Ethanol
We are all familiar with Ethanol and maybe some of us wouldn’t have been conceived without it. However, in your tox patient it causes synergistic CNS depression and even on its own in large doses can be potentially lethal.
Toxic Mechanism:
The sites of action are varied and uncertain but it does augment the GABAa receptor complex thus causing CNS depression. It also impairs gluconeogenesis therefore can cause hypoglycaemia in susceptible individuals (children, liver patients).
Toxicokinetics:
- Rapid absorption
- Volume of distribution is low (0.6L/kg) therefore dialysis could be used.
- Ethanol is converted to acetaldehyde by alcohol dehydrogenase, then to acetate by aldehyde dehydrogenase. See Alcohol pathways. During these steps NAD is reduced to NADH which decreases the conversion of lactate to pyruvate, thus a lactic acidosis can be seen.
- Zero order kinetics apply above a serum concentration of 4 mmol/L (2 mg/dL) therefore only a constant amount is eliminated per unit time (it is not exponential). In most patients 4 mol/L/hour (20 mg/dL/hour; 0.02%/hour).
Resuscitation:
- CNS depression is the greatest risk. If there is any doubt over the patients ability to protect their own airway or you believe they are an aspiration risk they will require intubation and ventilation.
Risk Assessment
- This post concentrates on the risk assessment of ethanol per dose but do not forget these patients are at increased risk of infection (meningitis, encephalitis, pneumonia), trauma, co-ingestants, hypoglycaemia. Do not always assume there reduced GCS or behaviour is due to alcohol.
- 11 mmol/L = Disinhibition and euphoria
- 22 mmol/L = Slurred speech, impaired judgement, coordination, significant CNS depression in those non-tolerant.
- 43 mmol/L = Potential for coma, although ethanol dependent individuals can still be ambulant
- >87 mmol/L = Coma and respiratory depression, hypotension (except in those with marked tolerance)
- To convert SI units (used above) to mg/dL, multiply by 4.61. mg/dL to SI unit multiple by 0.22.
Supportive Care
- General supportive measures (i.e. IV fluids only if dehydrated), monitor for urinary retention.
- Need to observe patients with alcohol dependence for withdrawals and treat with benzodiazepines as per local guidelines.
- Thiamine 100mg TDS IV if no signs of Wernicke’s encephalopathy (Confusion, ataxia and ophthalmoplegia) otherwise 300mg TDS IV.
- If intubated see FASTHUGSINBED for further supportive care.
Investigations
- Screening: 12 lead ECG, BSL, Paracetamol level
- Specific: blood serum and breath alcohol levels.
- Remember that if the patient has CNS depression and ethanol on breath or serum testing it does not necessarily mean this is the only drug in their system or responsible for the CNS depression.
- Breath alcohol levels are an estimate, they are affected by minute ventilation.
- If there are concerns for a toxic alcohol ingestion go on to perform osmolalities and a blood gas to calculate an anion gap and osmolar gap.
Decontamination:
Activated charcoal does not bind to alcohol
Enhanced Elimination
Ethanol can be haemodialysed but the majority of patients can be managed with good supportive care.
Antidote
None available
Disposition
- Patients with mild intoxication can be managed on the ward and discharged once they are clinically well, eating and drinking, passing urine and have a safe environment to return to.
- Patients with significant CNS depression require intubation and ICU admission.
- Always counsel patients on their alcohol use (most drunk people do not end up in ED).
References and Additional Resources:
- Alcohol Toxidrome
- Alcohol withdrawal
- Chronic Alcohol Abuse
- Alcoholic Ketoacidosis
Zeff – Gas analysis and osmolar gaps
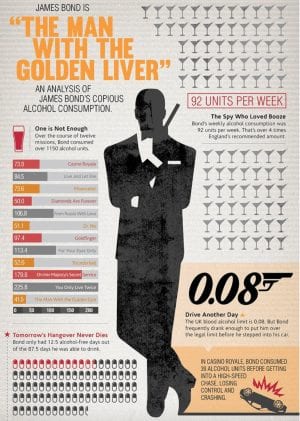
- And for something more amusing see the BMJs report on James Bond’s alcohol consumption.
References:
- Lieber CS. Medical disorders of alcoholism. New England Journal of Medicine 1995; 333(16):1058-1065
- Murray L et al. Toxicology Handbook 3rd Edition. Elsevier Australia 2015. ISBN 9780729542241
- O’Connor PG, Schottenfield RS. Patients with alcohol problems. New England Journal of Medicine 1998; 338(9):592-602
- Tiptoe AC, Taylor DMcD, Lieu H. Alcohol use among young adults presenting to the emergency department. Emergency Medicine Australasia 2006; 18(2):125-130

Toxicology Library
DRUGS and TOXICANTS
Dr Neil Long BMBS FACEM FRCEM FRCPC. Emergency Physician at Kelowna hospital, British Columbia. Loves the misery of alpine climbing and working in austere environments (namely tertiary trauma centres). Supporter of FOAMed, lifelong education and trying to find that elusive peak performance.