Crohn’s disease
Crohn’s disease is a chronic, immune-mediated inflammatory bowel disease (IBD) characterised by transmural inflammation that can affect any part of the gastrointestinal tract, from the mouth to the anus.
The terminal ileum and colon are most commonly involved, with a predilection for segmental (“skip”) lesions and a tendency toward complications such as strictures, fistulae, and abscess formation. Extraintestinal manifestations such as arthritis, uveitis, and erythema nodosum are frequently observed.
The disease typically presents in adolescence or early adulthood, with a second incidence peak in later life. Global prevalence is rising, particularly in industrialised nations, with estimates around 3.2 per 1,000 in Europe and North America . Risk factors include a family history of IBD, smoking, and certain genetic mutations, notably in the NOD2/CARD15 gene, which are associated with ileal involvement and a stricturing phenotype
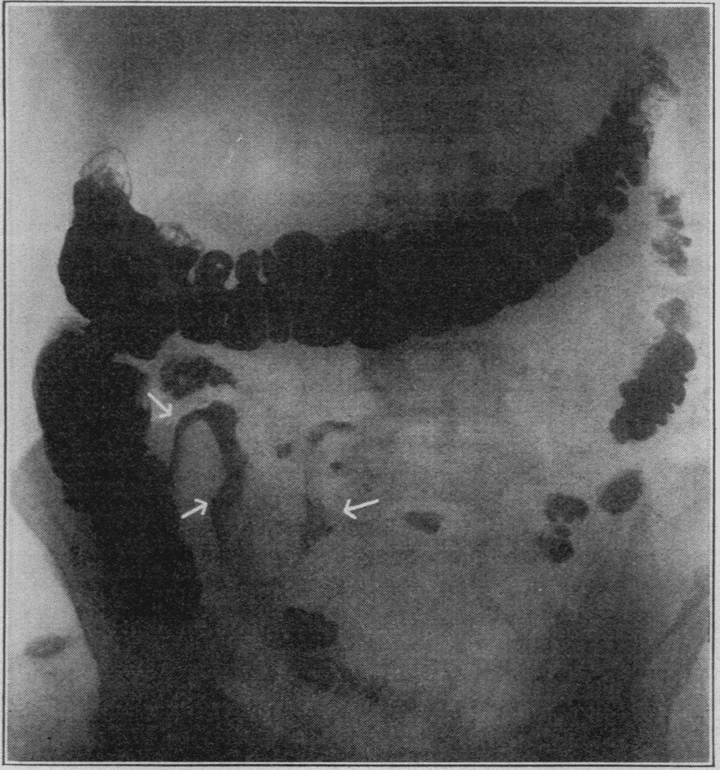
Diagnosis is established through a combination of clinical evaluation, endoscopic examination with biopsy, imaging studies, and laboratory tests. Endoscopic findings often reveal aphthous ulcers, cobblestoning, and skip lesions, while histology may show transmural inflammation and non-caseating granulomas. Imaging modalities such as MRI enterography and capsule endoscopy are valuable for assessing small bowel involvement.
Management aims to induce and maintain remission, prevent complications, and improve quality of life. Treatment strategies are tailored to disease severity and location and may include corticosteroids for acute flares, immunomodulators like azathioprine for maintenance, and biologic therapies targeting TNF-α or integrins for moderate to severe disease. Surgical intervention is reserved for refractory cases or complications such as obstruction or fistulae
History of Crohn’s disease
1769 – Giovanni Battista Morgagni (1682-1771) provided an early description of Ulceration of the intestines in De Sedibus et Causis Morborum (The Seats and Causes of Diseases). He describes the death and autopsy of a 20-year-old male patient who succumbed to a longstanding illness of fever, abdominal pain, and bloody diarrhoea. The autopsy revealed perforations and transmural inflammation with ulceration stretching from the terminal ileum to “two hands breadth” along the colon.
