Pre-excitation syndromes
This page covers the pathophysiology and ECG features of pre-excitation syndromes in sinus rhythm. The two main forms of tachyarrhythmias that occur due to accessory pathways are discussed separately — see atrioventricular re-entry tachycardia (AVRT) and atrial fibrillation/flutter in pre-excitation.
Overview of Wolff-Parkinson-White (WPW) Syndrome
- WPW Syndrome refers to the presence of a congenital accessory pathway (AP) and episodes of tachyarrhythmias. The term is often used interchangeablely with pre-excitation syndrome
- First described in 1930 by Louis Wolff, John Parkinson and Paul Dudley White
- Incidence is 0.1 – 3.0 per 1000
- Associated with a small risk of sudden cardiac death
ECG features of WPW in sinus rhythm
- PR interval < 120ms
- Delta wave: slurring slow rise of initial portion of the QRS
- QRS prolongation > 110ms
- Discordant ST-segment and T-wave changes (i.e. in the opposite direction to the major component of the QRS complex)
- Pseudo-infarction pattern in up to 70% of patients — due to negatively deflected delta waves in inferior/anterior leads (“pseudo-Q waves”), or prominent R waves in V1-3 (mimicking posterior infarction)
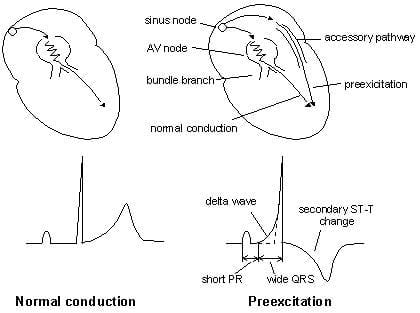
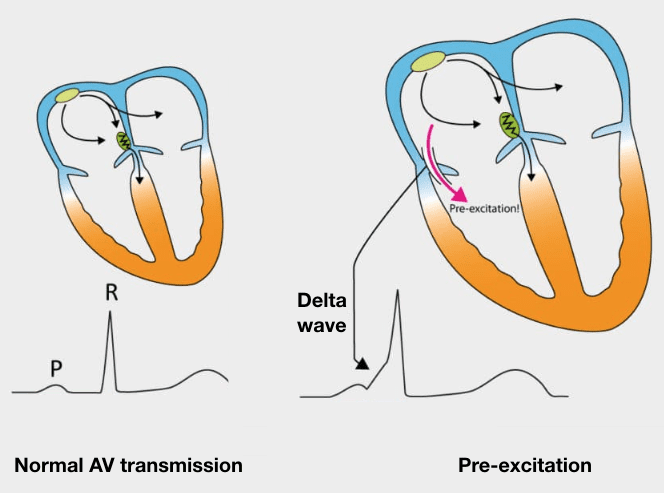
Understanding ECG changes makes them easier to recognise
- Aberrant conduction via an AP leads to early ventricular depolarisation (pre-excitation), which manifests as a short PR interval and slurred upstroke of the QRS complex
- Conduction still occurs via the AV node, and is actually a brake on AP conduction, ceasing its propagation path in the ventricle
- QRS duration is thus prolonged, but not to the same extent as in bundle branch block
- Because there is an initial abnormal direction of depolarisation (e.g. originating from left ventricle in left-sided AP), there will be an abnormal direction of repolarisation. This produces appropriately discordant ST segment and T wave changes (see above diagram)
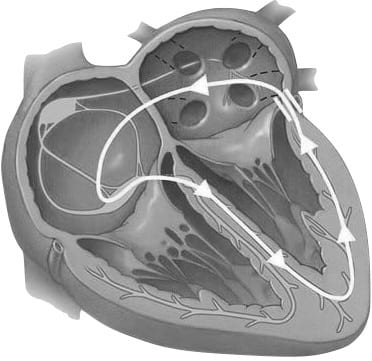
Pathophysiology of pre-excitation and APs
Pre-excitation refers to early activation of the ventricles due to impulses bypassing the AV node via an AP. Also known as bypass tracts, APs are abnormal conduction pathways formed during cardiac development and can exist in a variety of anatomical locations and in some patients there may be multiple pathways. In WPW, the AP is sometimes referred to as the Bundle of Kent, or atrioventricular bypass tract.
