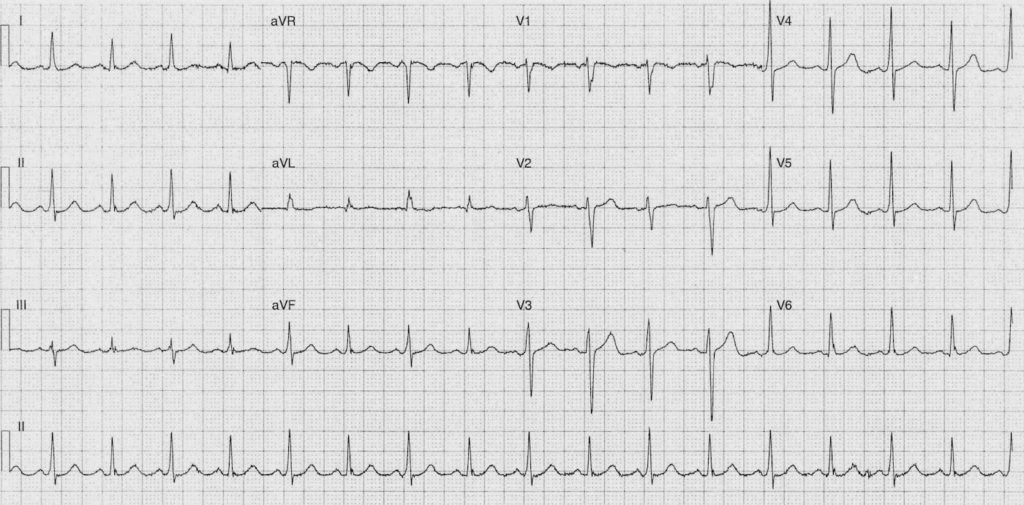
ECG Case 097
54 year old lady attends with 2 month history of ‘chest flutterings’
Describe and interpret this ECG
ECG ANSWER and INTERPRETATION
Rate:
- 102 bpm
Rhythm:
- Regular
- Sinus Rhythm
- Alternating QRS Morphologies
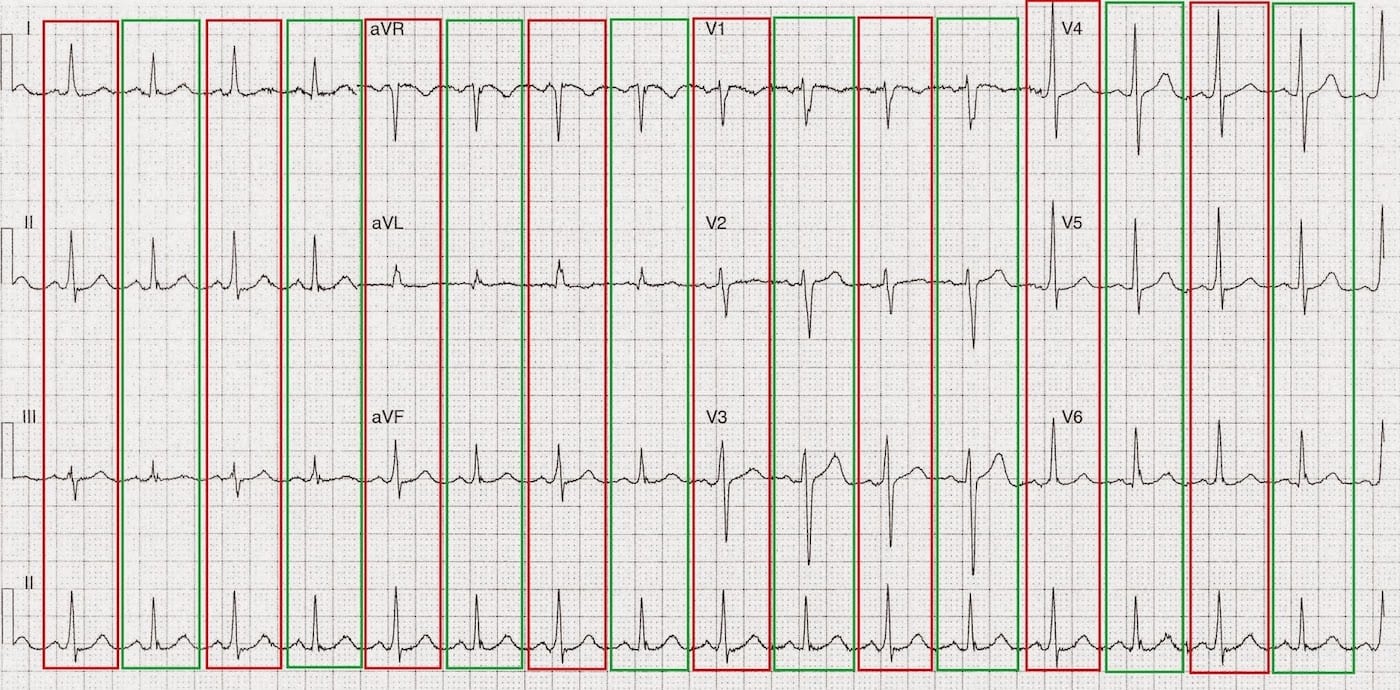
- See annotated ECG below
Axis:
- Normal
- All complexes
Intervals – QRS Complexes Labelled in Red
- PR – Short at ~110ms
- QRS – Normal at 100ms
- QT – 340ms
Intervals – QRS Complexes Labelled in Green
- PR – Normal at ~140ms
- QRS – Normal at 80ms
- QT – 320ms
Additional:
- Alternating variation in QRS voltages
- Alternating variation in T wave voltages in right precordial leads
- Subtle delta waves seen in the complexes labelled red in the right precordial and inferior leads
Interpretation:
- Alternating pre-excitation / accessory pathway conduction with sinus conduction
CLINICAL PEARLS
The EP members of our team agree this is likely a weak left sided pathway with classical intermittent pre-excitation which usually confers a benign prognosis in the setting of atrial fibrillation.
For a great overview article on pre-excitation and paroxysmal SVT check out:
- Almendrala J, Castellanosa E, Ortiza M. Paroxysmal Supraventricular Tachycardias and Preexcitation Syndromes. Rev Esp Cardiol. 2012;65:456-69.
TOP 100 ECG Series
Emergency Medicine Specialist MBChB FRCEM FACEM. Medical Education, Cardiology and Web Based Resources | @jjlarkin78 | LinkedIn |

Hi…how is it different from electrical alternans
Hi, thank you for this interesting case. I’d just like to point out that this actually is an “alternating WPW pattern” rather than an “intermittent” one. The potentially underlying mechanisms are the following:
1) Supernormal 2:1 conduction through the accessory pathway associated with phase 3 block and concealed retrograde activation of the same pathway;
2) Phase 3 bidirectional block in the accessory pathway;
3) Phase 4 unidirectional (anterograde only) block in the accessory pathway.
In the presence of relatively fast sinus rates (like in this case), the most likely mechanisms are 1) and 2), being phase 4 block associated with bradycardia.
The observation of accessory pathway conduction during higher and slower rates is critical for differentiating from supernormal 2:1 conduction and phase 3 bidirectional block in the accessory pathway.
The diagnosis of supernormal conduction is clinically relevant since this mechanism may support extremely fast ventricular responses during atrial tachyarrythmias possibly degenerating into ventricular fibrillation.