Ileum vero, atque intestinum caecum, atque colon, mirum in modum affecta erant. Nam haec intestina non modo inusitata crassitie conspicua, sed & ulceribus scatentia, & in multis locis cohaerentia, atque stricta visa sunt; ita ut materiae faecales difficulter transirent. Quaedam ulcera in intimo tunicae situ ita profunda, ut pene ad peritonæum usque penetrarent. Praeterea abscessus in pariete intestini repertus est, ad quem fistula perduxit, quae in cavitatem abdominis aperta erat – Morgagni, De Sedibus, 1761, Epist. XXXIV, Art. IX (Vol. II)
The ileum, cecum, and colon were found to be extraordinarily diseased. For these intestines were not only remarkable for unusual thickening, but also were full of ulcers, and in many places were adherent and constricted, so that the faecal material passed with great difficulty. Certain ulcers extended so deep within the tunic that they nearly reached the peritoneum. Furthermore, an abscess was discovered in the intestinal wall, into which a fistula opened, which in turn communicated with the abdominal cavity – Morgagni, De Sedibus, 1761, Epist. XXXIV, Art. IX (Vol. II)
1806 – Dr. William Saunders (1743-1817) communicated, to the Royal College of Physicians in London, ‘A singular case of stricture and thickening of the ileum‘, by Charles Coombe (1743–1817). The presentation included clinical history and autopsy findings…
[the patient] had been for many years troubled with flatulency and complaints in the bowels, attended with costiveness, a quick pulse and an irregular intermittent fever…He especially complained of wind and great costiveness, and about two to three hours after eating, of excessive pain in the bowels.
[at autopsy]…the lower part of the ileum as far as the colon, was contracted, for the space of three feet, to the size of a turkey’s quill.
Coombe, Saunders 1806 [published 1813]
1828 – John Abercrombie (1780-1844) in his Diseases of the Stomach and Intestinal Canal (1828), Abercrombie describes cases which demonstrate inflammatory lesions of the small intestine, including stricture formation, ulceration, and chronic obstruction, with clinical-pathological correlation. One example is the autopsy of a 63 year old lady with chronic diarrhoea, and abdominal pain:
There was great thickening and induration of the coats of the ileum at its termination in the colon and the opening was so narrowed that it only admitted the point of the little finger
1859 – Sir Samuel Wilks (1824–1911) advocates idiopathic colitis as distinct from epidemic dysentery; Dr Smethurst’s trial raises medico-legal interest in chronic intestinal inflammation.
…we have seen a case attended by discharge of mucus and blood where, after death, the whole internal surface of colon presented a highly vascular, soft, red surface, covered with tenacious mucus or adherent lymph, and here and there a few minute points of ulceration ; and the coats, also, much swollen by exudation into the mucous and submucous tissues.
In the small intestine nothing remarkable was observed until the lower end of the ileum was reached, when at about three feet from its termination in the caecum, the mucous membrane commenced to exhibit an inflammatory response. In the caecum, inflammation of the most acute and violent character was observed…
1904 – Antoni Leśniowski publishes case reports of nonspecific ileitis in Polish literature — frequently cited in European scholarship.
1913 – Thomas Kennedy Dalziel (1861–1924) read a paper on ‘Chronic Interstitial Enteritis‘ at the Annual B.M.A. Conference at Brighton. He presented nine cases of chronic interstitial enteritis with granulomas, distinguishing the condition from tuberculosis and concluded:
As far as I am aware the disease has not been previously described, but it seems probable that many cases must have been seen and have been diagnosed as tuberculous.
1923 – Eli Moschcowitz (1879-1964) and Abraham O. Wilensky (1885-1949) detail cases of nonspecific granulomatous inflammation of the intestine, highlighting features such as transmural inflammation, fistula formation, and the absence of caseating necrosis, distinguishing them from tuberculosis.
The lesions were characterized by a chronic inflammatory process involving the entire thickness of the intestinal wall, leading to the formation of strictures and fistulous tracts…In none of our cases was there any evidence of tuberculosis, either clinically or histologically
1927 – Follow-up article on Non-specific granulomata of the intestine by Moschcowitz and Wilensky presents additional cases and reinforces their earlier observations, further solidifying the concept of a distinct pathological entity. These early descriptions were pivotal in the recognition of a unique form of chronic intestinal inflammation, laying the groundwork for the later characterization of Crohn’s disease.
May 1932 – Burrill Crohn, along with Leon Ginzburg and Gordon Oppenheimer present “Terminal Ileitis: A New Clinical Entity” at the AMA in New Orleans. Initially listed as Crohn’s sole paper, co-authors were added after intervention by surgeon Dr A.A. Berg
October 1932 – Their article is published in JAMA as “Regional Ileitis: A Pathologic and Clinical Entity” — a concise clinicopathologic description of transmural necrotising inflammation in the terminal ileum. A case series of 14 patients aged between 17-years to 52-years:
We propose to describe, in its pathologic and clinical details, a disease of the terminal ileum, affecting mainly young adults, characterized by a subacute or chronic necrotizing and cicatrizing inflammation. The ulceration of the mucosa is accompanied by a disproportionate connective tissue reaction …associated with the formation of multiple fistulas.