An AP can conduct impulses in three ways:
- In both directions (majority)
- Retrograde only, away from the ventricle (15%)
- Anterograde only, towards the ventricle (rare)
The direction of conduction affects the appearance of the ECG in sinus rhythm and during tachyarrhythmias.
APs can be left-sided or right-sided, and ECG features will vary depending on this:
- Left-sided AP: produces a positive delta wave in all precordial leads, with R/S > 1 in V1. Sometimes referred to as a type A WPW pattern
- Right-sided AP: produces a negative delta wave in leads V1 and V2. Sometimes referred to as a type B WPW pattern
Note that the features of pre-excitation may be subtle, or present only intermittently. Pre-excitation may be more pronounced with increased vagal tone e.g. during Valsalva manoeuvres, or with AV blockade e.g. drug therapy.
Concealed pathway
In patients with retrograde-only accessory conduction, all anterograde conduction occurs via the AV node. No pre-excitation occurs and therefore no features of WPW are seen on the ECG in sinus rhythm. This is termed a “concealed pathway”. These patients can still experience tachyarrhythmias, as the pathway can still form part of a re-entry circuit.
Tachyarrhythmias in WPW
There are only two main forms of tachyarrhythmias that occur in patients with WPW — these are discussed separately:
- Atrial fibrillation or flutter. Due to direct conduction from atria to ventricles via an AP, bypassing the AV node
