Death Adder
The Death Adder are found throughout most of Australia and Papua New Guinea but bites and envenoming are rare. They are largely nocturnal at is unheard of for them to bite above knee height because they lie in wait for prey twitching its grub-like tail close to its head as a lure. When an animal approaches to investigate the movement, the death adder quickly strikes. The classic presentation of an envenomed patient includes a painful bite site with a symmetrical descending flaccid paralysis and normal blood tests.
The Death Adder has a number flavours including: Common Death Adder, Barkly Tableland death adder, smooth-scaled death adder (PNG), northern death adder, desert death adder, rough-scaled death adder (PNG) and Pilbara death adder.
Resus
- Potential to be immediately life threatening, the patient should initially be managed in an area capable of resuscitation.
- Early threats to life include hypotension and descending flaccid paralysis.
- If respiratory failure occurs regardless of whether antivenom has been given, provisions should be made to secure the airway and to ventilate the patient.
Risk Assessment
Typical symptoms include:
- Pain at the bite site – puncture wounds may not be apparent
- Local swelling and bruising – sometimes the wounds can develop cellulitis
- Non-specific symptoms including nausea and vomiting
- Myotoxicity is uncommon and usually mild
- When envenomed the characteristic presentation is a progressive symmetrical descending flaccid paralysis (usually within 6 hours). Early signs include ptosis, blurred vision, diplopia and difficulty swallowing. With more advanced cases, respiratory failure maybe evident. The paralysis usually resolves after 1-2 days.
Supportive Care
- Symptomatic relief – IV fluids (if hypotensive / raised CK), antiemetics, analgesia
- Intubation and Ventilation if respiratory failure is present.
- Pressure bandage with Immobilisation (PBI) – Should have been applied pre-hospital, if not apply while awaiting initial investigations.
PBI Video
Investigations
1. Laboratory Tests (At presentation, 1 hour post PBI removal, 6 and 12 hours following the bite): FBC, EUC, CK, INR, APTT, Fibrinogen, D-dimer. Never use point of care testing for D-dimer or INR. If there is no evidence of envenoming at 12 hours after the bite (including 6 hours post PBI removal), the patient is fit for discharge (although not during the night as subtle neurotoxicity maybe missed).
2. Death Adder envenoming will have no clotting abnormalities and only clinical findings to confirm the diagnosis. Therefore spirometry can be a good measure of pending respiratory decline alerting you to the potential for intubation and ventilation. Clinical exam for descending paralysis should also be performed with the spirometry, check these every time you do bloods as a minimum.
3. The CK maybe mildly elevated
4. The Snake Venom Detection Kit (SVDK): This is not used to diagnose envenoming but can be used to determine which monovalent antivenom to use if more than one snake could be responsible for the observed clinical features. This kit does produce false positives and false negatives, caution needs to be used and contacting a clinical toxicologist is highly recommended if your patient is envenomed.
Differential Diagnosis:
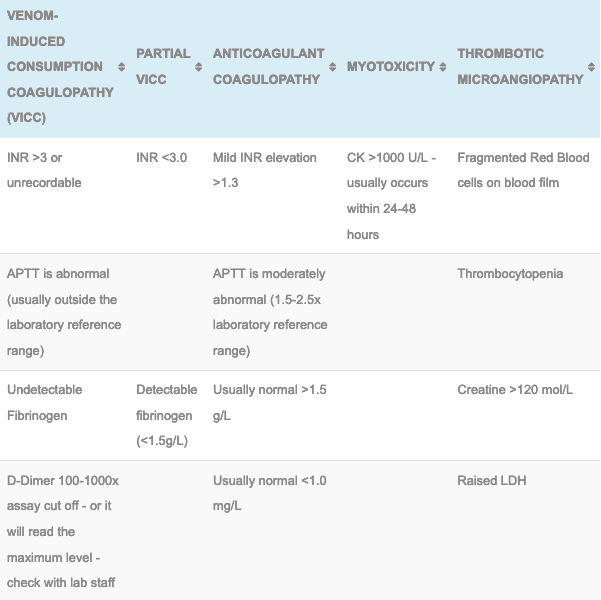
- Tiger, Taipan and Brown snakes (rarely) cause a neurotoxic paralysis but these are all associated with a venom-induced consumptive coagulopathy.
Antivenom
- 1 amp CSL monovalent Death Adder Antivenom: Used in the treatment of envenomation by the death adder, failing the availability of death adder antivenom, CSL Polyvalent Antivenom maybe used.
- See Death Adder antivenom for dosing, administration and complication details
Disposition
- All patients must be observed in a hospital capable of managing a potential snake bite envenomation, this involves adequate laboratory cover and the ability to administer antivenom and manage potential anaphylaxis.
- Patients with no clinical evidence of paralysis at 12 hours post bite are not envenomed and maybe discharged in daylight hours.
- Envenomed patients can be discharged following antivenom, complete reversal of their paralysis and have remained well for a subsequent 24 hours.
References and Additional Resources:
Additional Resources:
- Death Adder antivenom
- Polyvalent antivenom
- Approach to the Snakebite Patient
- Tox Conundrum 005 – Snakebite vs Stickbite
- Tox Conundrum 026 – Snakebite Envenoming Challenge
Zeff – James Hayes Fellowship teaching Snakebite
References:
- Currie BJ. Snakebite in tropical Australia: a prospective study in the “Top End” of the Northern Territory. Medical Journal of Australia 2004; 181: 693-697.
- Johnston CI, O’Leary MA, Brown SCA et al. Death adder envenoming causes neurotoxicity not reversed by antivenom – Australian Snakebite Project (ASP-16). PLoS Neglected Tropical Diseases 2012; 6(9):e1841
- Lalloo DG, Trevett AJ, Black J et al. Neurotoxicity, anticoagulant activity and evidence of rhabdomyolysis in patients bitten by death adders (Acanthophis sp) in southern Papua New Guinea. Quarterly Journal of Medicine 1996; 89:25-35
- Little M, Pereira P. Successful treatment of presumed death adder neurotoxicity using anticholinesterases. Emergency Medicine 1996; 89:25-35
- White J. A clinician’s guide to Australian venomous bites and stings: Incorporating the updated CSL antivenom handbook. Melbourne: CSL Ltd, 2012

Toxicology Library
TOXINS
Dr Neil Long BMBS FACEM FRCEM FRCPC. Emergency Physician at Kelowna hospital, British Columbia. Loves the misery of alpine climbing and working in austere environments (namely tertiary trauma centres). Supporter of FOAMed, lifelong education and trying to find that elusive peak performance.