The disease is clinically featured by symptoms resembling those of ulcerative colitis, ie, fever, diarrhea, emaciation, and a mass in the right iliac fossa usually requiring surgical resection. The etiology is unknown.
Crohn, Ginzburg, Oppenheimer 1932
1933 – Franklin Harris et al published an article titled ”Chronic cicatrizing enteritis: Regional enteritis (Crohn). A new surgicxal entity” as the first published reference to Crohn, recognising the term ‘regional ileitis’ but proposing ‘cicatrizing enteritis’ as an alternative.
1934 – John L. Kantor presented series of 6 cases (four operated on by AA Berg with pathology reviewed by Dr. Paul Klemperer at the Mount Sinai Hospital) all cases diagnosed nonspecific ulcerative granulomatous inflammation of the terminal ileum according to the criteria presented by Crohn and his collaborators in 1932.
1939 – Geoffrey Hadfield (1899–1981), professor of pathology at the University of London, evaluated the histological changes found in the terminal ileum and its related lymph nodes in 20 cases of regional ileitis:
The earliest and possibly the specific histological lesion of regional ileitis is lymphadenoid hyperplasia with the formation of non-caseating giant-cell systems in the submucosa. Acid-fast bacilli cannot be demonstrated histologically in these lesions. This lesion is also present in the regional lymph-nodes. Ulceration and fistulae are secondary to this lesion in the submucosa and the obstructive lymphoedema which it produces.
Hadfield 1939
1956 – President Dwight D. Eisenhower undergoes bowel resection for presumed Crohn disease. Crohn becomes public spokesperson, further cementing the eponym.
1988 – Michael Harmer argues in Bristol Medico-Chirurgical Journal that the condition should be renamed “Crohn–Dalziel disease,” citing Ginzburg’s personal letters refuting Crohn’s sole authorship.
2001 – Genetic studies identify NOD2/CARD15 mutations as susceptibility markers for Crohn disease — the first major molecular insight into its pathogenesis.
2000s–present – Advances in animal models and immunogenetics reveal Crohn disease as a dysregulated immune response to commensal microbiota, with clinical subtypes (inflammatory, stenotic, fistulizing) echoing those described in 1932.
The controversy
In 1932, Burrill Bernard Crohn, Leon Ginzburg, and Gordon David Oppenheimer co-authored the landmark JAMA article describing “regional ileitis,” as a new clinical and pathological entity affecting the terminal ileum. The trio were all based at Mount Sinai Hospital in New York, with Ginzburg and Oppenheimer having already prepared much of the pathological groundwork.
Crohn was initially slated to present a solo paper at the AMA meeting in New Orleans, but Mount Sinai’s chief surgeon, Dr A.A. Berg, insisted the work be credited to all three. The paper was eventually published alphabetically, but public and professional discourse quickly associated the disease primarily with Crohn.
Over time, Ginzburg and others expressed discomfort with Crohn receiving sole recognition. Ginzburg later wrote that Crohn had “taken credit” for pre-existing work. Historians and clinicians have since argued that earlier contributions — notably by Dalziel, Moschowitz, and Leśniowski — deserved equal or greater attribution. Nonetheless, the term “Crohn’s disease” gained traction globally, especially after President Eisenhower’s high-profile diagnosis in 1956.
Associated Persons
- Giovanni Battista Morgagni (1682-1771)
- Charles Coombe (1743-1817)
- John Abercrombie (1780-1844)
- Thomas Kennedy Dalziel (1861-1924)
- Eli Moschcowitz (1879-1964)
- Burrill Bernard Crohn (1884-1983)
- Leon Ginzburg (1898-1988)
- Gordon David Oppenheimer (1900-1974)
Alternative names
- Chronic interstitial enteritis (Dalziel, 1913)
- Non-specific granuloma (Moschowitz, 1927)
- Regional ileitis (Crohn, 1932)
- Leśniowski-Crohn’s disease (choroba Leśniowskiego-Crohna)
- Regional enteritis, Regional enterocolitis, Cicatrizing enteritis
- Crohn–Dalziel disease (Harmer 1988)
References
Historical references
- Morgagni GB. Ulceration of the intestines with flaccidity of the heart. In: The seats and causes of diseases, investigated by anatomy 1761 [Book III; Letter XXXI; Article 2] 1822 translation Vol II: 83-90
- Coombe C, Saunders W. A singular case of stricture and thickening of the ileum. Medical transactions 1813; 4: 16-21.