- Atrioventricular re-entry tachycardia (AVRT). Due to formation of a re-entry circuit involving the AP
Other Pre-Excitation Syndromes / Accessory Pathways
Lown-Ganong-Levine (LGL) Syndrome
Proposed pre-excitation syndrome. AP composed of James fibres.
ECG features:
- PR interval < 120ms
- Normal QRS morphology
The term should not be used in the absence of paroxysmal tachycardia. Existence is disputed.
Mahaim-Type Pre-excitation
Right sided APs connecting either AV node to ventricles, fascicles to ventricles, or atria to fascicles.
ECG features:
- Sinus rhythm ECG may be normal
- May result in variation in ventricular morphology
- Re-entry tachycardia typically has LBBB morphology
ECG Examples
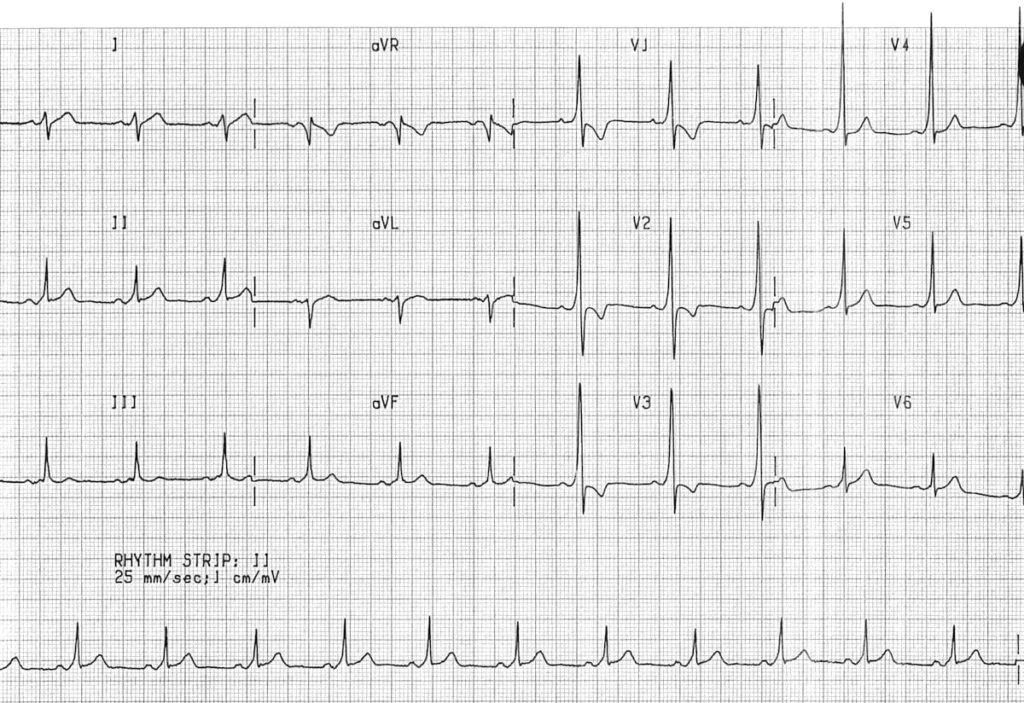
Sinus Rhythm – Type A Pattern
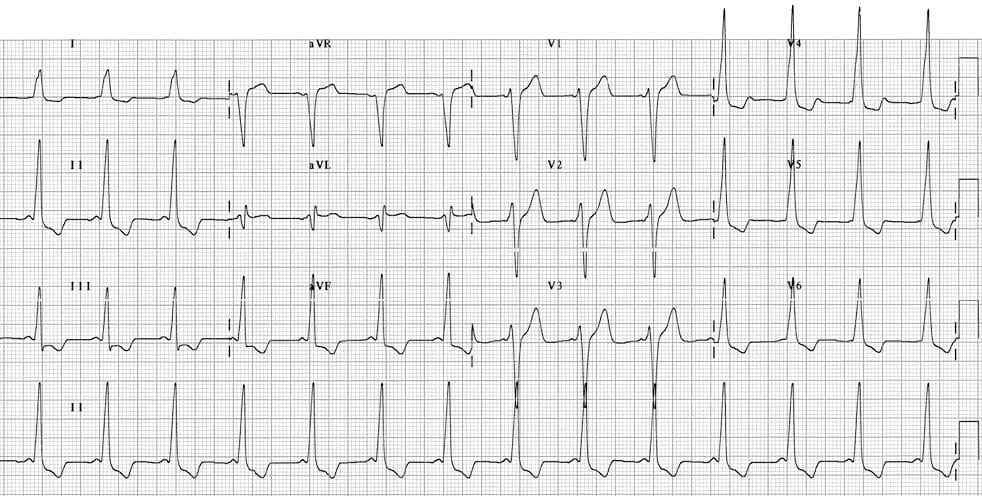
Example 1

- Sinus rhythm with a very short PR interval (< 120 ms)
- Broad QRS complexes with a slurred upstroke to the QRS complex — the delta wave
- Dominant R wave in V1 suggests a left-sided AP, and is sometimes referred to as “Type A” WPW
- Tall R waves and inverted T waves in V1-3 mimicking right ventricular hypertrophy (RVH) — these changes are due to WPW and do not indicate underlying RVH
- Negative delta wave in aVL simulating the Q waves of lateral infarction — this is referred to as the “pseudo-infarction” pattern
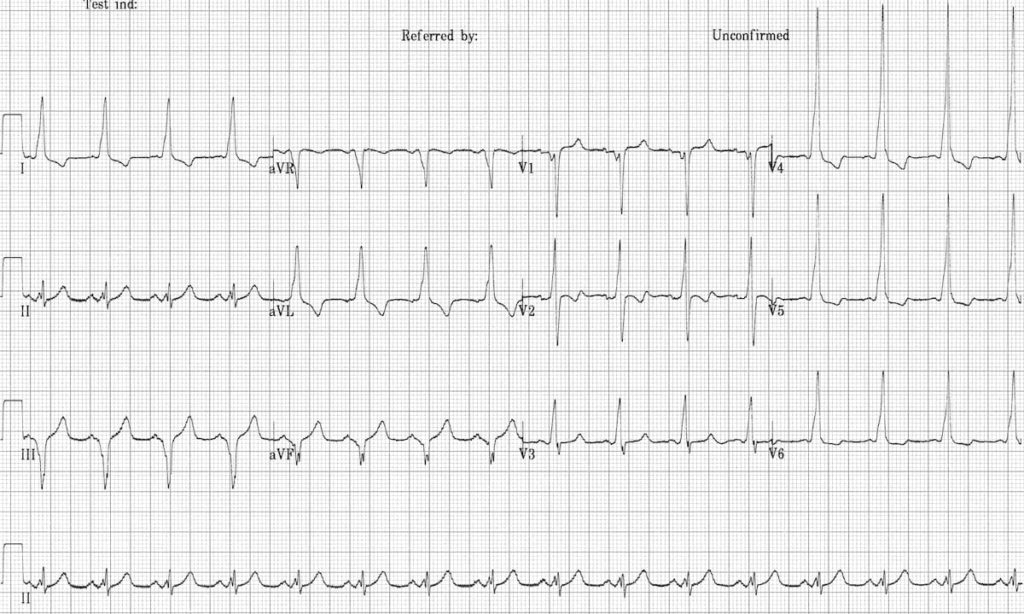
Example 2
Another example of a left-sided AP (type A WPW), with dominant R wave in V1 and right precordial T-wave inversions simulating RVH.
