FFS: Trigeminal neuralgia
Trigeminal neuralgia (also occasionally known as tic douloureux) is a disabling syndrome characterised by neuropathic facial pain which is sudden, brief, severe and recurrent.
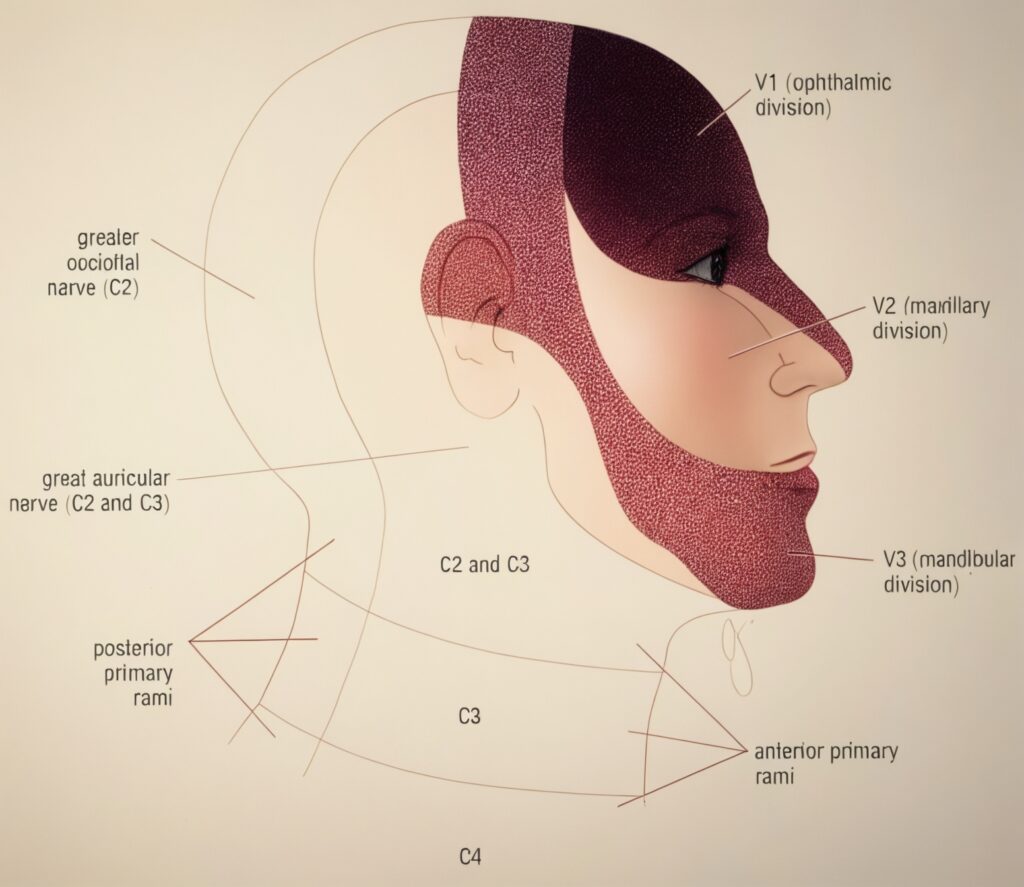
Trigeminal neuralgia involves the unilateral distribution of one or more branches of the fifth cranial (trigeminal) nerve. It may be classic (primary/idiopathic) or secondary to an identifiable underlying cause.
Treatment includes antineuralgic medications, addressing the underlying cause, or surgical options.
History
In 1756, French surgeon, Nicolas André (1704- vers 1780) coined the term tic douloureux, proposing that the pain arose from compression of sensory peripheral nerves. Using early scientific methods, he attempted to reproduce the pain by compressing nerves with tweezers and treated it with caustic mercury solution, mistakenly believing he was removing adhesions and preventing recurrence by keeping the wound open.
Epidemiology
Most commonly affects older patients, typically over 55 years.
Pathophysiology
The mechanism of pain remains unclear in many cases. Multiple pathologies may be involved.
Causes include:
1. Classic (primary/idiopathic):
- No lesion identified.
2. Secondary:
Lesions irritating the trigeminal nerve roots near the pons, including:
- Tumours
- Chronic meningeal inflammation
- Vascular causes: aneurysms, or abnormal vessel courses (e.g. superior cerebellar artery)
- Focal demyelination, e.g. multiple sclerosis (MS)
Clinical features
History
1. Pain characteristics:
- Unilateral distribution of one or more trigeminal nerve branches
- Sudden, brief (seconds to 2 minutes), severe, and recurrent
- Described as stabbing or like an electric shock
- Does not usually awaken from sleep
- Possible residual ache, but persistent full-intensity pain suggests alternate diagnoses
- Attacks are often stereotyped in individual patients
2. Trigger factors:
- Pain may be spontaneous or triggered by trivial stimuli:
- Light touch
- Wind on face
- Talking, chewing, brushing teeth
- Specific trigger point may be identified, often intraoral (e.g. gingivae)
3. Sensory findings:
- No sensory loss in painful region
4. Course:
- Attacks may remit for weeks to months and recur
Examination
- Normal neurologic exam unless an underlying lesion is present
Differential diagnosis
- Multiple sclerosis — particularly in young patients (<40 years)
- Herpes zoster (early phase or postherpetic neuralgia)
- Giant cell arteritis — must be considered in the elderly
Investigations
MRI is essential to exclude:
- Demyelination
- Mass lesions (e.g. cerebellopontine angle)
- Vascular compression
MRI should be prioritised if there are atypical features, especially sensory loss.
Management
1. Carbamazepine (first-line):
- Begin at 100 mg controlled-release, orally once or twice daily
- Titrate weekly as tolerated, up to 600 mg twice daily
- Once controlled, reduce dose gradually to the minimum effective dose
2. Other agents:
Consider if carbamazepine fails:
- Baclofen
- Clonazepam
- Gabapentin
- Lamotrigine
- Oxcarbazepine
- Phenytoin
- Sodium valproate
Note: Amitriptyline is usually ineffective for trigeminal neuralgia.
3. Surgery:
Consider if symptoms are refractory or due to compressive lesion:
- Microvascular decompression (invasive but potentially curative)
- Thermocoagulation or radiofrequency rhizotomy
- Stereotactic radiotherapy (e.g. gamma knife)
Disposition
- All patients should be referred to a neurologist
- Neurosurgical input required for refractory cases or confirmed structural causes
References
Publications
- André NA. Observations pratiques sur les maladies de l’urèthre Paris. 1756
- Govoni V, Granieri E, Menini C. The history of the tic douloureux: autopathograph of an Italian lawyer who suffered from trigeminal neuralgia from 1803 to 1824. J Hist Neurosci. 1996 Aug;5(2):169-89.
- Brown JA, Coursaget C, Preul MC, Sangvai D. Mercury water and cauterizing stones: Nicolas André and tic douloureux. J Neurosurg. 1999 May;90(5):977-81.
- Shankar Kikkeri N, Nagalli S. Trigeminal Neuralgia. 2024 Mar 3. In: StatPearls
FOAMed
- Coni R. Cranial neuralgias. LITFL
- Hayes J. FFS: Headache – Neuralgic Chart. LITFL
Fellowship Notes
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner
Educator, magister, munus exemplar, dicata in agro subitis medicina et discrimine cura | FFS |


