Dealing with D-dimer debacles
aka Hematology Hoodwinker 001
An intern in the emergency department has been nervously standing behind you for the past ten minutes while you’ve dealt with a barrage of phone calls. He wants to discuss the positive D-dimer result of the patient he is working up.
You look to the patient’s cubicle and see a 30 year-old man looking around nervously between taking bites out of a sandwich and texting on his iphone. You take a deep breath, crack your knuckles, and prepare yourself for the ‘d-dimer’ talk….
Questions
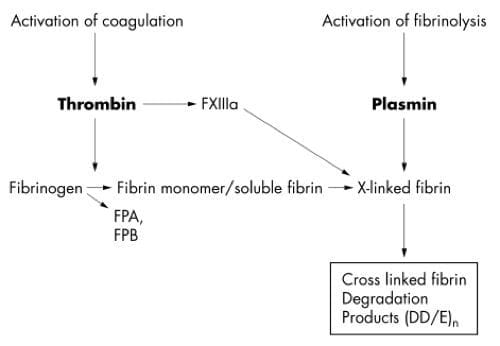
Q1. What are D-dimers?
Q2. When is the D-dimer test indicated?
Answer and interpretation
The D-dimer assay can be used as a “rule out” test in the emergency department when the pre-test probability of venous thromboembolism (VTE) is low.
The pre-test probability is best assessed using a clinical prediction guide (CPG), such as the Wells criteria or the revised Geneva score for pulmonary embolism (PE) and the Wells criteria for deep vein thrombosis (DVT). For instance, a ‘negative’ D-dimer test result when using a highly sensitive assay can ‘rule out’ VTE using the Wells’ clinical prediction guides if:
- Low/intermediate probability of PE (score 0 to 6) — Wells criteria for PE
- DVT unlikely (score 0 or 1) — Wells criteria for DVT
The D-dimer assay can also be used to help diagnose fibrinolytic disorders such as venom-induced consumptive coagulopathy (VICC) and disseminated intravascular coagulation (DIC).
This is my approach to the use of the d-dimer assay in the emergency department:

How to use the D-dimer assay in the Emergency Department. Note that highly sensitive D-dimer assays can be used to rule out PE in patients with low or intermediate Wells scores (0 to 6), less sensitive assays should only be used for low Wells scores (0 to 2).
[see Pulmonary Puzzle 010 for a discussion of the PERC rule]
Q3. Can the D-dimer test be used to rule out thoracic aortic dissection?
Answer and interpretation
No
The systematic review of 10 studies by Sutherland et al (2008) showed that D-dimer cannot be used as a sole screening tool for acute aortic dissection. Problems with the studies include:
- 4 of the 10 studies had sensitivities <95%, and 3 of the 5 studies with sensitivities of 100% had the lower limit of the 9% confidence interval <85%. Thus the sensitivty of the D-dimer is insufficient for ruling out a ‘must not miss’ diagnosis like acute aortic dissection
- inclusion bias and poorly defined inclusion criteria
- poorly defined duration of symptoms prior to performing the D-dimer test (up to 120 hours)
- the studies do not assess how clinical suspicion or other investigations affected the use of the D-dimer test
- heterogeneity of D-dimer assays used and the cut-off values used
- the non-specificity of the D-dimer test might lead to excessive imaging
- use of the D-dimer in high risk cases may delay definitive imaging and treatment
Q4. Can the D-dimer test be used to rule atrial thrombus in a patient with atrial fibrillation, thus allowing safe cardioversion?
Answer and interpretation
No — early studies are promising but the test is not yet ready for ‘prime-time’ for this use.
A Best Bets review (updated in 2007) suggests that a negative D-dimer test may be able to rival echocardiography in ruling out an atrial thrombus in atrial fibrilation (negative predictive value ~98%), thus allowing cardioversion to be safely performed in the emergency department without the need for further investigation. However many of the studies included were in Japanese and only the English language abstracts were appraised. A large well-designed study is needed to confirm these promising findings.
Q5. What situations may result in a ‘false negative’ D-dimer assay when investigating for possible venous thromboembolic disease?
Answer and interpretation
VTE can occur in the presence of a negative D-dimer test
D-dimer assays can only be used to rule out VTE if the pre-test probability is sufficiently low. Negative results in the presence of VTE can occur if:
- there is a small clot load (eg. small calf only DVTs)
- the thrombus has matured over time
- the patient has defective fibrinolysis (which can contribute to thrombus formation in the first place)
Q6. What ‘non-pathological’ conditions are associated with elevated D-dimer titres?
Answer and interpretation
Non-pathological conditions associated with elevated D-dimer titres include:
- Age (healthy elderly people)
- Cigarette smoking
- Functional impairment
- Post-operatively
- Pregnancy
- Race (e.g. African Americans)
Q7. What pathological conditions are associated with elevated D-dimer titres?
Answer and interpretation
Pathological conditions associated with elevated D-dimer titres include
- Acute coronary syndromes
- Acute upper gastrointestinal haemorrhage
- Aortic dissection
- Arterial or venous thromboembolism
- Atrial fibrillation
- Consumptive coagulopathy – DIC, VICC
- Infection
- Malignancy
- Pre-eclampsia
- Sickle cell disease
- Stroke
- Superficial thrombophlebitis
- Trauma
Q8. Can the D-dimer assay be used to rule out VTE in an elderly patient?
Answer and interpretation
Yes, with caveats.
The D-dimer assay is more likely to give a positive result in the elderly, limiting the usefulness of the test. However, if the D-dimer is negative it can still be used to rule out VTE in elderly patients with low pre-test probabilities. A recent retrospective study by Douma et al (2010) suggests that higher cut-offs might be safely used in patients over 55 years of age.