Sinus rhythm – Type B Pattern
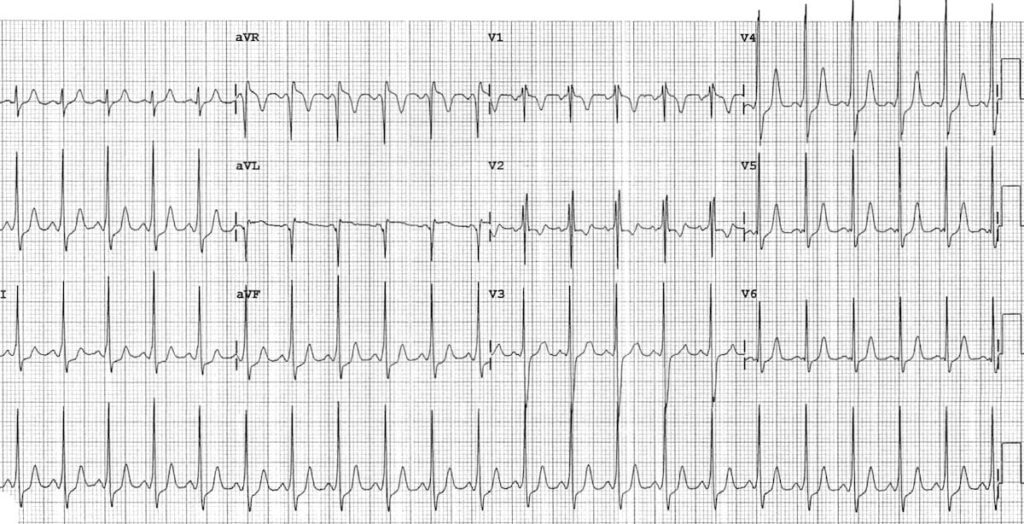
Example 3
- Sinus rhythm with very short PR interval (< 120 ms)
- Broad QRS complexes with a slurred upstroke to the QRS complexes — the delta wave
- Dominant S wave in V1 indicates a right-sided AP — sometimes referred to as “Type B” WPW
- Tall R waves and inverted T waves in the inferior leads and V4-6 mimic the appearance of left ventricular hypertrophy (LVH) — again, this is due to WPW and does not indicate underlying LVH
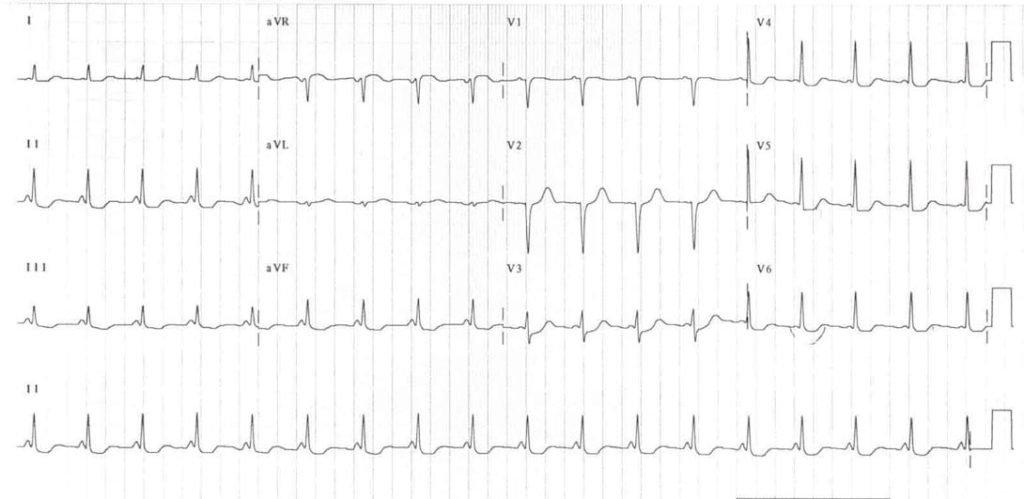
Example 4
Another example of a right-sided AP (Type B WPW):
- Negative delta waves in leads III and aVF simulate the Q waves of prior inferior MI (= pseudo-infarction pattern)
Sinus Rhythm – Paediatric ECGs
Example 5
An example of WPW in a 5-year old boy — the ECG changes are more subtle than in adults:
- The PR interval is short even allowing for the patient’s age
- The QRS complexes do not appear particularly broad — however, there is definite slurring of the upstroke of each R wave, most obvious in leads II, III, aVF and V4 (= delta waves)
- The RSR’ pattern with T wave inversion in V1-2 is a normal variant in children of this age; this is still a Type B pattern due to absence of a dominant R wave in V1
- There are pseudo-infarction Q waves in lead aVL simulating lateral infarction
For more information on interpretation of the paediatric ECG, check out our Guide to Paediatric ECG Interpretation.
Example 6

Another example of paediatric WPW, this time in a 7-year old child:
- Slight QRS widening and delta waves are more evident in the older child
- Again, there are pseudo-infarction Q waves in aVL
- It is difficult to determine if this is a left or right-sided AP, as a dominant R wave in V1 is normal for the child’s age
Lown-Ganong-Levine Syndrome
Example 7
This is a possible example of LGL syndrome:
- Very short PR interval
- Narrow QRS complexes
- No evidence of delta waves
Clinical Cases
- Top 100 ECG – Case 002
- Top 100 ECG – Case 038
- Top 100 ECG – Case 073
