CT Case 034
A 70-year-old man presents with sudden onset of severe epigastric pain, radiating to his back.
His vitals are HR 85, BP 175/90, Sats 99% RA, RR 22, and he is afebrile
As part of his work-up he has a CT aortogram to exclude an aortic dissection.


Describe and interpret the CT images
CT INTERPRETATION
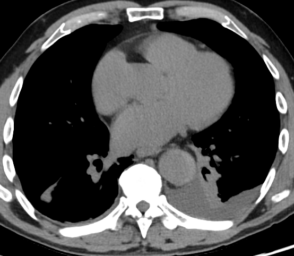
There is an acute aortic intramural haematoma (IMH) involving the descending aorta. It is seen as hyperdense crescentic eccentric thickening of the aortic wall which does not enhance on aortogram.
The haematoma starts from the level of the aortic isthmus (anatomically located between the origin of the subclavian artery and the ligamentum arteriosum) and continues until just above the coeliac trunk.

There is a small left pleural effusion.
There is no dissection flap or intimal tear seen.
On additional views the was no sign of involvement of the ascending aorta, aortic root or coronary arteries.



CLINICAL CORRELATION
An aortic intramural haematoma is part of the spectrum of acute aortic syndrome
The Acute aortic syndromes comprise;
- Aortic dissection
- Intramural haematoma (IMH)
- Penetrating atherosclerotic ulcer
Pathogenesis of IMH
An intramural haematoma is confined within the medial layer of the aorta (the tunica media) in the absence of a detectable intimal tear, which is the key difference between IMH and aortic dissection.
The definite mechanism of intramural haematoma formation is unclear. Two mechanisms have been described; rupture caused by penetrating atherosclerotic ulcer and spontaneous rupture of the vasa vasorum vessels within the tunica media.
An intramural haematoma can be a precursor to aortic dissection or rupture.

Classification
As with aortic dissections, intramural haematomas are categorised according to the Stanford classification.
- Type A; pathology involves the ascending aorta (with or without descending aorta involvement)
- Type B; limited to the descending aorta

Radiographic features of intramural haematoma
There are certain radiographic features that tell us this is an intramural haematoma rather than an aortic dissection
- The absence of an intimal flap (see case 006 for example of dissection flap seen)
- There is a crescent shape (representing the haematoma) along the aortic wall. On non-contrast scan this is hyperdense relative to the aortic lumen
- On the post-contrast scan the intramural haematoma is hypodense compared to the aortic lumen as it does not enhance with contrast
- There is absence of compression of the aortic lumen
Note, this patient had both non-contrast and arterial phase CT scans, the non-contrast scan helps quickly identify the intramural haematoma.
Management decisions
The management principles of intramural haematoma are the same as for aortic dissection.
As a general rule the treatment of Type A syndromes is surgical and Type B syndromes are usually managed medically (that is analgesia and aggressive BP and HR control).
References
- Chao CP, Walker TG, Kalva SP. Natural history and CT appearances of aortic intramural hematoma. Radiographics. 2009 May-Jun;29(3):791-804.
- Braverman AC. Acute aortic dissection: clinician update. Circulation. 2010 Jul 13;122(2):184-8.
- Alomari IB, Hamirani YS, Madera G, Tabe C, Akhtar N, Raizada V. Aortic intramural hematoma and its complications. Circulation. 2014 Feb 11;129(6):711-6.
- Lopez KN, Tume SC, Hall SR, Liou A, Kristen S, Tejtel S, Mery CM. Aortic Coarctation and Interrupted Aortic Arch. Texas Children’s hospital
[cite]
TOP 100 CT SERIES
Dr Leon Lam FRANZCR MBBS BSci(Med). Clinical Radiologist and Senior Staff Specialist at Liverpool Hospital, Sydney
Sydney-based Emergency Physician (MBBS, FACEM) working at Liverpool Hospital. Passionate about education, trainees and travel. Special interests include radiology, orthopaedics and trauma. Creator of the Sydney Emergency XRay interpretation day (SEXI).
Provisional fellow in emergency radiology, Liverpool hospital, Sydney. Other areas of interest include paediatric and cardiac imaging.
Emergency Medicine Education Fellow at Liverpool Hospital NSW. MBBS (Hons) Monash University. Interests in indigenous health and medical education. When not in the emergency department, can most likely be found running up some mountain training for the next ultramarathon.




