FFS: Cluster Headache
Cluster headache is an uncommon primary headache syndrome classified among the trigeminal autonomic cephalalgias (TACs) — a group of idiopathic disorders characterised by unilateral severe headache and associated cranial autonomic symptoms.
Cluster headache is the most prominent TAC and has been referred to as the “suicide headache” due to its extreme intensity.
The term “cluster headache” is often misused to describe migraines with cyclical attacks.
Management is similar to that of migraine, with triptans being first-line agents.
Epidemiology
- Prevalence: <1%
- Sex: More common in males
Pathophysiology
Cluster headache is classified as a neurovascular headache.
- Most accepted theory: Hypothalamic activation triggers the trigeminal-autonomic reflex, likely via a trigeminal-hypothalamic pathway.
- Stress (mental or physical) is a common precipitant.
- Rarely, structural lesions (e.g. pituitary tumours) may mimic or cause cluster headache.
- Some evidence suggests a familial or genetic component.
Clinical Features
1. Site
- Pain is centred around the orbit or temporal regions
- Strictly unilateral during each cluster period (side-shift occurs in ~15%)
2. Severity
- Typically severe, hence the term “suicide headache”
- Patients are often restless and may pace or rock
3. Duration
- Individual attacks last 15 minutes to 3 hours
- Contrasts with migraine which lasts >4 hours untreated
4. Frequency
- Attacks often occur nocturnally
- 1–8 attacks/day over 6–12 weeks
- Remission may last up to 12 months or longer
5. Autonomic Symptoms
- Unilateral autonomic dysfunction ipsilateral to the pain
- Due to parasympathetic hyperactivity and/or sympathetic impairment
- Involvement of the cavernous sinus plexus may lead to partial Horner’s syndrome
Associated features:
- Rhinorrhoea
- Lacrimation
- Conjunctival injection
- Ptosis
- Miosis
- Facial sweating
~3% of patients lack autonomic features
Chronic Cluster Headache
- Defined by no remission for ≥1 year or remission <1 month
- May be primary or evolve from episodic form (secondary chronic cluster)
Differential Diagnosis
| Condition | Differentiating Features |
|---|---|
| Migraine | Longer duration, may swap sides, photophobia common |
| Paroxysmal hemicrania | Similar features, but shorter attacks; responds to indomethacin |
| Primary stabbing headache | Brief, ice-pick like pains |
| Trigeminal neuralgia | Shock-like pain, lacks autonomic symptoms |
| Giant cell arteritis | Consider in elderly with new unilateral headache |
Investigations
No definitive diagnostic test — diagnosis is clinical and ideally confirmed by a neurologist.
Tests to exclude secondary causes:
- FBC
- ESR / CRP (especially for temporal arteritis)
- MRI Brain (with pituitary views) to exclude lesions near the sella turcica
Management
Neurologist involvement is essential.
Acute Treatment
- Oxygen
- 100% via CPAP-type mask or high-flow (15 L/min) with reservoir
- Ineffective if <100% oxygen
- Discontinue if no benefit in 20 minutes (risk of toxicity)
- Triptans
- Sumatriptan 6 mg SC or 20 mg intranasally
- Rizatriptan 10 mg orally
- Zolmitriptan 2.5 mg orally
Bridging Treatment
Used during initiation of preventive therapy:
- Prednisolone 50 mg/day for 5 days, taper by 12.5 mg every 3 days
- Naratriptan 2.5 mg orally BID for 1 week
- Greater occipital nerve block (e.g. methylprednisolone + bupivacaine or lignocaine)
- May relieve symptoms for up to 3 months
- Can be used as sole therapy for short cluster periods
Preventive Treatment
Start immediately post-diagnosis under neurologist supervision:
- Verapamil
- Topiramate
- Sodium valproate
- Gabapentin
- Melatonin (high-dose)
Refer to the Neurology Therapeutic Guidelines for detailed prescribing.
Neurosurgical Intervention
Consider in refractory, debilitating cases:
- Neuromodulation: Occipital nerve stimulation, deep brain stimulation (posterior inferior hypothalamus)
- Sphenopalatine stimulation
Appendix 1
Schematic model showing most of the putative components in cluster headache pathogenesis.
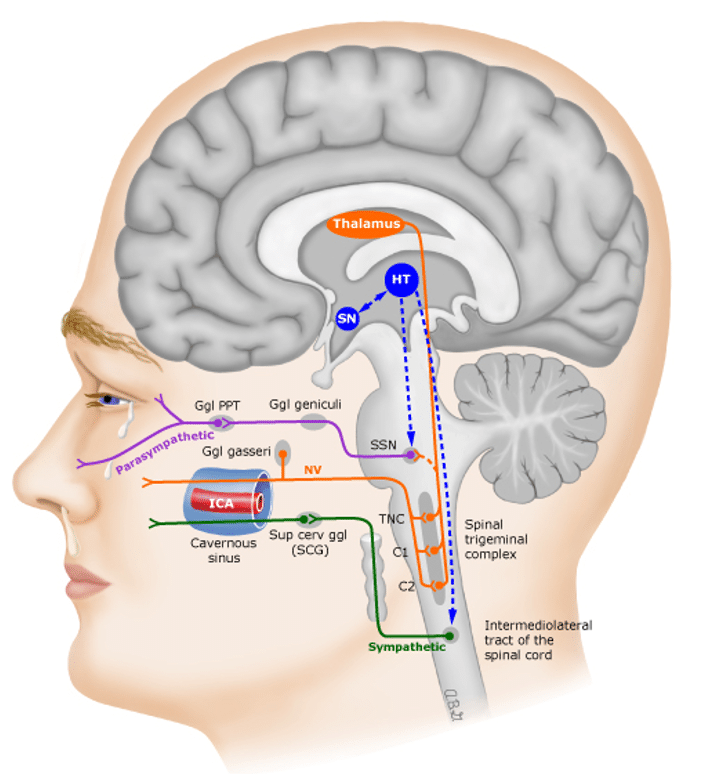
- Pain afferents from the trigeminovascular system synapse on the trigeminocervical complex (TNC), and then project to the thalamus and lead to activation in cortical areas known to be involved in pain transmission.
- Either a direct influence of the hypothalamus or a reflex activation of the parasympathetic outflow from the superior salivatory nucleus (SSN) predominately through the pterygopalatine (sphenopalatine) ganglion, leads to the parasympathetic symptoms ipsilateral to the pain.
- A third-order sympathetic nerve lesion, thought to be caused by vascular changes in the cavernous sinus loggia with subsequent irritation of the local plexus of nerve fibers, results in a partial Horner’s syndrome.
- The key site in the CNS for triggering the pain and controlling the cycling aspects is in the posterior hypothalamic grey matter region.
References
Publications
- Brazis PW, Masdeu JC, Biller J. Localization in Clinical Neurology. 8e 2021
- Fuller G. Neurological Examination Made Easy. 6e 2019
FOAMed
- Coni R. Cluster headache. LITFL
- Coni R. Headache classification. LITFL
- Coni R. Headache Essentials. LITFL
Fellowship Notes
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner
Educator, magister, munus exemplar, dicata in agro subitis medicina et discrimine cura | FFS |