Q9. Can the D-dimer assay be used to rule out VTE in a pregnant patient?
Answer and interpretation
Yes, with caveats.
As in the elderly, the D-dimer test result is more likely to be positive. The D-dimer result is nearly always positive in the third trimester, and less so the earlier the pregnancy. A negative D-dimer test in a patient with a low pre-test probability still ‘rules out’ VTE.
Q10. Are there different types of d-dimer assays? Does it matter?
Answer and interpretation
There are many different D-dimer assays (qualitative and quantitative) available.
Different types of assay are not standardized and have varying sensitivities and specificities, but they generally have high sensitivity and negative predictive value for the presence of thrombus in patients with low pre-test probabilities. Furthermore, different laboratories may use different ‘cut-offs’ for what constitutes a positive or negative result.
The performance characteristics of the available D-dimer assay can affect its use in clinical decision making.
I am most familiar with the HemosIL DD HS assay, which is a rapid highly sensitive ‘second-generation’ latex agglutination D-dimer assay. This has similar performance characteristic to the best performing ELISA assays, unlike ‘first-generation’ latex agglutination assays. The published data for the HemosIL DD HS assay’s performance characteristics (using a cut-off of 230 ng/mL) are:
- Sensitivity: 100% (95%CI 95.4-100%)
- Negative predictive value: 100% (95%CI 96.5-100%)
- Specificity: 46.8% (95%CI 40.1-53.6%)
It turns out that the patient is a lawyer. He has a sore right calf and additional symptoms consistent with a mild panic attack. He wants to know what the meaning and significance of a positive or negative D-dimer test.
Q11. What will you say?
Answer and interpretation
As you would say to any patient, something that encapsulates this information:
- The D-dimer test is a marker of blood clotting activity and is not diagnostic of VTE
- When used appropriately the D-dimer test helps “rule out” VTE if the test is negative and the chance of the patient having a VTE is relatively low
- If the D-dimer test is positive further investigation may or may not be necessary depending on the likely cause of the elevated D-dimer result, of which there are many
- Diagnosis of VTE is based on probabilities and balances the risks of further investigation against the risk of missing the diagnosis. No investigation can reduce the chance of having VTE to ‘absolute zero’.
- D-dimer negative patients can still develop VTE and should be advised to return if symptoms worsen or new symptoms develop (e.g. worsening of leg pain and swelling, shortness of breath, chest pain or collapse)
References
- Body R, Allie B. Towards evidence based emergency medicine: best BETs from the Manchester Royal Infirmary. Negative D-dimer may allow safe early cardioversion of atrial fibrillation. Emerg Med J. Jun 2007;24(6):432-435 PMID: 17513547 [D-dimer in AF]
- Chunilal SD, et al. (2003) Does this patient have pulmonary embolism?. JAMA, 290(21), 2849-58. PMID: 14657070
- De Moerloose P, et al. Performances of the HemosIL D-dimer HS assay for the exclusion of venous thromboembolism. J Thromb Haemost. 2005;3:2361-2363 PMID: 16194215
[The highly sensitive D-dimer assay mentioned in Q10] - Douma RA et al. Potential of an age adjusted D-dimer cut-off value to improve the exclusion of pulmonary embolism in older patients: a retrospective analysis of three large cohorts. BMJ May 2010;340:c1475 PMID: 20354012
- Fields JM, & Goyal M (2008). Venothromboembolism. Emerg Med Clin North Am, 26 (3) PMID: 18655939
[Highly recommended review article includes the VTE CPGs used in this Q&A] - Ho WK, et al. Venous thromboembolism: diagnosis and management of deep venous thrombosis. Med J Aust. May 2 2005;182(9):476-481 PMID: 15865594
[Australian DVT Guidelines] - Lee CH, et al. Venous thromboembolism: diagnosis and management of pulmonary embolus. Med J Aust. 2005; 182 (11): 569-574 PMID: 15938684
[Australian PE Guidelines] - Le Gal G, et al. Prediction of pulmonary embolism in the emergency department: the revised Geneva Score. Ann Intern Med 2006;144:168 PMID: 16461960
[Revised Geneva Score] - Sutherland A, et al. D-dimer as the sole screening test for acute aortic dissection: a review of the literature. Ann Emerg Med. Oct 2008;52(4):339-343 PMID: 18819176
[D-dimer in acute aortic dissection] - Wakai A, et al. Role of fibrin D-dimer testing in emergency medicine. Emerg Med J. 2003;20:319-325 PMID: 12835339
[Good review of the use of the D-dimer in the emergency department] - Wells PS, et al. Evaluation of D-dimer in the diagnosis of suspected deep-vein thrombosis. N Engl J Med. Sep 25 2003;349(13):1227-1235 PMID: 14507948
- Wells PS, et al. Derivation of a simple clinical model to categorize patient’s probability of pulmonary embolism: increasing the models utility with the SimpliRED D-dimer. Thromb Haemost 2000;83:416–20
- Wells PS, et al. Does this patient have deep vein thrombosis? JAMA. Jan 11 2006;295(2):199-207 PMID: 10744147
CLINICAL CASES
Hematology Hoodwinker
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC

What are the DOAC effects (or not) on d-dimer? e.g. a patient with AF on DOAC presents with a suspicious calf swelling
Dabigatran, Rivaroxaban, and apixaban do not affect D-dimer results according to this review:
https://onlinelibrary.wiley.com/doi/full/10.1111/ijlh.12235
Cheers
Chris