ECG Case 080
This 53 year old male presented to ED following an episode of collapse.
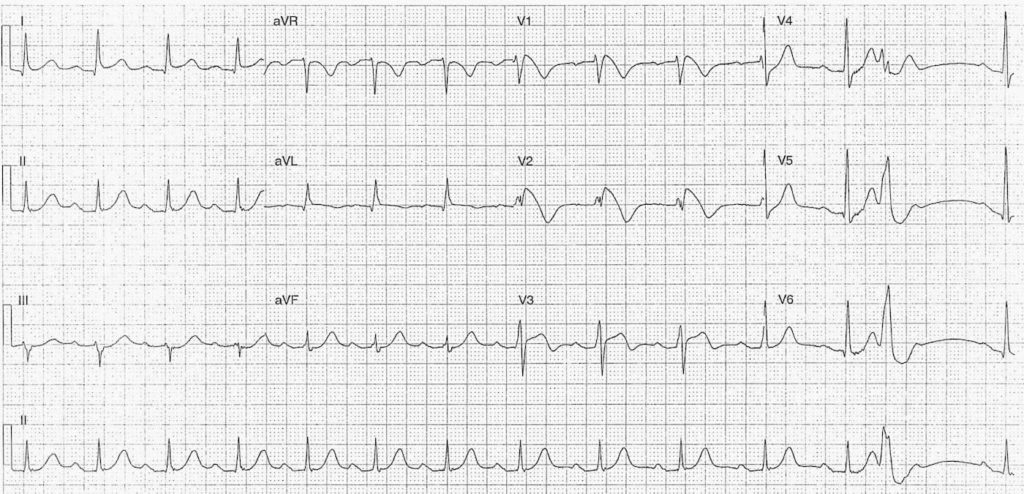
Describe and interpret this ECG
ECG ANSWER and INTERPRETATION
Rate:
- 88bpm
Rhythm:
- Regular sinus rhythm
- Single PVC
Axis:
- Normal (~20 deg)
Intervals:
- PR – Prolonged (~240ms)
- QRS – Normal (100ms)
- QT – 400ms (QTc Bazette ~ 480 ms)
Segments:
- ST elevation with coved morphology in leads V1 (2mm) and V2 (~4mm)
- ST elevation with concave morphology in leads I (<1mm) and V3 (~2mm)
- ST depression V4, V5
Additional:
- T wave inversion leads aVR, aVL, V1-3
- Compensatory pause post PVC of ~1.2s
- Partial RBBB
- rsR’ pattern V2
- Note PVC is closely coupled near preceding T wave peak
Interpretation:
- Brugada Syndrome
- History of syncope
- Type 1 Pattern
- 1st degree AV block
CASE FOLLOW UP
What happened next in this case really highlights why anyone looking at ECG’s needs to be able to recognise this particular ECG pattern.
Shortly after the patient arrived in the Emergency Department he had two episodes of VF arrest both reverted following asynchronous DC cardioversion. He was transferred to a tertiary centre for further investigation and management, including:
- Angiogram – multi-vessel irregularities
- ECHO – normal, ejection fraction of 65%
- Cardiac MRI – no RV or outflow tract dysplasia, no LV scarring or lesion.
He then underwent Automatic Implantable Cardioverter Defibrillator (AICD) insertion and was discharged from hospital within the week.
CLINICAL PEARLS
So what is Brugada Syndrome?
It’s an inherited sodium channelopathy, associated with sudden death and syncope due to polymorphic VT and, as in our case, VF.
Three types of ECG pattern are describe in Brugada, although only type 1 is considered diagnostic, as shown in our ECG.
Type 1 ECG pattern:
- Cove-shaped ST elevation of at least 2mm followed by a negative T wave in one or more of leads V1-3
In conjuction with these ECG features you need, at least, one of the following:
- Document VF / polymorphic VT
- Family history of sudden cardiac death at <45 years
- Type 1 pattern ECG i n family members
- Inducibility of VT with programmed stimulation
- Syncope
- Nocturnal agonal respiration
- Attributed to self-terminating VF/polymorphic VT
The above diagnostic criteria are taken from the CSANZ (Cardiac Society of Australia and New Zealand) Guidelines for the diagnosis and management of Brugada syndrome, this document is well worth a read as it covers pathophysiology, diagnostic criteria, management, and includes examples of the type 2 and type 3 ECG patterns.
Also check out the following great blog posts on Brugada:
- ECG Library – Brugada Syndrome
- ALiEM – An ECG Pattern You Need to Know
- ECG Interpretation Blog – ECG Case of pre-syncope
What can/should we do about it ?