- Top 100 ECG – Case 092
- Top 100 ECG – Case 136
Related Topics
- Pre-excitation syndromes
- Pre-excitation with atrial fibrillation/flutter
- Atrioventricular Re-entry Tachycardia (AVRT)
- Atrioventricular Nodal Reentrant Tachycardia (AVNRT)
- Supraventricular tachycardia
- VT versus SVT with aberrancy
- ECG Medical Training – WPW Syndrome Part 1
- ECG Medical Training – WPW Syndrome Part 2
Advanced Reading
Online
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog.
- Wiesbauer F. Little Black Book of ECG Secrets. Medmastery PDF
Textbooks
- Zimmerman FH. ECG Core Curriculum. 2023
- Mattu A, Berberian J, Brady WJ. Emergency ECGs: Case-Based Review and Interpretations, 2022
- Straus DG, Schocken DD. Marriott’s Practical Electrocardiography 13e, 2021
- Brady WJ, Lipinski MJ et al. Electrocardiogram in Clinical Medicine. 1e, 2020
- Mattu A, Tabas JA, Brady WJ. Electrocardiography in Emergency, Acute, and Critical Care. 2e, 2019
- Hampton J, Adlam D. The ECG Made Practical 7e, 2019
- Kühn P, Lang C, Wiesbauer F. ECG Mastery: The Simplest Way to Learn the ECG. 2015
- Grauer K. ECG Pocket Brain (Expanded) 6e, 2014
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric 6e, 2008
- Chan TC. ECG in Emergency Medicine and Acute Care 1e, 2004
LITFL Further Reading
- ECG Library Basics – Waves, Intervals, Segments and Clinical Interpretation
- ECG A to Z by diagnosis – ECG interpretation in clinical context
- ECG Exigency and Cardiovascular Curveball – ECG Clinical Cases
- 100 ECG Quiz – Self-assessment tool for examination practice
- ECG Reference SITES and BOOKS – the best of the rest
ECG LIBRARY
Emergency Physician in Prehospital and Retrieval Medicine in Sydney, Australia. He has a passion for ECG interpretation and medical education | ECG Library |
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner


Really appreciate your superb ECG collection and explanations!
[…] Pre-excitation syndromes […]
Good to see and get knowledge about the ECG and other problem which is concern for professional