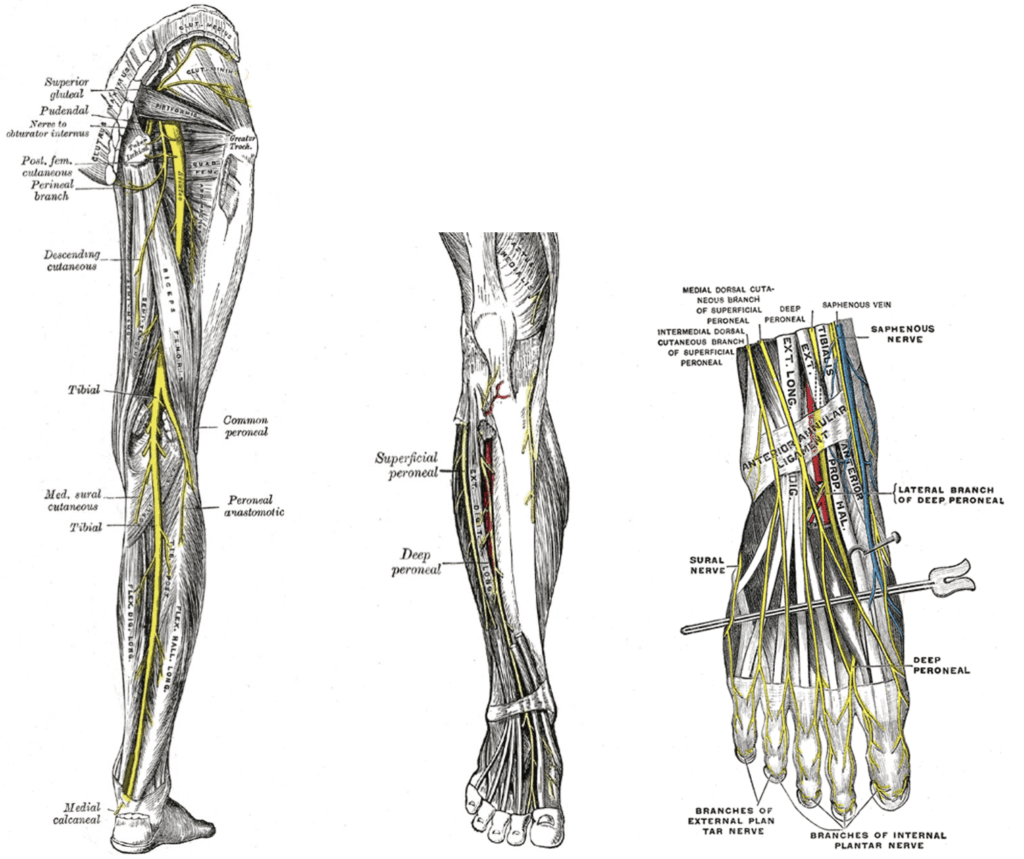
Structures passing superficial to the extensor retinaculum of the ankle:
- Medially: Saphenous Nerve, Great Saphenous Vein.
- Laterally: Branches of the Superficial Peroneal Nerve.
Structures passing deep or through the extensor retinaculum of the ankle, (medial → lateral):
- Tibialis anterior.
- Extensor hallucis longus
- Anterior tibial artery (and its venae commitantes).
- Deep peroneal nerve
- Extensor digitorum longus (four tendons)
- Peroneus tertius.
Appendix 2
References
Publications
- Brazis PW, Masdeu JC, Biller J. Localization in Clinical Neurology. 8e 2021
- Fuller G. Neurological Examination Made Easy. 6e 2019
- O’Brien M. Aids to the Examination of the Peripheral Nervous System. 6e 2023
FOAMed
- Coni R. Neuro 101: Peripheral Nervous System. LITFL
- Nickson C. Myotomes and Differentiating Nerve Lesions. LITFL
Fellowship Notes
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner
Educator, magister, munus exemplar, dicata in agro subitis medicina et discrimine cura | FFS |


