CT Case 011
A 50yo male is brought to the ED after an OOHCA (out of hospital cardiac arrest) due to a large dose recreational fentanyl overdose.
He had prolonged CPR (>1hr) prior to return of spontaneous circulation (ROSC). Following ROSC, despite double strength vasopressors he remained hypotensive with a systolic blood pressure SBP ~60mmHg.
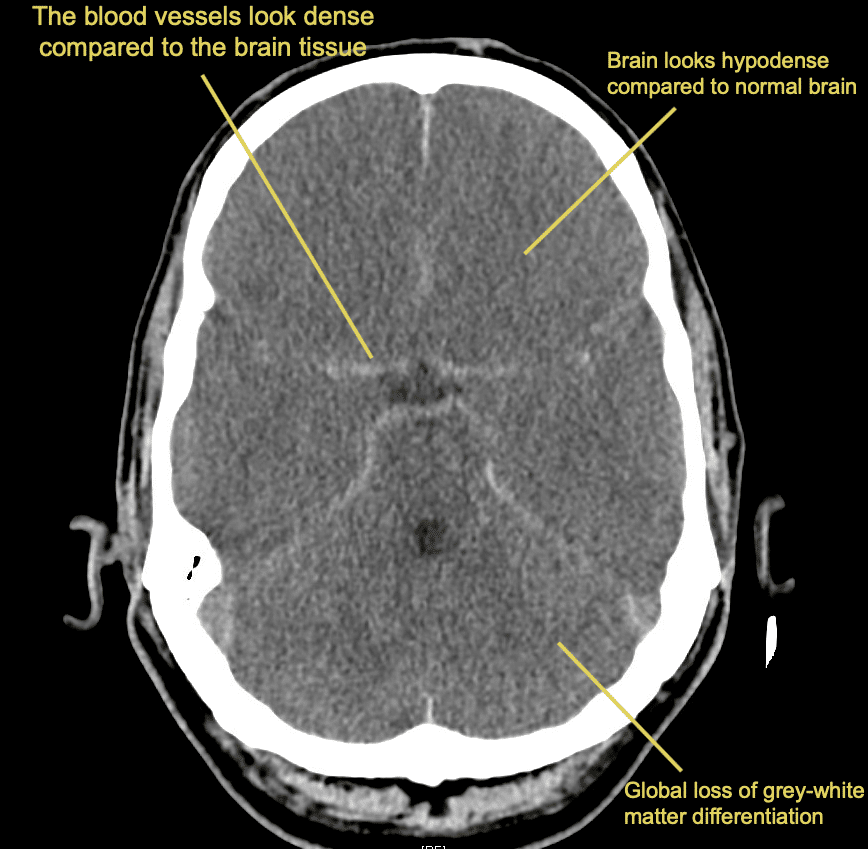
Describe and interpret the CT scan
CT INTERPRETATION
There is (relative) increased density of the circle of Willis compared to the brain parenchyma.
The brain parenchyma has reduced density (looks darker compared to normal appearance) and there is loss of grey-white matter differentiation.
The ventricles are small (slit like) and there is sulcal effacement.

CLINICAL CORRELATION
Pseudo-subarachnoid haemorrhage
A quick glance at this CT and you might be fooled into thinking this patient has had a massive SAH, but this is actually a case of ‘Pseudo-subarachnoid haemorrhage’.
Pseudo-subarachnoid haemorrhage is an artifact of CT imaging seen when the intracranial vessels appear more-dense compared to the brain parenchyma.
This is caused by diffuse cerebral oedema which lowers the density of the brain tissue on CT, making the vessels appear more prominent by comparison.
The cause of cerebral oedema in this case was cardiac arrest with prolonged downtime causing global ischaemia of brain tissue.
We look for the same CT changes in global ischaemia as we would in focal ischaemia (ie a CVA), that is;
- Cerebral oedema (decreased denisty of the brain parenchyma, loss of grey-white matter differentiation)
- Effacement of the cerebral sulci and slit-like appearance of ventricles. This is the result of mass effect caused by the oedema
There are a few other pathologies that can mimic the appearance of SAH, also causing ‘PseudoSAH’, these are;
- Severe polycythaemia (higher concentration of haemoglobin in the vessels makes the vessels appear more prominent)
- Purulent meningitis (the blood-brain barrier is disrupted and protein can enter the subarachnoid space)
- Meningeal leukaemia (increased cell mass in the subarachnoid space)
Cerebral oedema, as seen in this case, is by far the most common cause of PseudoSAH
REFERENCES
- O’Hare M, Berkowitz AL. Pseudo-Subarachnoid Hemorrhage. Neurohospitalist. 2021 Jan;11(1):93-94.
- Zubair AS, Johnson M, Gilmore EJ. Pseudosubarachnoid hemorrhage. Surg Neurol Int. 2022 Jan 29;13:32
[cite]
TOP 100 CT SERIES
Dr Leon Lam FRANZCR MBBS BSci(Med). Clinical Radiologist and Senior Staff Specialist at Liverpool Hospital, Sydney
Emergency Medicine Education Fellow at Liverpool Hospital NSW. MBBS (Hons) Monash University. Interests in indigenous health and medical education. When not in the emergency department, can most likely be found running up some mountain training for the next ultramarathon.
Sydney-based Emergency Physician (MBBS, FACEM) working at Liverpool Hospital. Passionate about education, trainees and travel. Special interests include radiology, orthopaedics and trauma. Creator of the Sydney Emergency XRay interpretation day (SEXI).