As an emergency physician encountering a case of suspected / likely Brugada it’s easy, phone your cardiologist. For those patients with a Brugada pattern ECG with a history of syncope, arrest, or arrhythmias, definitive treatment is an AICD insertion. The incidental Brugada pattern in the otherwise well patient is a bit more controversial, again from an Emergency Medicine perspective phone your cardiology team. The CSANZ guidelinecontains a nice algorithm for the diagnostic approach to Brugada and also discusses management strategies in the incidental and asymptomatic Brugada.
We should also be aware that some drugs can cause Brugada-like ECG changes and should be avoided in patients with known or suspected Brugada. For more information on what not to give go to www.brugadadrugs.org which contains information for both clinicians and patients.
Check out these cases from Dr Smith’s blog (Case 1 and Case 2) which illustrate Brugada-like changes secondary to drug therapy.
Avoiding certain drugs raises the question what should we give ?
The simple answer is electricity in the setting of acute arrhythmia.
In those patients experiencing an arrythmic storm, or having repeated ICD shocks then iv isoprenaline has been proven to be useful and is recommended in the CSANZ guidelines.
For chronic prevention of arrhythmia the only oral agent shown to work is quinidine, but this is often very difficult to source.
Ii is also worth noting that fever can unmask Brugada, due to impaired sodium channel function and aggressive management of fever should be instigated. Other potential precipitants include alcohol, hypokalaemia, cocaine, large carb meals, and very hot baths.
But I’ll never see it ?
- The simple answer to this is that it’s entirely possible you will.
- The issue is will you recognise it?
I work in a district general Emergency Department seeing ~90,000 attendances a year across a mixed population. This year alone I’m aware of at least 3 cases of Brugada that have been diagnosed in our Emergency Department.
This is an ECG pattern we must be aware of and understand the implications it has for the patient and what needs to happen next.
This isn’t small print stuff, this isn’t once a career pick-up, this is a real condition that you can easily encounter in any ED, at any time.
Guest Editorial by Dr Ken Grauer
Excellent case by John Larkin – with a classic ECG pattern plus bonus of not only displaying Brugada Type 1 changes in leads V1,V2 – but also J-point subtle-but-real ST elevation in leads I,aVL – legitimate ST elevation in lead V3 (that does not look like the Brugada changes we see in V1,V2) – a “telltale” PVC (this patient had several VF episodes soon thereafter) – plus almost hyperacute (broad) T waves in several leads and a hint of lateral precordial ST depression. Certainly not normal accompaniments to the ominous pattern we see in leads V1,V2.
Words don’t do the “Brugada Type I ST Segment” justice. More than just “cove-shaped ST elevation ≥2mm with negative T in ≥1 leads V1-3” – You just have to see (and embed) the picture of the ST segments of Brugada Syndrome in your mind. It is not RBBB or incomplete RBBB. The ST segment elevation doesn’t last; instead there is a rapid downslope (steeply directed downward) that is not Wellens, and unique to Brugada syndrome. A picture is worth a thousand words. The image in V1,V2 of this case needs to be embedded in the mind.
As to “rarity” of the syndrome – there is to me a “disconnect”. How can what is now felt to be one of the most common causes of sudden death in younger adults be “rare”? It IS “out there”. It is not commonly out there in classic ECG form as in the classic tracing of this case obtained from a man with syncope and then VFib in the ED. But Brugada Syndrome seems to be far more prevalent than it ever was in years past – and the pattern WILL be seen by virtually all medical providers who obtain and interpret ECGs on their patients.
But the concern is not so much with classic cases as the one presented here – in which the need for immediate referral to Cardiology for AICD placement after resuscitation from VFib is obvious. Instead – the much more prevalent issue is what to do with all the not-quite-Brugada-pattern ECGs that show saddleback (rather than downsloping) ST segment elevation in anterior leads – or perhaps hint of more than a simple rSr’ in V1 with high J-point takeoff – and in addition present with a history of perhaps questionable presyncope – equivocal family history of sudden death – and/or perhaps manifest background “benign” early repolarization on 12-lead (that might not be so “benign” ). “Rarity” is a relative term. We are increasingly appreciating the legion of other conditions that may intermittently precipitate Brugada-like ECG manifestations – including fever, various drugs, stress, hot baths, hypokalemia, other severe medical illness. What clinical implications are for these intermittent Brugada-like patterns is far less certain. Almost wishing you didn’t see such patterns – the question then arises as to what truly merits not only referral, but consideration for prophylactic AICD placement? Not all answers are in – but we’ll all be watching as management of this entity refines over the near future. In the meantime – awareness of frank cases such as the illustrative one presented here need to be universally recognized on sight for the ominous threat they pose by all health care providers.
THANKS for presenting this great case John!
TOP 100 ECG Series
Emergency Medicine Specialist MBChB FRCEM FACEM. Medical Education, Cardiology and Web Based Resources | @jjlarkin78 | LinkedIn |