- Leśniowski A. Przyczynek do chirurgii kiszek. Medycyna (Warsaw). 1903;31:460–464, 483–489, 514–518.
- Dalziel TK. Chronic Interstitial Enteritis. Br Med J 1913; 2: 1068-1070.
- Moschowitz E, Wilensky AO. Non-specific granulomata of the intestine. The American Journal of the Medical Sciences 1923; 166: 48-66
- Wilensky AO, Moschowitz E. Non-specific granulomata of the intestine. The American Journal of the Medical Sciences 1927; 173: 374-380
- Crohn BB, Ginzburg L, Oppenheimer GD. Regional ileitis; a pathologic and clinical entity. JAMA, 1932; 99: 1323-1329.
- Harris F, Bell G, Brunn H. Chronic cicatrizing enteritis: Regional enteritis (Crohn). Surgery, Gynecology & Obstetrics 1933; 57: 637-645.
- Kantor JL. Regional (terminal) ileitis: its roentgen diagnosis. JAMA 1934; 103: 2016-21
- Hadfield G. The Primary Histological Lesion of Regional Ileitis, Lancet, 1939; 234(6058): 773-776
Review articles
- Armitage G, Wilson M. Crohn’s disease; a survey of the literature and a report on 34 cases. Br J Surg. 1950; 38(150): 182‐193.
- Heaton LD, Ravidin IS, Blades B, Whealan TJ. President Eisenhower’s Operation for Regional Enteritis: A Footnote to History. Ann. Surg., May 1964, 159: 661-666.
- Fein HD. The History of Crohn’s Disease. In: Korelitz B.I. (eds) Inflammatory Bowel Disease. 1982: 1-3
- Kirsner JB. Landmark perspective. Crohn’s disease. JAMA. 1984;251(1):80‐81.
- Ginzburg L. Regional enteritis: historical perspective (B. Crohn and L. Ginzburg) Gastroenterology. 1986; 90(5 Pt 1): 1310-1.
- Fielding JF. Crohn’s disease and Dalziel’s syndrome. A history. J Clin Gastroenterol. 1988; 10(3): 279‐285.
- Harmer M. Crohn’s disease–a misnomer? Bristol Med Chir J. 1988;103(1):9‐10.
- Ginzburg L. Leon Ginzburg 1899-1988. The road to regional enteritis. 1974. Dis Colon Rectum. 1992 Mar;35(3):273-6.
- Fazio VW, Aufses AH Jr. Evolution of surgery for Crohn’s disease: a century of progress. Dis Colon Rectum. 1999; 42(8): 979‐988.
- Baron JH. Inflammatory bowel disease up to 1932. Mt Sinai J Med. 2000; 67(3): 174‐189.
- Janowitz HD. Inflammatory bowel disease after 1932. Mt Sinai J Med. 2000; 67(3): 190‐197.
- Kirsner JB. Historical origins of current IBD concepts. World J Gastroenterol. 2001;7(2):175‐184.
- Aufses AH Jr. The history of Crohn’s disease. Surg Clin North Am. 2001; 81(1): 1‐vii.
- Franklin JL. Eisenhower and Crohn’s Disease. Hektoen International 2009; 1(2)
eponymictionary
the names behind the name
Bret P. Nelson, MD, AEMUS-FPD, FACEP. Professor of Emergency Medicine, System Vice Chair for Education in the Department of Emergency Medicine, System Chief of the EM Ultrasound Division Mount Sinai Hospital | Sinai EM |
BA MA (Oxon) MBChB (Edin) FACEM FFSEM. Emergency physician, Sir Charles Gairdner Hospital. Passion for rugby; medical history; medical education; and asynchronous learning #FOAMed evangelist. Co-founder and CTO of Life in the Fast lane | On Call: Principles and Protocol 4e| Eponyms | Books |

